Role of Negative Suction Subcutaneous Drains in Contaminated Abdominal Surgeries
Received: 11-Dec-2018 / Accepted Date: 23-Dec-2018 / Published Date: 03-Jan-2019 DOI: 10.4172/2161-069X.1000587
Abstract
Wounds and their management are fundamental to the practice of surgery. In any elective surgery or in the surgery of trauma, the surgeon’s task is to minimize the adverse effects of the wound, remove or repair damaged structures and enhance the process of wound healing to restore function. Because of unavoidable contamination of wounds that occurs at the time of surgery, surgeons have used a number of methods of wound management. Use of subcutaneous drains at the site of surgery is one of them. The study was carried out prospectively on patients of contaminated abdominal surgeries to assess the role of placement of negative suction drains in wounds subcutaneously on the incidence of incisional Surgical Site Infections (SSIs). This study was a prospective, open and comparative cohort study. Patients were divided into two groups by random sampling. Total sample size was 300 patients with 150 in each group. Subcutaneous suction drains were inserted in one group (cases) and no drains were inserted in another group (control). The results from the present study show that use of negative suction drain in subcutaneous = plane during laparotomy for class III wounds reduces the incidence of postoperative surgical site of infection, seroma formation and wound dehiscence. It was concluded that insertion of subcutaneous suction drains at the end of operation could provide effective drainage of the wound collections and wound seroma, thereby preventing SSI and wound dehiscence.
Keywords: Subcutaneous drain; Seroma; Surgical site infection; Diabetes; Sepsis
Introduction
Wounds and their management are fundamental to the practice of surgery. Wound seromas, infections and wound dehiscence are the commonest complications of the wounds. Wound seromas are collections of serum and lymph that becomes symptomatic or clinically apparent after operations in which subcutaneous lymphatic channels are disrupted. Abdominal wound dehiscence is one of the complications after abdominal surgery; wound dehiscence is the parting of the layers of a surgical wound. Either the surface layers separate (wound gap) or the whole wound splits open. Primary cause of wound dehiscence is infection and seroma formation. Wound infection referred to as Surgical Site Infection (SSI) by the Centre for Disease Control and Prevention is the most common nosocomial infection in surgical patients and account for 38% of all such infections [1]. Postoperative wound infections are the major source of infectious morbidity in surgical patients. Development of a surgical site infection has a large impact on mortality and morbidity as well as healthcare costs, patient inconvenience and dissatisfaction [2,3]. In any elective surgery or in the surgery of trauma, the surgeons’ task is to minimize the adverse effects of the wound, remove or repair damaged structures and enhance the process of wound healing to restore function. Because of unavoidable contamination of wounds that occurs at the time of surgery, surgeons have used a number of methods of wound management. Use of subcutaneous drains at the site of surgery is one of them. The rationale of placement of subcutaneous drains is theoretical and is based on the premise that the removal of any collecting serum or debris and elimination of dead space would perhaps result in lower rate of wound complications. Their use is effective in reducing the incidence of incisional SSI not only because of the continuous suction of the subcutaneous effusion, hematoma and bacteria but also because of reduction in the dead space of the subcutaneous wound area. In contrast to passive (open) drains, Closed-suction Drains (CSDs) establish a pressure gradient between the wound and the external environment and empty into a sealed reservoir, and are believed to reduce the risk of retrograde microbial contamination [4].
Using subcutaneous wound drainage after laparotomy in all patients is unnecessary as it does not reduce SSI risk. Similarly, there seems to be no benefit in using it in clean and clean contaminated wounds. However, there may be benefit in using drains in patients who are at high risk, including patients who are obese and/or have contaminated wound types. A well designed trial is needed which would examine these factors [5]. Studies on prevention of incisional SSI in surgical wounds classified as III or IV based on the US Center for Disease Control and Prevention (CDC) classifications are very few [6]. Such wounds are at high risk for infection. This study was undertaken to study the effect of negative suction drains on surgical wounds classified as class III based on the US Center for Disease Control and Prevention (CDC) classifications.
Materials and Methods
The study included patients admitted in the department of General and Minimal Access Surgery, Sher-i-Kashmir Institute of Medical Sciences (SKIMS) Srinagar. This study was a prospective, open and comparative cohort study with controls in order to assess the use of suction drains (active drains). The study was carried out prospectively on patients of contaminated abdominal surgeries:
• To know any role of placement of negative suction drains in wounds subcutaneously.
