Role of High Resolution Manometry in the Evaluation of Esophageal Symptoms
Received: 17-Apr-2020 / Accepted Date: 01-May-2020 / Published Date: 03-May-2020 DOI: 10.4172/2161-069X.1000614
Abstract
Background and Aims Esophageal High Resolution Manometry (HRM) is widely employed for the diagnosis and evaluation of esophageal motor disorders. There is often a dichotomy between HRM findings and various clinicalcorrelates. We attempted to retrospectively evaluate the clinical profiles of patients with their clinical correlates to establish the role of HRM in evaluation of esophageal symptoms. Results Total of 235 patients were studied.Predominant symptoms were Dysphagia (70.6%), Non-cardiac Chest pain (8.5%) and reflux in 9%. Normal HRM was seen in 31.5%, minor motility disorders in 22.5%. Achalasia (61.1%) and Esophago-gastric (EGJ) outflow obstruction (11.1%) was considered as part of the Major disorders. Dysphagia was the most common symptom of which majority of patients had major motility disorders (93 patients (56%)). Normal HRM was seen in 41/166 patients (24.6%) with dysphagia and 68% in NCCP. Only 11% presenting with NCCP had major motility disorder. Half the patients with GERD had a normal HRM study (10/20 patients). On follow up, 78/93 patients (83.8%) were asymptomatic, of which, >50%had normal HRM. Among those with minor motility disorders (n=39), 33(84.6%) were asymptomatic at follow up. Conclusion The significance of HRM in assessment of symptoms other than dysphagia, with diagnosis within the Minor Motility disorders group and associated with benign outcomes, may be questioned. The diagnosis group of Minor Motility disorders, in itself, may be questioned in future Chicago classifications.
Keywords: Motility; Manometry; Chicago Classification; Minor motility disorders; Esophagus
Introduction
Esophageal High Resolution Manometry(HRM) is widely employed for the diagnosis and evaluation of esophageal motor disorders[1–3]. This decade so far, has witnessed a rapid progress in our understanding of HRM and its role in the evaluation of patients with common esophageal symptoms like dysphagia, non-cardiac chest pain, Gastro-esophageal Reflux Disease(GERD) related symptoms and globus sensation among others[2]. The Chicago classification of esophageal motility disorders using HRM has been instrumental in bringing about a classification, providing clarity on diagnosis and subsequently, management[4]. The classification itself, taking into account the results of studies and proposal of various metrics for assessment from across the world, has seen multiple iterations to incorporate new findings and sharpen the diagnostic capability of HRM. The current classification, Chicago v3.0 was published in 2015 and is widely accepted as the gold standard for evaluation of esophageal motility disorders[5].
The clinical presentation of esophageal motility disorders display wide variations in the type and severity of symptoms. The most common and consistent symptom is dysphagia which is defined as a discomfort accompanying an abnormal delay in the transit of liquid or solid bolus during the oropharyngeal or esophageal stages of swallowing[6]. The other symptoms of motility disorder such as chest pain, regurgitation, and night cough however, are not specific for any of the subtypes of motility disorders. In other words, there is often a discrepancy between HRM findings and various clinical correlates, especially when it comes to esophageal motility disorders[3,7]. However, one condition where such a correlation is more accurate is Achalasia[2,8,9]. The diagnostic value of HRM for the evaluation of symptoms other than those of Achalasia is less clear in other conditions[7,10].
On the other hand, HRM is extremely sensitive as compared to conventional manometry in uncovering minor peristaltic breaks and fragmented peristaltic disorders that were previously labelled as normal. However, there is very little evidence to suggest that they are clinically relevant[11].
To that end, we retrospectively evaluated the patients who were referred for an esophageal HRM study to the motility clinic in order to study the clinical profile of these patients and assess the role of HRM in the evaluation of typical esophageal symptoms like dysphagia, non-cardiac chest pain (NCCP), Gastro-Esophageal Reflux disorder (GERD) symptoms, among others (regurgitation, globus sensation and food impaction).
