Review Article Open Access
Role of Calcitonin Gene-related Peptide in Gastric Motility Function: Animal and Human Studies
Shaquana Y. Clark1 and Pandu R. Gangula2*1Department of Physiology and Oral Biology and Research Meharry Medical College, USA
2Department of Physiology, Oral Biology and Research, Center for Women’s Health Research, Meharry Medical College, Nashville, TN, USA
- *Corresponding Author:
- Pandu R. Gangula, PhD
Department of Physiology
Oral Biology and Research Meharry Medical College
School of Medicine and School of Dentistry
1005 Dr. D.B. Todd Jr. Blvd Nashville
TN 37208, USA
Tel: +01-615-327-6511
Fax: 615-327-6218
E-mail: pgangula@mmc.edu
Received date: February 22, 2015; Accepted date: March 28, 2015; Published date: April 10, 2015
Citation: Clark SY, Gangula PR (2015) Role of Calcitonin Gene-related Peptide in Gastric Motility Function: Animal and Human Studies. J Gastrointest Dig Syst 5:276. doi:10.4172/2161-069X.1000276
Copyright: © 2015 Clark SY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Diabetes is one of the leading causes of gastroparesis. Gastroparesis is a state of partial gastric paralysis where gastric emptying is delayed due to slower or faster gastric motility. Over the years, many other distinct causes of gastroparesis have emerged, including collagen-related vascular diseases and Parkinson’s disease. Calcitonin gene-related peptide, or CGRP, a potent smooth muscle relaxant, is a 37-amino acid neuropeptide found in the gastrointestinal system that has been shown to slow gastric emptying in healthy rodents. Regulation of its synthesis and release from neurons is achieved in part by activation of the transient receptor potential vanilloid subtype 1 (TRPV1). Regulation of its function is achieved by binding to its own receptor, a complex of the Calcitonin Receptorlike Receptor (CRLR) and Receptor Activity Modifying Protein 1 (RAMP1). In the gastrointestinal system, CGRP regulates the release of somatostatin, also known as Growth Hormone Inhibiting Hormone, or GHIH. Somatostatin functions to inhibit the release of gastric acid thus, demonstrating a possible indirect role of CGRP in the pathogenesis of gastroparesis. Cells present in the gastrointestinal system include mucosal cells, submucosal cells, myenteric neuronal cells, and others. CGRP is localized in the gastric mucosa and the myenteric plexus. The neurons present in the enteric or myenteric nervous system play a vital role in gastric motility functions. CGRP is released from the inhibitory neurons in the enteric or myenteric nervous system. Both serum and gastric CGRP have been found to be decreased in diabetes, but it is not known whether these decreases play a role in the pathogenesis of gastroparesis in diabetic/idiopathic patients. The present review provides information about CGRP, its functions, and its possible roles in gastroparesis. The findings presented can be a great asset to the medical community in directing future research for possible causes and developing treatments for gastroparesis.
Abstract
Diabetes is one of the leading causes of gastroparesis. Gastroparesis is a state of partial gastric paralysis where gastric emptying is delayed due to slower or faster gastric motility. Over the years, many other distinct causes of gastroparesis have emerged, including collagen-related vascular diseases and Parkinson’s disease. Calcitonin gene-related peptide, or CGRP, a potent smooth muscle relaxant, is a 37-amino acid neuropeptide found in the gastrointestinal system that has been shown to slow gastric emptying in healthy rodents. Regulation of its synthesis and release from neurons is achieved in part by activation of the transient receptor potential vanilloid subtype 1 (TRPV1). Regulation of its function is achieved by binding to its own receptor, a complex of the Calcitonin Receptor-like Receptor (CRLR) and Receptor Activity Modifying Protein 1 (RAMP1). In the gastrointestinal system, CGRP regulates the release of somatostatin, also known as Growth Hormone Inhibiting Hormone, or GHIH. Somatostatin functions to inhibit the release of gastric acid thus, demonstrating a possible indirect role of CGRP in the pathogenesis of gastroparesis. Cells present in the gastrointestinal system include mucosal cells, submucosal cells, myenteric neuronal cells, and others. CGRP is localized in the gastric mucosa and the myenteric plexus. The neurons present in the enteric or myenteric nervous system play a vital role in gastric motility functions. CGRP is released from the inhibitory neurons in the enteric or myenteric nervous system. Both serum and gastric CGRP have been found to be decreased in diabetes, but it is not known whether these decreases play a role in the pathogenesis of gastroparesis in diabetic/idiopathic patients. The present review provides information about CGRP, its functions, and its possible roles in gastroparesis. The findings presented can be a great asset to the medical community in directing future research for possible causes and developing treatments for gastroparesis.
