Research Article Open Access
Role of Electrical Muscle Stimulation (EMS) for Treatment or Prevention of ICU-associated Weakness
Dharam Pani Pandey1*, Ram Babu2 and Esha Arora11Department of Physiotherapy and Rehabilitation, BLK Super Speciality Hospital, New Delhi, India
2Department of Internal Medicine, Jaipur Golden Hospital, New Delhi, India
- *Corresponding Author:
- Dharam Pani Pandey
Department of Physiotherapy & Rehabilitation
BLK Super Speciality Hospital
Pusa Road, New Delhi-110085, India
Tel: +911130653154; +919818910029
E-mail: drdprehab@gmail.com
Received date: September 16, 2016; Accepted date: December 01, 2016; Published date: December 14, 2016
Citation: Pandey DP, Babu R, Arora E (2016) Role of Electrical Muscle Stimulation (EMS) for Treatment or Prevention of ICU-associated Weakness . J Nov Physiother 6:318. doi:10.4172/2165-7025.1000318
Copyright: © 2016 Pandey DP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Background: Neuromuscular abnormalities developing as a consequence of critical illness can be found in the
majority of patients hospitalized in the intensive care unit (ICU) for 1 week or more. The spectrum of illness ranges
from isolated nerve entrapment with focal pain or weakness, to disuse muscle atrophy with mild weakness, to severe
myopathy or neuropathy with associated severe, prolonged weakness. The prevalence and impact of acquired
neuromuscular weakness is likely larger than generally recognized. Greater than 50% of patients mechanically
ventilated for more than 7 days will develop electrophysiologic abnormalities, with 25–33% developing clinically overt
weakness. Acquired neuromuscular dysfunction is associated with difficulty in separating from mechanical
ventilation, increased hospital costs, and increased mortality.
Objective: This study was designed to investigate the effects of electrical muscle stimulation (EMS) on strength
of muscle groups stimulated and gain in functional independence in critically ill patients.
Methods: Subjects were recruited among the patient admitted in multidisciplinary intensive care units during the
study period. The study employed a randomized single blind controlled experimental study design consisting of two
group experimental group (Electrical stimulation group) and control group. The MRC score was used for clinical
assessment of muscle strength and barthel index were used to assess the level of independence.
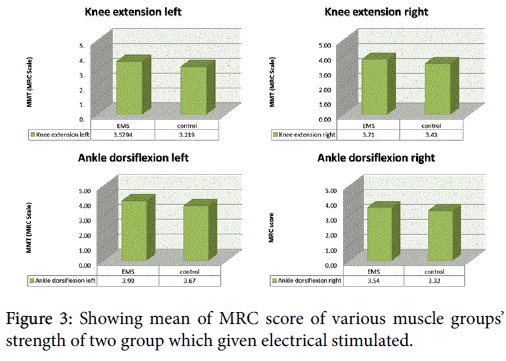
Results: EMS group patients achieved higher MRC scores than controls in knee extensors (left P ≤ 0.01), (right
P ≤ 0.01) and ankle dorsiflexors (left P ≤ 0.02), (right P ≤ 0.02).
Conclusions: EMS has beneficial effects on the preserving strength of critically ill patients mainly affecting
muscle groups stimulated, it also has beneficial effect on improving the functional independence level post ICU
discharge, it can be considered as a potential effective means of muscle strength preservation and early mobilization
in this patient population.
Keywords
Electrical muscle stimulation; Muscle strength; CIPNM; CIM; ICU-AW
Introduction
Weakness that is acquired during hospitalization for critical illness is increasingly recognized as common and important clinical problem. Weakness acquired in the intensive care unit (ICU) and related acquired neuromuscular dysfunction occur in a large percentage of critically ill patients [1-3] and are associated with increased morbidity and mortality [4,5]. Critical illness polyneuromyopathy (CIPNM) is an acquired neuromuscular disorder observed in survivors of acute critical illness. It is characterized by profound muscle weakness and diminished or absent deep tendon reflexes [1] and is associated with delayed weaning from mechanical ventilation [2] suggesting a possible relation between limb and respiratory neuromuscular involvement. In addition, the syndrome is associated with prolonged hospitalization and increased mortality [3]. The diagnosis of CIPNM requires a reliable bedside muscle strength examination and depends on patient's cooperation and maximal effort [4].