• To assess the role of placement of negative suction drains in wounds subcutaneously on the incidence of incisional SSIs.
Patients were divided into two groups by random sampling. Total sample size was 300 patients with 150 in each group. Subcutaneous Suction drains were inserted in one group (cases) and no drains were inserted in another group (controls). All laparotomy incisions performed at SKIMS Soura, in the age groups of 16 and 75 years, of either sex were included in the study. Among these patients only those patients with contaminated abdominal surgeries (class III) were included in the study. The patients were randomized to two groups. The first patient was put in the study group and the following in the control group. Prophylactic antibiotics were given to both groups of patients. The patients <16 years and >75 years, all the immunocompromised patients including patients on steroid therapy, patients with associated factors like diabetes, hypertension, bronchial asthma, tuberculosis, sepsis elsewhere, radiotherapy, hepatic insufficiency or renal insufficiency, patients who were in shock at the time of presentation, patients requiring ileostomy for surgical reasons or death of the patients in the postoperative period due to systemic cause were excluded from the study. Accidental removal of the drain was also excluded from the study. The incision was made by scalpel only. Wound closure technique was uniform in all of the patients. A closed drainage system for subcutaneous tissue was used through a separate stab incision. Drains were kept in place for two days. All the patients were examined and evaluated postoperatively for detection of wound seromas, SSIs and wound dehiscence. All participants were followed in outpatient department at regular intervals for about a month. They were evaluated throughout for wound healing and any complications. The diagnosis of seroma was made on a clinical basis in patients having serous discharge or soft fluctuant bulge in the wound which on aspiration revealed serous fluid. SSI cases were diagnosed within 30 postoperative day by ICT (Information and Communications Technology) according to the Centers for Disease Control and Prevention (CDC) criteria [1]: (1) Purulent drainage with or without laboratory confirmation from the superficial incision; (2) Organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision; (3) At least one of the following signs or symptoms of infection: pain or tenderness, localized swelling, redness, or heat and superficial incision were deliberately opened by surgeon, unless the incision was culture-negative; and (4) Diagnosis of s-SSI by the surgeon or ICT. Wound dehiscence is the parting of the layers of a surgical wound. Either the surface layers separate (wound gap) or the whole wound splits open. All patients who developed seroma underwent drainage through the main wound followed by regular antiseptic dressings. Wound dehiscence having only wound gap small in size was treated with regular dressing and healed itself. Wound dehiscence which was deep, regular dressing and debridement of infected part and after granulation tissue formation secondary suturing was done. SSIs were treated with regular dressings, debridement, if needed and systemic antibiotics as per the culture sensitivity.
Statistical methods
Statistical Software SPSS (Version 21.0) was used to carry out the statistical analysis of data. Continuous variables were summarized as Mean ± SD and categorical variables as percentages. Student’s independent t-test was employed for parametric data. Chi-square testor Fisher’s exact t-test, whichever appropriate, was used for categorical data. Graphically the data was presented by bar diagrams. A p-value of less than 0.05 was considered statistically significant. All p-values were two tailed.
Observations and Results
The two groups were comparable with respect to age, gender, type of surgery, nature of surgery, subcutaneous fat thickness, pre-operative serum albumin levels, presence of obesity, type of disease and type of incision. There was no statistically significant difference between cases and controls viz. above parameters. SSI was present in 15.3% of cases and 30% of controls and the difference was statistically significant (p value=0.002). 14.7% of cases and 50% of controls developed seroma and the difference was statistically significant (p value <0.001). 12% of the cases and 45.3% of the controls developed wound dehiscence and the difference was statistically significant (p value <0.001) (Table 1).
| SSI | Cases % (no.) | Control % (no.) | p value |
|---|---|---|---|
| Present | 15.3 (23) | 30 (45) | 0.002* |
| Absent | 84.7 (127) | 70 (105) | |
| Total | 100 (150) | 100 (150) | |
| Seroma | Cases % (no.) | Control % (no.) | p value |
| Present | 14.7 (22) | 50 (75) | <0.001* |
| Absent | 85.3 (128) | 50 (75) | |
| Total | 100 (150) | 100 (150) | |
| Wound Dehiscence | Cases % (no.) | Controls % (no.) | p value |
| Present | 12 (18) | 45.3 (68) | <0.001* |
| Absent | 88 (132) | 54.7 (82) | |
| Total | 100 (150) | 100 (150) | |
| *Statistically significant difference (p value < 0.05) | |||
Table 1: Showing the status of SSI, seroma and wound dehiscence among cases and controls.