Keywords
Gastroparesis; Gastric motility; Calcitonin gene-related peptide; CRLR; RAMP1; Somatostatin
Introduction
Gastroparesis is a common condition among diabetic and idiopathic patients, with diabetes accounting for 29% of the cases [1]. Diabetes is a condition in which the body does not produce insulin, or effectively use the insulin produced. There are two types of diabetes, Type 1 and Type 2. Type 1 diabetes is an insulin-dependent condition in which the body does not produce insulin [2]. The causes of Type 1 diabetes are unknown; however, there are risk factors, such as having parents with Type 1 diabetes, having Type 2 polyglandular syndrome, or other immune disorders. Type 2 diabetes is a non-insulin dependent condition in which patients are not effectively using the insulin produced. Risk factors include genetics and lifestyle, such as eating habits and obesity [3]. Obesity is one of the most important risk factors in developing Type 2 diabetes. Obesity alters the amount of specific hormones secreted from adipose tissue. These hormones, called adipokines, cause insulin resistance. In obesity, adipose tissue secretes more adipokines, leading to increased insulin resistance and less insulin sensitivity, which leads to diabetes [4]. Gastroparesis can also be an idiopathic condition, where the exact cause of the condition is unknown. This accounts for 35.6% of all gastroparesis cases [1].
Gastroparesis is a state of partial gastric paralysis where gastric emptying is delayed [5].
Gastric emptying is the process by which food empties the stomach and enters the small intestine [1]. It is largely regulated by neurons of the enteric nervous system (ENS) [6]. It begins with food traveling down the esophagus and into the fundus of the stomach, where it is stored [6] and mixed with gastric acid, beginning digestion. Food then travels to the antrum, or body, where muscular contractions are the strongest [7]. Next, food reaches the pylorus, the lowest portion of the stomach, where it is now in a paste-like form called chyme. While in the pylorus, muscle contractions continue. Finally, the chyme reaches the duodenum, the first part of the small intestine, and gastric emptying is complete [1]. In gastroparesis, this process is delayed5 and the rate at which food reaches the small intestine is decreased. This condition mainly affects young women. The basis for this is unknown; however our laboratory studies have shown that sex hormones play a role in gastroparesis by way of nitric oxide [8]. Studies have also shown that CGRP increases as a result of increased female sex hormones [9-11]. Thus, we speculate Calcitonin Gene-Related Peptide, or CGRP, may also play a role in regulating gastric motility functions, either independently or via sex hormones.
Calcitonin Gene-related Peptide
Calcitonin-gene related peptide, or CGRP, is a 37 amino acid neuropeptide. It is present in two forms, α-CGRP and β-CGRP. These forms differ by three amino acids in humans, with α-CGRP being derived from calcitonin and β-CGRP being encoded by a different gene [12]. CGRP is a neurotransmitter from capsaicin-sensitive neurons. Capsaicin is the active ingredient in chili peppers that gives them their “hot” sensation [13]. Synthesis of CGRP begins in the dorsal root ganglion (DRG), which also houses the capsaicin-sensitive sensory neurons. The synthesis of CGRP is regulated by activation of the capsaicin receptor, Transient Receptor Potential Vanilloid Subtype 1 (TRPV1). This activation can be achieved by harmful temperatures, acidic extracellular pH, lipids, and vanilloid molecules. Once TRPV1 is activated, CGRP is then synthesized and released by the capsaicin-sensitive inhibitory sensory neurons to other parts of the body. Synthesis and release of CGRP is also known to be regulated by other factors such as nerve growth factor (NGF), arachidonic acid derivatives, vascular wall tension, and others [14].
CGRP is present throughout the body in locations such as blood vessels, smooth muscles, and nerve plexuses [12,15]. Published reports have shown that the receptor for CGRP is Calcitonin Receptor-like Receptor (CRLR); however it cannot act alone and must be complexed to an accessory protein, Receptor Activity Modifying Protein 1, or RAMP1. The complex of CRLR and RAMP1 is the receptor complex for regulation of CGRP. When CGRP binds to its receptor complex, it becomes active [16]. CGRP carries out functions in various body systems such as the respiratory, cardiovascular, and gastrointestinal systems [14]. This review will focus on its function in the gastrointestinal system as it relates to gastroparesis.