Several risk factors have been identified including systemic inflammatory response and sepsis [5], medications such as corticosteroids [6] and neuromuscular blocking agents [7], inadequate glycemic control [8], protracted immobility [4], hypoalbuminemia [9], Gram-negative bacteremia [9] and severity of organ dysfunction [10]. A very few of studies available suggesting the treatment and prevention of critical illness myopathy these includes intensive insulin therapy, optimal glycemic control and minimized use of neuromuscular blocking agents, high dose and prolong use of corticosteroids.
Objective of the study
The objective of this study was to investigate whether electrical muscle stimulation (EMS) would decrease the incidence of ICUassociated muscle weakness
Our experimental Hypothesis was that “EMS would beneficially affect muscle functional status and preserve muscle strength in the critically ill patients.
Material and Methods
Subjects
The 212 subjects were recruited among the patient admitted in multidisciplinary intensive care units during the 8 month study period.
Inclusion criteria
More than 2 days of mechanical ventilation with an expectation of requiring ≥ 2 additional days of mechanical ventilation in the Medical Intensive Care Unit (MICU), and Respiratory Intensive Care Unit (RICU). Age 18 years and above.
Exclusion criteria
Unable to understand or speak English and or Hindi due to language barrier or cognitive impairment prior to admission, unable to independently transfer from bed to chair at baseline prior to hospital admission (based on detail history taken from caregivers.
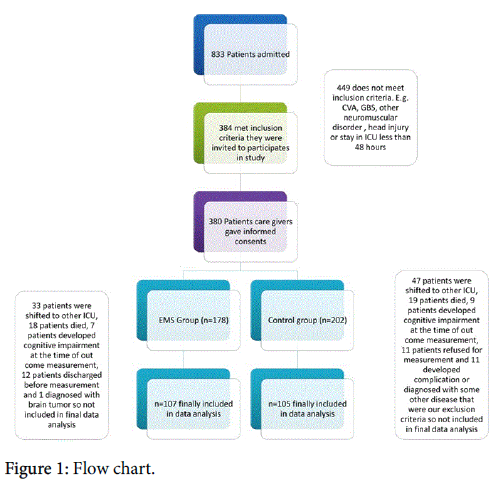
Patient with known history of primary systemic neuromuscular disease, vascular events, organ transplant, intracranial process that associated with localizing weakness, transferred from another ICU after >2 consecutive days of mechanical ventilation, amputation of lower extremities, any limitation of life support, pregnancy, age under 18 years, obesity, technical obstacles that did not allow the implementation of EMS such as bone fractures, skin lesions and, endstage malignancy were excluded from our study (Figure 1).
Design of study
The study employed a randomized single blind controlled experimental study design consisting of two group experimental group and control group, Subjects were randomly assigned ether to experimental group or to control group every day the ICU patient admission register were observed and within 24 hour the assessment were done, each time when a patient met the criteria for inclusion a random number were picked up between 1 to 10 using sealed envelope method if it were an odd number than the subject were assigned to experimental group similarly if even number were obtained the subjects were assigned to control group.
Intervention
EMS was implemented on knee extensors, tibialis anterior and of both lower extremities. Patients received daily sessions. After skin cleaning, rectangular electrodes (90 × 50 mm) were placed on motor point of targeted muscle.
The stimulator (Unistim, HMS medical system) delivered biphasic, symmetric impulses of 50 Hz, 100 μsec pulse duration, 12 seconds at intensities able to cause visible contractions. The duration of the session was 30 minutes each muscle group. EMS sessions were continued until ICU discharge, both group were getting routine physiotherapy included the passive movements, active assisted movements and chest physiotherapy.
Outcome measures
MRC muscle strength scale: The MRC score was used for clinical assessment of muscle strength. After ICU discharge, MRC grading of muscles was on the same day. As soon as patients shifted from ICU level of consciousness adequate to respond to at least three of the following orders ('open/close your eyes', 'look at me', 'put out your tongue', 'nod your head', 'raise your eyebrows') [11].
