Mini Review Open Access
Role of Palliative Radiotherapy for Bone Metastasis
Takeo Takahashi1*, Keiichiro Nishimura1, Takafumi Yamano1 and Masatoshi Gika21Department of Radiation Oncology, Saitama Medical Center, Saitama Medical University, Japan
2Palliative Care Team, Saitama Medical Center, Saitama Medical University, Japan
- *Corresponding Author:
- Takeo Takahashi
Department of Radiation Oncology, Saitama Medical Center
Saitama Medical University, Japan
Tel: +81-49-228-3441
Fax: +81-49-228-3753
E-mail: taketaka@saitama-med.ac.jp
Received date December 30, 2013; Accepted date February 22, 2014; Published date February 28, 2014
Citation: Takahashi T, Nishimura K, Yamano T, Gika M (2014) Role of Palliative Radiotherapy for Bone Metastasis. J Palliat Care Med 4: 171. doi:10.4172/2165-7386.1000171
Copyright: © 2014 Takahashi T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Introduction
With approximately 50-70% of patients with advanced cancer developing bone metastases during the course of their disease, treatment of bone metastases depends on many factors including performance status, pathology, site of disease, and neurologic status [1]. Radiotherapy has become highly precise, improving local control and facilitating minimally invasive treatment, and has attracted attention as a curative treatment method comparable to surgery. On the other hand, radiotherapy also plays an extremely important role in palliative treatment for advanced cancer patients [2]. Palliative care and treatment is aimed at providing relief from pain and other symptoms. Curative and palliative radiotherapies differ in the radiation field size, dose fraction, and treatment schedule. We review the role of radiotherapy in palliative treatment for patients with symptomatic bone metastases.
Characteristics of Palliative Radiotherapy
Palliative radiotherapy usually reduces pain symptoms caused by bone metastases after a short treatment schedule. Since palliative radiotherapy is localized to the tumor lesion in most cases, adverse effects are generally mild, and this therapy is indicated even in patients with a poor general condition. After radiotherapy, improvement in not only tumor related symptoms but also the patient’s quality of life (QOL) is expected [3,4]. Bone metastases represent the most common indication for palliative radiotherapy. Radiotherapy, whose treatment method is different from analgesic or bisphosphonate administration, is localized to the lesion responsible for pain, and can also provide tumor reduction and local tumor control.
Radiotherapy for Painful Bone Metastasis
Bone metastasis is a common and severe complication in advanced cancer. The major complications associated with bone metastases are severe pain, spinal cord compression, and pathological fracture. These complications restrict mobility and great reducing patient’s activity of daily living and QOL. Radiotherapy for bone metastasis is classified into external beam radiotherapy as a local treatment and radionuclide therapy as a systemic therapy. Radiotherapy has been established as an effective treatment for symptomatic bone metastases. Treatment of bone metastasis is mainly palliative and the aims of palliative radiotherapy for bone metastasis are: 1) pain relief, 2) improvement in symptoms due to metastatic spinal cord compression, and 3) prevention of imminent fractures.
Pain-relief effects of external beam radiotherapy (EBRT)
Although various fractionation schedule of EBRT may provide good rates of palliation, common fractionation schedules include 8-Gy single fraction, 20 Gy in five fractions, and 30 Gy in 10 fractions [1,5,6]. Single and multifractions regimen provided equal pain relief [7], and 8-Gy single fraction is a standard treatment [1,5]. A clinical trial (RTOG 7402) performed in the U.S. in the 1970s showed the effectiveness of palliative radiotherapy [8]: Overall, 89% experienced at least minimal relief of pain, with 83% obtaining partial relief and 53% obtaining complete pain relief. In this clinical trial, pain-relieving effects did not differ among dose fraction schedules, showing no dose-dependence of the pain-relieving effects. A randomized phase III controlled study (RTOG 97-14) showed similar pain-relieving effects between 30 Gy in 10 fractions and 8 Gy in a single fraction [9]. However, the single-fraction group more frequently required re-irradiation. Many subsequent randomized clinical trials comparing multiple fractions and a single fraction of 8 Gy have shown similar pain-relieving effects on painful bone metastasis [9-14] (Table 1). A recent meta-analysis reported that single fraction and multiple fractions provided overall pain response for 60% and 61% of patients respectively [7].