Discussion
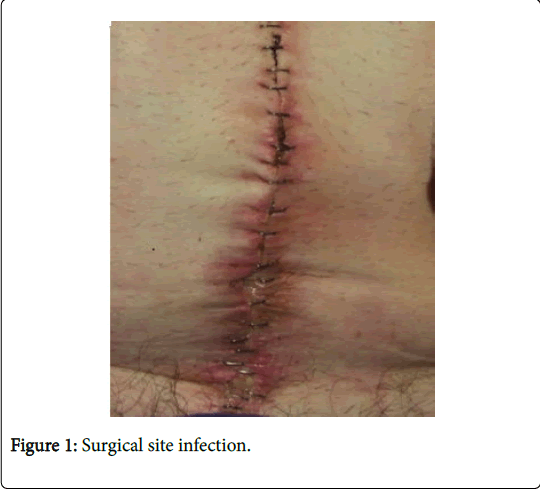
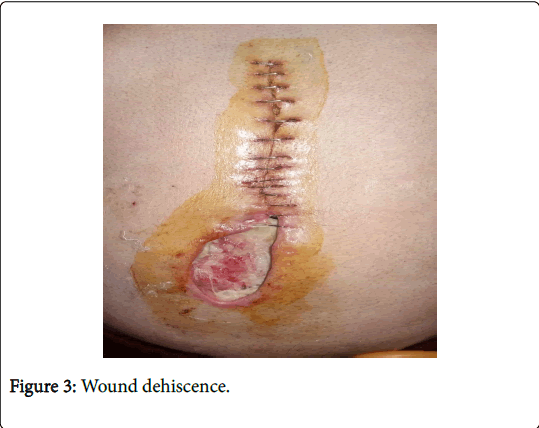
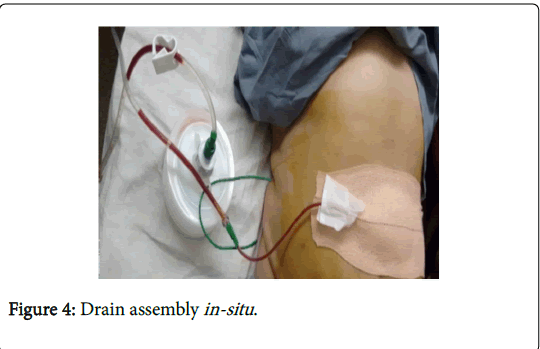
Surgical site infection (Figure 1), seroma formation (Figure 2), and wound dehiscence (Figure 3) is the most common complication in post laparotomy surgery. Infectious complications are the main causes of postoperative morbidity in abdominal surgery. Wound infection: the most common form is superficial wound infection occurring within the first week of surgery. The use of negative suction drain (Figure 4) in subcutaneous plane has been shown to reduce the incidence of surgical site infection, seroma formation, and wound dehiscence; however, there is only a limited data available about their role in contaminated abdominal surgeries (class III wounds).
In our study all patients were given antibiotic prophylaxis. We did not use any topical antibiotic or irrigation through drains as was done in one of the previous studies [7]. Although lack of irrigant in our study may have allowed for occlusion of the catheter by clot or debris, which would have been responsible for wound complications in some cases. The reason for not using irrigation in our study was that Farnell et al. [7] implied in their study that catheter closure technique with antibiotic irrigation in patients with a moderate amount of intraoperative subcutaneous contamination (type II or type III incisions) is not superior to primary closure. Vaghani et al. [8] study showed surgical site infection rate of 25% in study group and 57.7% in control group. Another study was done by Takaaki et al. [9] in the Department of General Surgical Science, Graduate School of Medicine, and Gunma University Japan [10]. In this study surgical site infection rate was 14.3% in study group, and 38% in control group. Khan et al. [11] study showed surgical site infection rate of 12% in study group and 30% in control group. Yasuo et al. [6] in Feb. 2014 carried out a study to determine if a subcutaneous closed suction drain decreases the incidence of wound complications in patients undergoing emergency surgery for colorectal perforation. Data on 47 patients who underwent emergency operations for colorectal perforation were examined retrospectively. The clinical features of these cases with or without the use of the J-VACTM Drainage System were examined, and statistical analysis was performed. In these high-risk cases, the overall incidence of incisional Surgical Site Infection (SSI) was 36.2%. The incidence of incisional SSI in these cases with and without the JVACTM Drainage System was 16.7% and 56.5%, respectively. The results suggest that a subcutaneous closed suction drain is effective for preventing incisional SSI in patients who have undergone emergency operations for colorectal perforation. Our study showed a SSI rate of 15.3% in cases & 30% in controls. The difference was statistically significant (p=0.002), implying a positive role of negative suction subcutaneous drains in preventing SSI.