Methods
We performed a single centre, retrospective study where HRM data of patients from June 2014 to May 2016 was collected. The study was approved by the institutional research review board. All the patients who were referred to the motility clinic with symptoms of suspected esophageal motility disorders were analysed. Dysphagia was identified as a difficulty in or discomfort experienced during swallowing. NCCP was considered when patients presented with retro-sternal chest pain and a normal cardio-vascular evaluation. GERD was considered when patients complained primarily of heartburn, sour taste in the mouth, globus sensation etc. Patients aged less than 18 years, those with past history of gastro-intestinal surgery and/or endoscopic dilatations and endoscopy showing strictures, malignancy or ulcers were excluded from the analysis. The relevant baseline characteristics of these patients which included demographics (age, gender), clinical features (symptoms, co-morbidities and investigations) along with treatment details and follow up data (where available) were meticulously recorded. All data were obtained from the hospital electronic medical records, after an institutional ethical committee clearance was obtained.
Institutional protocol for esophageal motility studies and study procedure
As an institution protocol, all esophageal manometry studies were performed in a dedicated manometry room at the Motility Clinic. All patients referred for a motility study underwent an Esophago-Gastro Duodenoscopy (EGD) with Olympus GIF series upper Endoscopes (Olympus Medical TM, Japan) prior to the procedure. HRM was then performed using a water-perfused 16-Channel manometry apparatus as per the following protocol:s
1. Procedure was performed after 6 hours of fasting
2. Clear liquid diet was commenced 2-3 days prior if there was a suspicion of Achalasia.
3. Drugs that affect esophageal motility (Prokinetic, nitrates, Calcium-Channel Blockers, Anti-Cholinergics etc.) were stopped for an appropriate duration prior to the procedure.
4. Supine position was preferred. However, if there was a difficulty in passing the catheter, the procedure was performed in the sitting position.
Each study included the measurement of the mean Basal LES pressures from a 30 second tracing, devoid of any swallows, in addition to inspiratory and expiratory LES pressures. Subsequently, 10 wet swallow (5 ml water) tracings were recorded, making sure that only one swallow was present in a 30 second tracing. The markers on the analysis software were adjusted for each of the swallows for automated calculation of the Distal latency (DL) (Normal value < 4.5sec), Distal Contractile Integral (DCI) (Normal: 45-8000 mm hg- sec- cm) and the pattern of bolus pressurizations (Pan-esophageal, Compartmental, Esophago-gastric Junction and No specific pattern of pressurization). All the swallows were assessed using Chicago V3.0 to arrive at a diagnosis. The diagnosis was coded as normal, achalasia, Esophagogastric outlet obstruction other than achalasia and primary peristaltic disorders. Overall incidence along with correlation of symptoms were then computed.
As per Chicago v3.0, patients were diagnosed to have a normal HRM, a major motility disorder or a minor motility disorder. Major motility disorders include Achalasia, Distal Esophageal Spasm (DES), EGJ outflow obstruction, Absent Contractility and Hypercontractile esophagus (Jackhammer). Minor motility disorders include Ineffective Peristalsis, Fragmented peristalsis and Hypomotility disorders.
In addition to symptoms correlation, the clinical significance of minor motility disorders was also examined. A telephonic survey was conducted in patients with normal or minor motility disorders and the persistence of clinical symptoms, repeated hospital visits for similar symptoms and treatment details were recorded. Patients with persistent symptoms requiring treatment (use of pro-kinetics, proton pump inhibitors for more than 6 months in a year) and/or who had more than one hospital visit for similar symptoms during follow up were noted to have recurrent symptoms
Statistical analysis
Statistical analysis was done using the IBM SPSS Statistics 20 Windows (SPSS Inc., Chicago, USA). The results are given in mean ± SD or Median (Min. to Max.) for all the continuous variables and in frequency (percentage) for categorical variables. The Pearson Chi-Square test with Continuity Correction and Fishers Exact test were used for finding the association between two categorical variables. ANOVA was applied for comparing mean of continuous parameters between three groups. p value of <0.05 was considered statistically significant difference. All tests of statistical significance were two-tailed.