| Study | Primary Site | RT Schedule | N | Pain Relief |
|---|---|---|---|---|
| Bone Pain Trail | Breast, Prostate | 8 Gy/F | 383 | 78% |
| Working Party Study[10] | Lung | 20 Gy/ 5F, 30 Gy/10F | 378 | 78% |
| Trans-Tasman | Breast, lung | 8 Gy/F | 272 | 53% |
| Radiation Oncology Group[11] | Prostate | 20 Gy/ 5F | 272 | 61% |
| Ducth Bone | Breast, Prostate | 8 Gy/F | 579 | 71% |
| Metastasis Study[12] | Lung, Other | 24 Gy/6F | 578 | 73% |
| Radiation Therapy | Breast, prostate | 8 Gy/F | 455 | 65% |
| Oncology Grouap 97-14[9] | 30 Gy/10F | 443 | 66% | |
| Norway and Sweden[13] | Breast, prostate | 8 Gy/F | 186 | No difference |
| Lung, other | 30 Gy/10F | 190 | (QOL) |
Table 1: Randomized trial for painful bone metastasis.
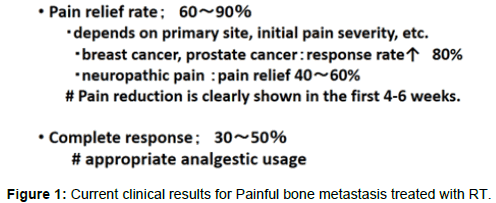
EBRT produces significant reduction of pain caused by bone metastases in 60-90%, with complete pain relief in 30 to 50% of patients, although the effects differ according to the primary lesion and severity of pain when treatment is initiated [9,15] (Figure 1). In particular, relief of pain is observed in about 80% of patients with breast cancer or prostatic cancer. However, in patients with neuropathic pain, the pain-relieving effects of opioids are slight, and those of radiotherapy are observed only in 40-60% [11,16]. The Dutch Bone Metastases Study Group presented that re-irradiation of painful bone metastasis was effective and retreatment response was 63%. Of patients in whom re-irradiation can be performed, 50-70% show pain-relieving effects [17]. The indications for re-irradiation are determined based on the previously applied dose and interval following prior radiotherapy. Re-irradiation is performed so that the total dose will not exceed that tolerated by organs at risk, such as the spinal cord and brainstem. Stereotactic body radiotherapy (SBRT) is expected to be useful for cases with vertebral metastasis because SBRT allows the shaped dose distribution sparing the spinal cord from high irradiation dose. Especially, SBRT might also be used when re-irradiation is required in previously irradiated sites.
In the presence of single bone metastasis, when the primary lesion is controlled, and the prognosis is favorable, treatment aiming at long-term symptom control is also considered [18-20]. Randomized controlled clinical trials have shown no dose dependence of painrelieving effects but higher incidences of re-irradiation rate after singlefraction than after multiple-fraction radiotherapy. The Dutch trial presented the rate of retreatment and fracture was higher in the 8-Gy single fraction group compared than in 30 Gy multifraction group. A systematic review showed that the risk of pathological fracture was not significantly different between single fraction and multiple fraction arms [7]. The local recurrence rate was reported to be low in a longcourse radiotherapy group [20].