Three muscle groups in all four limbs were assessed with the MRC scale with values ranging from 0 (quadriplegia) to 60 (normal muscle strength). The following functions were assessed, wrist flexion, forearm flexion, shoulder abduction, ankle dorsiflexion, knee extension, and hip flexion [12]. Patients with an MRC score of less than 48 of 60 were considered the case of ICU induced weakness.
Functional independence: The Barthel index were used to assess the level of independence. After assessing the MMT at least 6 hours but not more than 12 hour rest was given to patient before assessing the barthel score.
Other data were recorded such as duration of mechanical ventilation at ICU, ICU and hospital length of stay at ICU and hospital discharge, and Hospital discharge destination (e.g., home, rehab facility).
Data analysis: All continuous variables were presented by mean. The statistical significance of P value was set at 0.05. One way repeated measures analysis of variance (ANOVA) was made to compare MRC Grading and barthel index score.
Results and Discussion
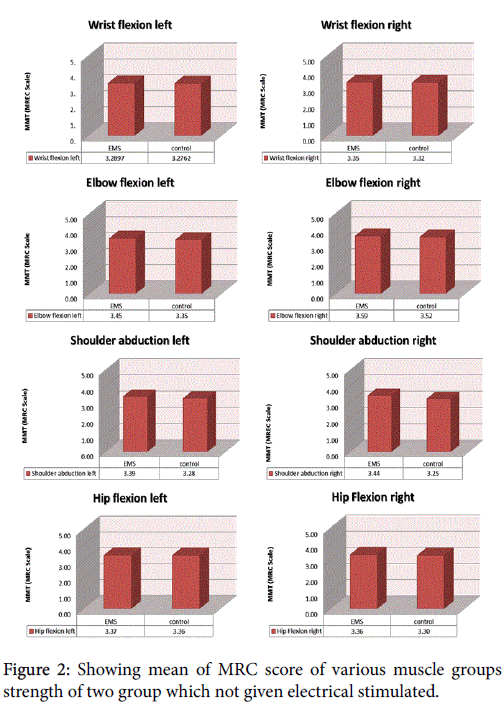
The final results shows significant difference (MRC muscle grading score of muscle being stimulated) between two groups, EMS group showed preserved muscle strength at time of discharged from ICU as compared to control group. Numerical data is summarized in Table 1.
| Intervention group(mean n=107) | Control group(mean n=105) | p-Value | ||
| Shoulder abduction | Lt | 3.39 | 3.28 | 0.32 |
| Rt | 3.44 | 3.25 | 0.12 | |
| Elbow flexion | Lt | 3.45 | 3.35 | 0.52 |
| Rt | 3.59 | 3.52 | 0.66 | |
| Wrist flexion | Lt | 3.29 | 3.28 | 0.92 |
| Rt | 3.35 | 3.32 | 0.86 | |
| Hip flexion | Lt | 3.37 | 3.36 | 0.92 |
| Rt | 3.36 | 3.3 | 0.63 | |
| Knee extension | Lt | 3.58 | 3.22 | 0 |
| Rt | 3.71 | 3.43 | 0.01 | |
| Ankle dorsiflexion | Lt | 3.99 | 3.67 | 0.02 |
| Rt | 3.54 | 3.32 | 0.02 | |
Table 1: Showing mean and corresponding significance level of manual muscle testing (MRC Scale).
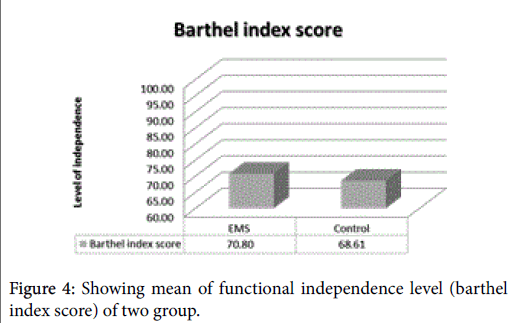
Level of independence as assessed using barthel index score were found significant difference between two groups, the mean score of EMS group was 70.80% of 100 and control group was 68.61% of 100 (p=0.01).