Results
A total of 235 patients were included in the study for analysis. The mean age of the patients who underwent Manometry was 50.9 ± 15.57 years with a median of 48 years. Details of the baseline characteristics, primary symptom, HRM diagnosis and the as shown in Table 1.
| Baseline characteristics | Overall (n=235) | Normal N=74 | Major motility disorders N=108 | Minor motility disorders N=53 |
|---|---|---|---|---|
| Mean age (years ± SD) | 50.9 ± 15.57 | 52.53 ± 15.36 | 48.78 ± 15.30 | 52.94 ± 16.14 |
| Gender n(%) Male Female |
114 (48.5) 121 (51.5) |
35(47.3) 39(52.7) |
45(42.1) 62(57.9) |
33(63.5) 19(36.5) |
| Symptoms Dysphagia NCCP GERD Miscellaneous |
166(70.6) 28(11.9) 20(8.5) 21(8.5) |
41(55.4) 19(25.6) 10(13.5) 4(5.5) |
93(86.2) 3(2.8) 4(3.7) 8(7.3) |
32(60.4) 6(11.3) 6(11.3) 9(17) |
Abbreviations: NCCP – Non cardiac chest pain, GERD – Gastro-esophageal reflux disorder
Symptom distribution
The patients who underwent HRM in our institution were mainly referred for either dysphagia or chest pain. They were divided on the basis of their primary complaint for which they sought evaluation, although other symptoms may have been present.
A total of 166 patients (70.6%) presented with dysphagia. Only 28 patients (11.9%) presented with non-cardiac chest pain while 20 patients (8.5%) had features of GERD and the remaining 21 patients (9%) presented with symptoms ranging from foreign body sensation to frequent belching and regurgitation.
HRM findings
The Chicago classification v 3.0 [5] was used in the HRM analysis and the motility disorders were classified as follows: (Table 2)
| HRM Findings | N (%) |
|---|---|
| Normal | 74 (31.5) |
| Major Motility Disorders | 108 (46) |
| • Achalasia Cardia | 66 (61.1) |
| • Distal esophageal spasm | 13 (12) |
| • EGJ outlet obstruction | 12 (11.1) |
| • Absent contractility | 16 (14.8) |
| • Hypertensive peristalsis | 1 (1) |
| Minor motility disorders | 53 (22.5) |
Abbreviations: HRM- High Resolution Manometry, EGJ- Esophago Gastric Junction.
Table 2: Distribution of patients as per Chicago Classification.
a. Normal Study
b. Major motility disorders
c. Minor motility disorders
It is worthwhile to note that 74 patients (31.5%) with suspected motility disorders were found to have a normal manometry study. Major motility disorders were the most common manometric diagnosis (108/235 patients (46%)) with Achalasia accounting for 66 patients (61.1%). Among the patients with Achalasia, type II was the most common (53/66 patients (80.3%)) while Type I was seen in 3/66 (4.5%) and Type III in 10/66 patients (15.2%).Minor motility disorders were seen in 53 patients (22.5%) and included ineffective peristalsis (n=36), fragmented peristalsis (n=16) and weak peristalsis (n=1).
Symptom correlation with HRM findings