Radiotherapy for metastatic spinal cord compression
In the presence of spinal cord metastasis, an increase in the tumor size causes spinal cord compression, and the resulting paraplegia markedly decreases the patient’s QOL. When symptoms of paraplegia develop, appropriate management within 48 hours is necessary. After radiotherapy, the motor function improves in about 40%. When treatment can be initiated while patients can still walk, 80% of them can maintain walking. In patients with paraplegia due to spinal cord compression, the paraplegia improvement rate after radiotherapy is only 7% [21]. Local control is more favorable after long-course than short-course radiotherapy [22]. The prognosis (local control) depends on the location of the primary lesion, presence or absence of visceral metastasis, and the radiotherapy schedule (dose fraction schedule) [22]. Prognositic factors were favorable histology, absence of other bone metastases, absence of visceral metastases, being ambulatory before radiotherapy, a slower development of motor deficits before radiotherapy, and a longer interval between tumor diagnosis and MSCC [22]. For spinal cord compression due to oligometastasis, the local control rates were reported to be 92, 88, and 78% after 1, 2, and 3 years, respectively, showing favorable outcomes [23]. In particular, the prognosis is more favorable when the progression of paraplegia is slower, and the symptoms of paraplegia are milder. Therefore, for metastatic spinal cord compression, the standard treatment may be long-course radiotherapy (30 Gy/10 fractions or 40 Gy/20 fractions) combined with steroid therapy. In particular, in patients in whom survival for at least 6 months is expected, long-course radiotherapy is recommended [6]. A recent matched pair analysis showed no difference in treatment results between the two methods. However, the only randomized clinical trial that compared the effects on spinal cord compression due to spinal cord metastasis between surgery combined with postoperative radiotherapy and radiotherapy alone showed the effectiveness of surgery [24,25]. A systematic review demonstrated that surgery should be considered for operable MSCC patients with a good progonosis [26]. Radiotherapy should be performed for nonsurgical MSCC peitens; For those with a poor prognosis, 8 Gy in single fraction should be given, and for those with a good prognosis, 30 Gy in 10 fractions could be considered [26].
Prevention of imminent fractures
In general, bone metastasis is frequently osteolytic, and its progression causes pathological fracture. After radiotherapy for osteolytic bone metastasis, recalcification is observed in 65-85%. After radiotherapy combined with bisphosphonate administration, recalcification is observed in more than 80%. However, there is no definite evidence that pathological fracture can be prevented by recalcification after radiotherapy. On the other hand, although stereotactic body radiotherapy precisely delivers high dose to the tumor volume, it has a risk of long term vertebral compression fracture.
Relationship Between Prognositic Factors and Radiotherapy Schedule
To estimate the survival of patients with bone metastasis, some scoring systems for survival have been used, and their usefulness has been reported for predicting prognosis of patients with bone metastasis. It is important to select appropriate treatment methods and radiotherapy dose fraction schedules according to the prognosis of patients with bone metastasis [27]. Single-fraction radiotherapy is advantageous for bone metastases patients with a short life expectancy. Fractionated regimen, such as 30 Gy in 10 fractions, 35 Gy in 14 fractions, or 40 Gy in 20 fractions, are favoured for patients with long life expectancy [1].
Radiopharmaceutical Therapy
Radiopharmaceutical therapies are utilized in palliation of painful bone metastases, and recommended for multiple osteoblastic skeletal metastases with pain symptoms [5,28]. Single intravenous administration of β-emitting agents including strontium-89 and samarium-153 can relieve pain in widespread bone metastases. The following conditions should be fulfilled for the use of strontium-89 therapy: (1) Bone scintigraphy shows accumulation at the site of metastasis. (2) The bone marrow function is maintained. (3) The life expectancy is at least 1 month. Pain relief is obtained due to the cytocidal effects of β-rays emitted by strontium (89Sr). Basically, the main effect of this agent is the alleviation of symptoms, and improvement in pain and a reduction in the analgesic dose are achieved in about 50% of patients. Its adverse effects are myelosuppression and the flare phenomenon. Sr- 89 therapy can also be combined with bisphosphonate administration or radiotherapy. Radium-223 is a bone-seeking an alpha emitter, and a new agent for bone metastases from prostate cancer. A phase III trial has showed that Radium-223 improved overall survival significantly for patients with metastatic prostate cancer [29]. It is a promising candidate for managing bone metastases of castration-resistant prostate cancer.