The main finding of this study is that daily, 30-minute EMS sessions prevented the development of critical illness associated muscle weakness in critically ill patients. Furthermore, EMS treatment was associated with improved level of independence at ICU discharge, avoidance of known risk factors, including hyperglycaemia, is the only preventive measure proposed so far [12].
To our knowledge, this is the first randomized single blinded control intervention study to suggest that of 30-minute EMS sessions would reduce the risk of development of critical illness associated muscle weakness in critically ill patients. Furthermore, EMS treatment was associated with an improved level of independence at ICU discharge in critically ill patients and preserves the muscle strength as assessed with the MRC score, thus potentially providing a preventive tool for this condition.
Our current understanding of muscle turnover, in regards to adaptation during critical illness, is poorly described. Increasing age affects the response of (MPS) muscle protein synthesis and (MPB) muscle protein breakdown to specific stimuli, including resistance training [13].
Other factors are reported to affect muscle mass in animal models [14], which may have little relevance to human disease. Some factors are likely to have universal effects on healthy subjects and critically ill patients.
EMS has been extensively used as an alternative to active exercise in patients with chronic heart failure (CHF) and chronic obstructive pulmonary disease (COPD) [15]. Many of these patients, even those who are clinically unstable, experience severe dyspnea on exertion, which can prohibit the regular application of conventional exercise training, considered necessary for an integrated therapeutic approach. In a recent systematic review, EMS implementation in most of the selected controlled clinical trials produced significant improvements in muscle strength, exercise capacity and disease-specific health status [15-18].
EMS, as a possible substitute to aerobic and resistance exercise training in severe CHF and COPD patients, has been shown to improve muscle performance, aerobic exercise capacity (Figure 2), and disease-specific health status [9-13].
Critical illness associated muscular weakness a common complication in patients who are mechanically ventilated due to critical illness. One of major causative factor is resulting from negative effect of bed rest, immobility, inactivity which directly and indirectly affects the muscle protein synthesis and muscle protein breakdown imbalance which is further facilitated by catabolic state in critically ill patients, contributing to development of muscle weakness.
There are various limitations to active exercises these limitations may be resulting from critical illness itself or other major contributing factors such as risk of dislodging of various line and tubes during exercise session, vital status issues and of course use of neuromuscular blocking agents & sedition to facilitate mechanical ventilation (Figure 3).
This study suggesting that the use of daily EMS sessions can prevent and slow down the development of critical illness associated muscular weakness in critically ill ICU patients, preserved the muscle strength and improved the level of functional independence post ICU discharge.
Thus potentially providing a preventive tool for this condition, EMS should be considered while clinical reasoning in critically ill patients who requires mechanical ventilation.
Conclusion
This randomized intervention trial suggest that EMS of lower extremities can prevent or slow down the development of critical illness associated muscular weakness in critically ill ICU patients. Daily EMS sessions prevented and slow down the development of critical illness associated muscular weakness in critically ill ICU patients preserved the muscle strength and improved the level of functional independence post ICU discharge.
EMS is an easily applicable, well-tolerated form of exercise that does not requires patient cooperation, can be applied in any muscle group and can be implemented immediately after ICU admission.
In this study, use of daily EMS of lower extremities was shown to prevent or slow down the development of critical illness associated muscular weakness in critically ill ICU patients preserved the muscle strength and improved the level of functional independence post ICU discharge thus contributing to decreased morbidity, improved mobility and improved independence level post ICU stay.
Further studies are needed to define which patients would benefit most from this intervention and to explore the EMS characteristics (current characteristics and muscle groups) that are most appropriate for this use.
The main limitation of our study is the relatively wide range age group of critically ill patients that were included (Figure 4).
Limitations
We did not use sham-EMS sessions in patients assigned to the control group.
The effect of EMS was assessed on muscle strength, but not on muscle cross sectional area and also electrophysiological evaluation was not performed, which would have assisted in the evaluation of patients who did not regain adequate cognitive function in order to perform the MRC scale.