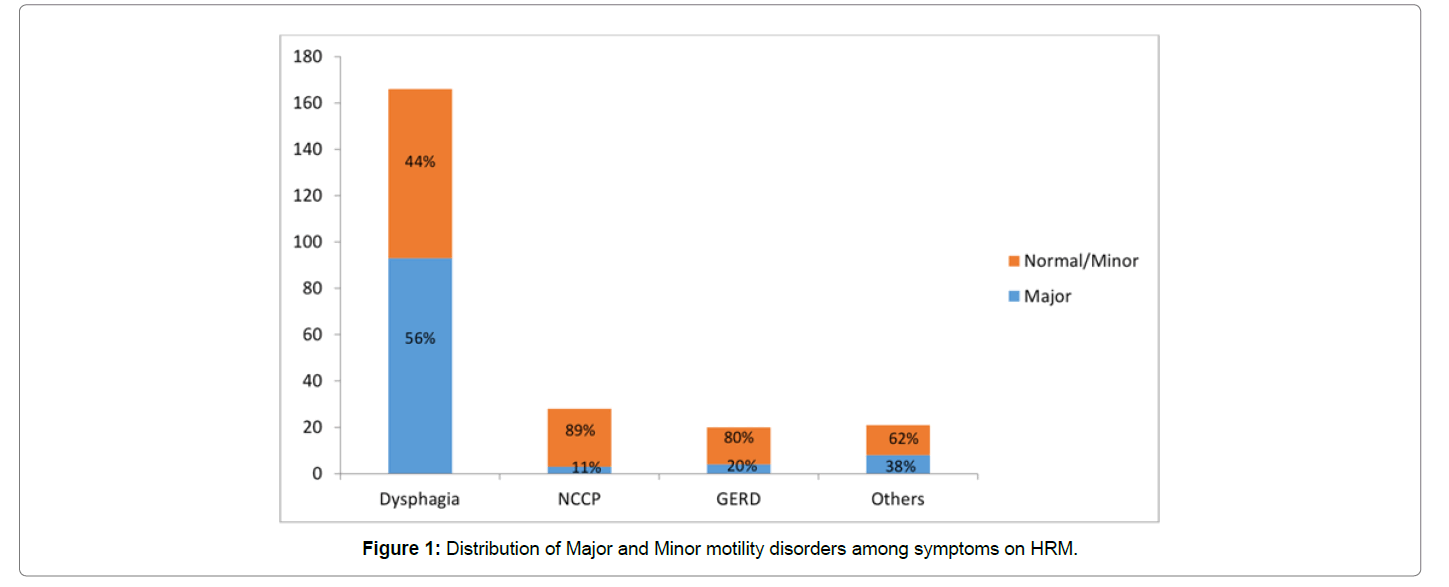
Dysphagia was the most common symptom for which patients were referred for HRM, and among these patients, a significant proportion of patients had major motility disorders (93 patients (56%)) which included Achalasia cardia (n=61; Type I – 2 patients, Type II – 50 patients and Type III – 9 patients), DES (n=7), EGJ outflow obstruction (n=10), Absent Contractility (n=14) and Hypercontractile esophagus (n=1). Normal HRM was seen only in 41/166 patients (24.6%) of patients with dysphagia as compared to patients who presented with NCCP where 19/28 patients (68%) had a normal HRM study. Only 3/28 patients (11%) presenting with NCCP had major motility disorder signifying a poor correlation of this symptom with HRM. Half the patients with symptoms of GERD had a normal HRM study (10/20 patients (50%)) and only 4 patients (20%) had a major motility disorder (Figure 1).
The kappa coefficient between the symptom and an HRM diagnosis of a major motility disorder was found to be the highest with dysphagia (κ-0.275) as opposed to NCCP (κ-0.09), GERD (κ-0.17) and others (κ- 0.03).
EGD Findings in Minor Motility Disorders and Normal HRM study
Amongst the patients with a ‘Normal’ HRM study, details of EGD were available in 67/74 patients. The predominant finding was of Reflux Esophagitis (34/67 (50.7%)). Ulcers and features of acid peptic disease were seen in 21/67 (31.34%). A normal study was seen only in 6/67 (8.9%). Other non-specific symptoms were only seen in 2 patients.
Amongst those with ‘Minor Motility Disorders’ EGD details were available for 51/53 patients. Reflux Esophagitis was the predominant finding in 27/53 (50.9%) followed by ulcers and features of APD (13/53 (24.5%)), a normal study (7/53 (13.2%)) and other non-specific findings in 4/53 (7.5%).
Clinical significance of normal/minor peristaltic disorders
A total of 93/127 patients who had a normal or minor motility disorder could be traced via a telephonic survey. Of these patients, 78/93 patients (83.8%) were asymptomatic at follow up of which, 45 patients (57.6%) had normal HRM at presentation. Ineffective esophageal motility was seen in 25 patients (32%) who had no symptoms at follow up, while the remaining 8 patients (10.4%) had other minor motility disorders. Among the 15 patients who had significant symptoms at follow up necessitating multiple hospital visits, investigations and continuing pharmacotherapy(PPIs, Prokinetics), 9 patients (60%) had normal HRM and 4 (26.7%) had ineffective esophageal motility at presentation.
Moreover, among the patients who had normal HRM at presentation and with follow up data (n=54), 45 patients (83.4%) were asymptomatic. Even in patients who had minor motility disorders (n=39), 33 patients (84.6%) were asymptomatic at follow up.