Role of Highly Precise Radiotherapy for Bone Metastasis
Intensity-modulated radiotherapy (IMRT) has facilitated highly precise irradiation localized to the tumor, and favorable treatment results have been reported for prostatic and lung cancer. SBRT implies one to hypo fractionated radiotherapy, and delivers high biological effectiveness doses to metastatic spine disease with a steep dose gradient, thereby sparing adjacent critical organs. The role of SBRT in the management of spinal oligometastasis, radioresistant spinal metastasis, and previously irradiated but progressive spinal metastasis are emerging [1]. The usefulness of highly precise radiotherapy for bone metastasis is also expected in terms of local control [30]. Re-irradiation is possible in most of cases with bone metastasis due to these modern irradiation technique. However, target delineation, total dose, and fractionation schedule have not to be fully defined. These highly precise radiotherapies for bone metastases are still under clinical trials.
Conclusion
Palliative radiotherapy for bone metastases is of significant benefit to patients with painful bone metastasis and metastatic spinal cord compression. Radiotherapy plays an important role in palliative care and treatment for patients with symptomatic bone metastases.
References
- Expert Panel on Radiation Oncology-Bone Metastases, Lo SS, Lutz ST, Chang EL, Galanopoulos N, et al. (2013) ACR Appropriateness Criteria ® spinal bone metastases. J Palliat Med 16: 9-19.
- Berger AM, Shuster JL, Von Roenn JH (2007) Principles and practice of palliative care and supportive oncology.Lippincott Williams & Wilkins.
- Takahashi T, Hondo M, Nishimura K, Kitani A, Yamano T, et al. (2008) Evaluation of quality of life and psychological response in cancer patients treated with radiotherapy. Radiat Med 26: 396-401.
- Caissie A, Zeng L, Nguyen J, Zhang L, Jon F, et al. (2012) Assessment of health-related quality of life with the European Organization for Research and Treatment of Cancer QLQ-C15-PAL after palliative radiotherapy of bone metastases. ClinOncol (R CollRadiol) 24: 125-133.
- Lutz S, Berk L, Chang E, Chow E, Hahn C, et al. (2011) Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. Int J RadiatOncolBiolPhys 79: 965-976.
- Feyer PC, Steingraeber M (2012) Radiotherapy of Bone Metastasis in Breast Cancer Patients - Current Approaches. Breast Care (Basel) 7: 108-112.
- Chow E, Zeng L, Salvo N, Dennis K, Tsao M, et al. (2012) Update on the systematic review of palliative radiotherapy trials for bone metastases. ClinOncol (R CollRadiol) 24: 112-124.
- Tong D, Gillick L, Hendrickson FR (1982) The palliation of symptomatic osseous metastases: final results of the Study by the Radiation Therapy Oncology Group. Cancer 50: 893-899.
- Hartsell WF, Scott CB, Bruner DW, Scarantino CW, Ivker RA, et al. (2005) Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J Natl Cancer Inst 97: 798-804.
- (1999) 8 Gy single fraction radiotherapy for the treatment of metastatic skeletal pain: randomised comparison with a multifraction schedule over 12 months of patient follow-up. RadiotherOncol 52: 111-121.
- Roos DE, Turner SL, O'Brien PC, Smith JG, Spry NA, et al. (2005) Randomized trial of 8 Gy in 1 versus 20 Gy in 5 fractions of radiotherapy for neuropathic pain due to bone metastases (Trans-Tasman Radiation Oncology Group, TROG 96.05). RadiotherOncol 75: 54-63.
- van der Linden YM, Lok JJ, Steenland E, Martijn H, van Houwelingen H, et al. (2004) Single fraction radiotherapy is efficacious: a further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J RadiatOncolBiolPhys 59: 528-537.