Further studies are needed to explore the possible role of EMS as a tool for preserving the muscle strength; the muscle properties and preventing CIPNM in critically ill patients and to define which patients would benefit most from this intervention.
Acknowledgements
We would like to acknowledge the support of all intensive care unit staff, consultants and all the patient caregivers.
Conflict of Interest
Authors declare that they have no conflict of interest.
Source of Funding
This study was self-finance and authors have no financial interest.
References
- De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, et al. (2002)Groupe de Reflexion et d’Etude des Neuromyopathies en Reanimation. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA 288:2859-2867.
- de Letter MA, Schmitz PI, Visser LH, Verheul FA, Schellens RL, et al. (2001) Risk factors for the development of polyneuropathy and myopathy in critically ill patients. Crit Care Med 29:2281-2286.
- Coakley JH, Nagendran K, Yarwood GD, Honavar M, Hinds CJ (1998) Patterns of neurophysiological abnormality in prolonged critical illness. Intensive Care Med 24:801-807.
- Garnacho-Montero J, Madrazo-Osuna J, Garcia-Garmendia JL, Ortiz- Leyba C, Jimenez-Jimenez FJ, et al. (2001) Critical illness polyneuropathy: risk factors and clinical consequences: a cohort study in septic patients. Intensive Care Med 27: 1288-1296.
- Spitzer AR, Giancarlo T, Maher L, Awerbuch G, Bowles A (1992) Neuromuscular causes of prolonged ventilator dependency. Muscle Nerve 15:682-686.
- Rudis MI, Guslits BJ, Peterson EL, Hathaway SJ, Angus E, et al. (1996) Economic impact of prolonged motor weakness complicating neuromuscular blockade in the intensive care unit. Crit Care Med 24:1749-1756.
- Latronico N, Peli E, Botteri M (2005) Critical illness myopathy and neuropathy. CurrOpinCrit Care 11:126-132.
- Bednarik J, Lukas Z, Vondracek P (2003) Critical illness polyneuromyopathy: the electrophysiological components of a complex entity. Intensive Care Med 29:1505-1514.
- Berghe GVD, Wouters P, Weekers F, Verwaest C, Bruyninckx F, et al. (2001) Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359-1367.
- Tennila A, Salmi T, Pettila V, Roine RO, Varpula T, et al. (2000) Early signs of critical illness polyneuropathy in ICU patients with systemic inflammatory response syndrome or sepsis. Intensive Care Med 26:1360-1363.
- Bolton CF, Gilbert JJ, Hahn AF, Sibbald WJ (1984) Polyneuropathy in critically ill patients. J NeurolNeurosurg Psychiatry 47: 1223-1231.
- Gerovasili V,Tripodaki E, Karatzanos E, Pitsolis T, Markaki V, et al. (2009) Short-term Systemic Effect of Electrical Muscle Stimulation in Critically Ill Patients. Chest 136:1249-1256.
- Kumar V, Selby A, Rankin D, Patel R, Atherton P, et al. (2009) Age-related differences in the dose–response relationship of muscle protein synthesis to resistance exercise in young and old men. J Physiol 587: 211-217.
- Sacheck JM, Hyatt JP, Raffaello A, Jagoe RT, Roy RR, et al. (2007) Rapid disuse and denervation atrophy involve transcriptional changes similar to those of muscle wasting during systemic diseases. FASEB J 21:140-155.
- Latronico N, Fenzi F, Recupero D, Guarneri B, Tomelleri G, et al. (1996) Critical illness myopathy and neuropathy. Lancet 347:1579-1582.
- Rich MM, Bird SJ, Raps EC, McCluskey LF, Teener JW (1997) Direct muscle stimulation in acute quadriplegic myopathy. Muscle Nerve 20:665-673.
- Friedrich O, Fink RH, Hund E (2005) Understanding critical illness myopathy: approaching the pathomechanism. J Nutr 135: 1813S-1817S.
- Duchateau J, Hainaut K (1987) Electrical and mechanical changes in immobilized human muscle. J ApplPhysiol (1985) 62: 2168-2173.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 4643
- [From(publication date):
December-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 3793
- PDF downloads : 850