Discussion and Conclusion
The advent of HRM in clinical practice changed the landscape of evaluation of esophageal motility disorders. The transformation from the Clouse plots in the 1990s to the Chicago classification v3.0 has provided a wider understanding of this unique group of disorders. HRM has now become the gold standard for the evaluation and diagnosis of esophageal motility disorders[12].
Although the impact of HRM has been significant in the management of Achalasia, the same cannot be stated with regard to motility disorders such as Ineffective peristalsis and other minor motility disorders. This is reflected in the poor symptom correlation with the HRM findings and the lack of specific treatment strategies. A large proportion of patients who presented with significant symptoms were found to have a normal HRM study. Various factors that have been attributed to this dichotomy including the bolus consistency, shape and surface area, not measured by manometry[13]. In our observations, 74 patients(31.5%) had normal HRM study, which is comparable to the previous studies[14,15].
Dysphagia was the most common symptom for referral to the motility clinic 166 patients (70.6%). It is worthwhile to note that a larger proportion of patients with dysphagia have a major motility disorder as compared to NCCP and other symptoms. Majority of patients with NCCP had normal or minor motility disorders. Similar findings were observed in multiple studies across the world where NCCP was not found to be a good indicator for a major motility disorder[7,15]. This reiterates the role of eliciting a good history and identifying the patient who will benefit from manometry study. In a study by Jain et. al., the presence of dysphagia had a sensitivity of 57.58% and a specificity of 74.55% for finding a peristaltic abnormality on the HRM with a positive predictive value of 80%[7]. Detecting minor peristaltic disorders may not have any clinical relevance in everyday practice. Despite the larger proportion of patients with major motility disorders being in the group with dysphagia, the kappa coefficient is quite low (0.275). This suggests a poor correlation of symptoms with major motility disorders and it would be worthwhile to keep this in mind when evaluating patients. This study also necessitates the need to develop composite clinical risk assessment scores that can include additional clinical covariates, apart from symptoms, in order to warrant an HRM study. This may enhance our ability to correctly identify the incidence of major esophageal motility disorders.
In this study, a telephonic survey of patients with normal and minor motility disorders was carried out which showed that more than 80% of these patients were asymptomatic at follow up. Such patients were treated symptomatically with proton pump inhibitors, prokinetics, dietary and lifestyle modifications. Owing to the retrospective design of the study, the treatment protocol was not uniform and can be a significant drawback to form any conclusion on patient outcomes. Despite this drawback, the finding that majority of these patients were asymptomatic, with no specific treatment offered, and could give us valuable information as to the clinical significance of HRM in these patients. A similar finding was observed in a study by Ravi et. al. who followed up patients with normal or minor motility disorders and found that only 16% had significant symptoms on long term follow up requiring medical interventions.[11]
Among minor motility disorders, ineffective peristalsis was the most common finding in our study (67.9%). On follow up, 8/36 were asymptomatic. The outcome of patients with ineffective peristalsis has been an area of intense study. Some investigators suggest that these patients may develop major motility disorders on follow up like Achalasia and DES[16]. There is also objective evidence that ineffective peristalsis with large breaks can lead to failure of bolus clearance and fragmented peristalsis can lead to GERD [17,18] Ravi et. al., however, showed that none of the minor motility disorders had a bad outcome on long term follow up[11]. Moreover, it has also been shown that these findings can be seen in asymptomatic individuals and their correlation with symptoms is tenuous at best[19]. It is noteworthy that among the patients with minor motility disorders, only 7 patients had a normal EGD. The most common findings were of reflux and acid peptic disease. It is likely that treatments targeted at these findings have led to symptom relief. Our study is an important addition to the growing body of evidence that purports a poor correlation between symptoms and HRM diagnoses. Our study also raises important questions as to the place of minor motility disorders in our everyday clinical practice. Although newer reports suggest a specific sub group of patients, within the broad definition of ineffective peristalsis, may have consistent clinical correlates that may have clinical relevance [20], it remains to be seen if future iterations of the Chicago classification would consider these manometry abnormalities as significant based on current evidence.
References
- Gyawali CP (2012) High resolution manometry: The Ray Clouse legacy. Neurogastroenterol Motil 1: 2–4.