- Kaasa S, Brenne E, Lund JA, Fayers P, Falkmer U, et al. (2006) Prospective randomised multicenter trial on single fraction radiotherapy (8 Gy x 1) versus multiple fractions (3 Gy x 10) in the treatment of painful bone metastases. RadiotherOncol 79: 278-284.
- Wu JS, Wong R, Johnston M, Bezjak A, Whelan T; Cancer Care Ontario Practice Guidelines Initiative Supportive Care Group (2003) Meta-analysis of dose-fractionation radiotherapy trials for the palliation of painful bone metastases. Int J RadiatOncolBiolPhys 55: 594-605.
- Chow E, Wong R, Hruby G, Connolly R, Franssen E, et al. (2001) Prospective patient-based assessment of effectiveness of palliative radiotherapy for bone metastases. RadiotherOncol 61: 77-82.
- Roos DE, O'Brien PC, Smith JG, Spry NA, Hoskin PJ, et al. (2000) A role for radiotherapy in neuropathic bone pain: preliminary response rates from a prospective trial (Trans-tasman radiation oncology group, TROG 96.05) Int J RadiatOncolBiolPhys 46: 975-981.
- Hayashi S, Hoshi H, Iida T (2002) Reirradiation with local-field radiotherapy for painful bone metastases. Radiat Med 20: 231-236.
- Ratanatharathorn V, Powers WE, Moss WT, Perez CA (1999) Bone metastasis: review and critical analysis of random allocation trials of local field treatment. Int J RadiatOncolBiolPhys 44: 1-18.
- Blitzer PH (1985) Reanalysis of the RTOG study of the palliation of symptomatic osseous metastasis. Cancer 55: 1468-1472.
- Rose CM, Kagan AR (1998) The final report of the expert panel for the radiation oncology bone metastasis work group of the American College of Radiology. Int J RadiatOncolBiolPhys 40: 1117-1124.
- Loblaw DA, Laperriere NJ (1998) Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 16: 1613-1624.
- Rades D, Fehlauer F, Schulte R, Veninga T, Stalpers LJ, et al. (2006) Prognostic factors for local control and survival after radiotherapy of metastatic spinal cord compression. J Clin Oncol 24: 3388-3393.
- Rades D, Veninga T, Stalpers LJ, Basic H, Rudat V, et al. (2007) Outcome after radiotherapy alone for metastatic spinal cord compression in patients with oligometastases. J Clin Oncol 25: 50-56.
- Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, et al. (2005) Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: a randomised trial. Lancet 366: 643-648.
- Rades D, Huttenlocher S, Dunst J, Bajrovic A, Karstens JH, et al. (2010) Matched pair analysis comparing surgery followed by radiotherapy and radiotherapy alone for metastatic spinal cord compression. J Clin Oncol 28: 3597-3604.
- Loblaw DA, Mitera G, Ford M, Laperriere NJ (2012) A 2011 updated systematic review and clinical practice guideline for the management of malignant extradural spinal cord compression. Int J RadiatOncolBiolPhys 84: 312-317.
- Mizumoto M, Harada H, Asakura H, Hashimoto T, Furutani K, et al. (2008) Prognostic factors and a scoring system for survival after radiotherapy for metastases to the spinal column: a review of 544 patients at Shizuoka Cancer Center Hospital. Cancer 113: 2816-2822.
- Kraeber-Bodéré F, Campion L, Rousseau C, Bourdin S, Chatal JF, et al. (2000) Treatment of bone metastases of prostate cancer with strontium-89 chloride: efficacy in relation to the degree of bone involvement. Eur J Nucl Med 27: 1487-1493.
- Parker C, Nilsson S, Heinrich D, Helle SI, O'Sullivan JM, et al. (2013) Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med 369: 213-223.
- Gerszten PC, Burton SA, Welch WC, Brufsky AM, Lembersky BC, et al. (2005) Single-fraction radiosurgery for the treatment of spinal breast metastases. Cancer 104: 2244-2254.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14915
- [From(publication date):
February-2014 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10209
- PDF downloads : 4706