Chowdri et al. [12] study showed seroma formation in surgical wound after laparotomy surgery of 16.74% in study group in which negative suction drain placed in subcutaneous plane and 72% in control group in which no drain was used. Khan et al. [11] showed seroma formation in study group of 16% and in control group, 42%. In our study seroma formation occurred in 14.7% of cases & 50% of controls (p <0.001).
Khan et al. [11] showed wound dehiscence of 14% in the study group and is 42% in the control group. In our study wound dehiscence occurred in 12% of cases & 45.3% of controls (p<0.001).
Conclusion
The results from the present study show that use of negative suction drain in subcutaneous plane during laparotomy for class III wounds reduces the incidence of postoperative surgical site infection, seroma formation and wound dehiscence. It was concluded that insertion of subcutaneous suction drains at the end of operation could provide effective drainage of the wound collections and SSI, wound seroma, wound dehiscence and their related complications can be avoided in class III wounds.
Conflicts of Interest
Conflict of interest disclosed was none.
References
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR (1999) Guideline for Prevention of Surgical Site Infection. Am J Infect Control 27; 97-132.
- Wilson AP, Gibbons C, Reeves BC, Hodgson B, Liu M, et al. (2004) Surgical wound infection as a performance indicator: agreement of common definitions of wound infection in 4773 patients. BMJ 25; 329:720.
- Scott RD II (2009) The direct medical costs of healthcare-associated infections in US. hospitals and the benefits of prevention.
- Dougherty SH, Simmons RL (1992) The biology and practice of surgical drains. Part 1. Curr Probl Surg 29:559–623.
- Manzoor B, Heywood N, Sharma A (2015) Review of subcutaneous wound drainage in reducing surgical site infections after laparotomy. Surg Res Pract 1-6
- Sumi Y, Yamashita K, Kanemitsu K (2014) Effects of subcutaneous closed suction drain for the prevention of incisional SSI in patients with colorectal perforation. Surg Sci 5:122-127.
- Farnell MB, Worthington S, Peter M, Duane M, McIlrath DC (1986) Closure of abdominal incisions with subcutaneous catheters: A Prospective Randomized Trial. Arch Surg 121:641-648.
- Yagnesh V, Jeeten C, Sudhir N (2014) A study of subcutaneous negative pressure closure versus simple closure in laparotomy wound of ileal perforation. Int J Med Sci Pub Health 3: 24-26.
- Muneiah SN, Roopesh Kumar NM, Sabitha P, Prakash GV (2015) Abdominal wound dehiscence- A look into the risk factors. IOSR- J Dental Med Sci 14:47-54.
- Fujii T, Tabe Y, Yajima R, Yamaguchi S, Tsutsumi S, et al. (2011) Effect of subcutaneous drain for prevention of incisional SSI in high risk patients undergoing colorectal surgery. Int J Colorectal Surg 26:1151-1155.
- Khan AQ, Kodalkar M (2016) Role of negative suction drain in subcutaneous plane in reducing laprotomy wound infection. Int J Scientific Res 5: 692-694.
- Chowdri NA, Qadri SA, Parray FQ, Gagloo MA (2007) Role of subcutaneous drains in obese patients undergoing elective cholecystectomy: A cohort study. Int J Surg 5: 404-407.
Citation: Wani JN and Bhat JA (2019) Role of Negative Suction Subcutaneous Drains in Contaminated Abdominal Surgeries . J Gastrointest Dig Syst 9: 587. DOI: 10.4172/2161-069X.1000587
Copyright: © 2019 Wani JN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5311
- [From(publication date): 0-2019 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 4465
- PDF downloads: 846