- Kahrilas PJ, Bredenoord AJ, Fox M, Prakash Gyawali C, Roman S, et al. (2017) Expert consensus document: Advances in the management of oesophageal motility disorders in the era of high-resolution manometry: A focus on Achalasia syndromes. Nat Rev Gastroenterol Hepatol 14: 677–688.
- Van Hoeij FB, Bredenoord AJ (2016) Clinical application of esophageal high-resolution manometry in the diagnosis of esophageal motility disorders. J Neurogastroenterol Motil 22: 6–13.
- Kahrilas PJ, Ghosh SK, Pandolfino JE (2008) Esophageal motility disorders in terms of pressure topography: The Chicago classification. J Clin Gastroenterol 42(5): 627–635.
- Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, et al. (2015) The Chicago Classification of esophageal motility disorders. Neurogastroenterol Motil 27: 160–174.
- Jalil AAA, Katzka DA, Castell DO (2015) Approach to the patient with dysphagia. Am J Med 128(10): 1138.e17-23.
- Jain M, Srinivas M, Bawane P, Venkataraman J (2017) Does Chicago Classification address Symptom Correlation with High-resolution Esophageal Manometry? Euroasian J Hepatogastroenterol 7: 122–125.
- Mikaeli J, Islami F, Malekzadeh R (2009) Achalasia: A review of Western and Iranian experiences. World J Gastroenterol 15(40): 5000–5009.
- Müller M (2015) Impact of high-resolution manometry on achalasia diagnosis and treatment. Ann Gastroenterol 28: 3–9.
- Schlottmann F, Patti MG (2017) Primary esophageal motility disorders: Beyond achalasia. Int J Mol Sci 18(7).
- Ravi K, Friesen L, Issaka R, Kahrilas PJ, Pandolfino JE (2015) Long-term Outcomes of Patients With Normal or Minor Motor Function Abnormalities Detected by High-resolution Esophageal Manometry. Clin Gastroenterol Hepatol 13: 1416–1423.
- Sato H, Takahashi K, Mizuno K, Hashimoto S, Yokoyama J, et al. (2017) Esophageal motility disorders: new perspectives from high-resolution manometry and histopathology J Gastroenterol 53: 484–493.
- Bogte A, Bredenoord AJ, Oors J, Siersema PD, Smout AJPM (2012) Relationship between esophageal contraction patterns and clearance of swallowed liquid and solid boluses in healthy controls and patients with dysphagia. Neurogastroenterol Motil. England 24: e364-72.
- Goyal O, Bansal M, Sood A (2017) Esophageal motility disorders-Symptomatic and manometric spectrum in Punjab, northern India. Indian J Gastroenterol 36: 202–208.
- Saha AK, Roy N, Hazra SC (2015) Role of Esophageal Manometry in Patients With Reflux Symptoms, Dysphagia and Noncardiac Chest Pain. IJSR 6: 2599–2601.
- Samo S, Carlson DA, Kahrilas PJ, Pandolfino JE (2016) Ineffective Esophageal Motility Progressing into Distal Esophageal Spasm and Then Type III Achalasia. ACG Case Rep J 3(4): e183.
- Roman S, Lin Z, Kwiatek MA, Pandolfino JE, Kahrilas PJ (2010) Weak Peristalsis in Esophageal Pressure Topography: Classification and Association With Dysphagia. Am J Gastroenterol 106: 349.
- Porter RF, Kumar N, Drapekin JE, Gyawali CP (2012) Fragmented esophageal smooth muscle contraction segments on high resolution manometry: a marker of esophageal hypomotility. Neurogastroenterol Motil. England 24(8): 763-768, e353.
- Herregods TVK, Roman S, Kahrilas PJ, Smout AJPM, Bredenoord AJ (2015) Normative values in esophageal high-resolution manometry. Neurogastroenterol Motil 27: 175–187.
- Jain A, Baker JR, Chen JW (2018) In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil 30: e13297.
Citation: Prakash A, Koshy AK (2020) Role of High Resolution Manometry in the Evaluation of Esophageal Symptoms. J Gastrointest Dig Syst 10: 614. DOI: 10.4172/2161-069X.1000614
Copyright: © 2020 Prakash A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2608
- [From(publication date): 0-2020 - Mar 11, 2025]
- Breakdown by view type
- HTML page views: 1923
- PDF downloads: 685