Localization of CGRP in the gut
In the stomach, CGRP has been shown to be localized in the gastric mucosa, the longitudinal muscles, and the myenteric plexus [15]. The myenteric and the submucosal plexuses together make up the ENS.7 The ENS regulates the gastrointestinal motility functions.6 Functions of CGRP in these locations include vasodilation and muscle relaxation [13,16]. CGRP is currently the most potent vasodilator known [14].
CGRP is present in many different places in the body [12]. In the gastrointestinal system, it is present in the capsaicin-sensitive afferent neurons. These capsaicin-sensitive neurons, when activated by capsaicin, have been found to cause contraction of the longitudinal muscles [13].
Contraction of the longitudinal muscles is essential for the passage of food through the gastrointestinal system.
Gastroparesis and CGRP
Gastroparesis is a medical condition in which the stomach is partially paralyzed [5]. As a result, food takes a much longer time to travel through the stomach and reach the small intestine. This process could be influenced by CGRP in various ways. Normally, CGRP is present in the Delta (D) cells of the gastric mucosa. There, CGRP controls the synthesis and secretion of substances, one being somatostatin. Somatostatin, also known as GHIH, is a hormone produced partially in the periventricular nucleus of the hypothalamus. When released, it inhibits the secretion of gastric acid [12]. Accordingly, we speculate that changes in CGRP would result in changes in somatostatin synthesis and release, resulting in changes in gastric acid secretion, thus, CGRP may indirectly control the release of gastric acid, which is an essential part of the gastric emptying process. Therefore, CGRP could be a factor in slower gastric emptying; however, a connection between CGRP and gastroparesis has not been established and can be a focus in future research.
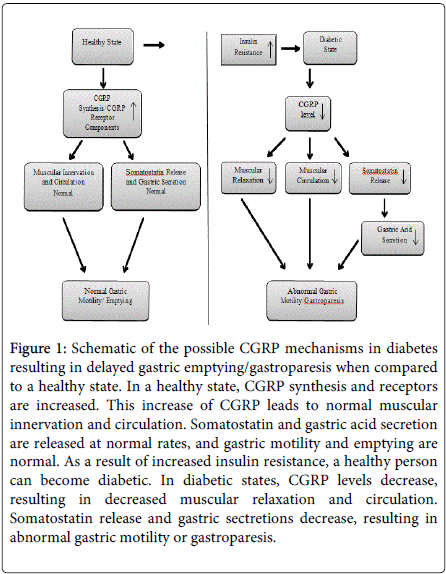
In a healthy state, during the gastric emptying process, food travels through the stomach. In order for this to happen, the longitudinal and circular muscles of the stomach have to contract [12] and relax. CGRP has been shown to cause increased smooth muscle relaxation and decreased muscular contraction [12]. Since CGRP levels are reduced [17,18] in diabetic serum and stomachs (Figure 1); we speculate that it could lead to abnormal gastric motility thus gastroparesis as we have noticed with reduced nitric oxide synthesis [19]. A relationship between CGRP, gastric muscular innervation, and gastroparesis has also not been established and can be a focus in future research.
As earlier stated, the ENS regulates the gastrointestinal system [6]. The ENS consists of two components, an extrinsic component, and an intrinsic component. The extrinsic component is comprised of autonomic divisions, parasympathetic and sympathetic. The intrinsic component is made up of millions of neurons, including the myenteric plexus and the two layers of submucosal plexuses. The neurons of the myenteric plexus are responsible for the innervation to the muscle layers [6]. We speculate that CGRP localized in these areas may play a critical role in maintaining normal stomach motility and emptying processes. A change in the synthesis of CGRP could lead to gastroparesis in the onset of diabetes.
In diabetes, serum and stomach CGRP has been found to be reduced as compared to people without diabetes [17,18]. Decreases in CGRP could result in decreased vasorelaxation, which could in turn result in a decreased blood circulation to the muscles needed for gastric emptying (Figure 1). However, it is not known whether decreased serum or gastric CGRP contributes to the pathogenesis of diabetic gastroparesis. There is currently little research on the pathology of idiopathic gastroparesis [20].
Figure 1: Schematic of the possible CGRP mechanisms in diabetes resulting in delayed gastric emptying/gastroparesis when compared to a healthy state. In a healthy state, CGRP synthesis and receptors are increased. This increase of CGRP leads to normal muscular innervation and circulation. Somatostatin and gastric acid secretion are released at normal rates, and gastric motility and emptying are normal. As a result of increased insulin resistance, a healthy person can become diabetic. In diabetic states, CGRP levels decrease, resulting in decreased muscular relaxation and circulation. Somatostatin release and gastric sectretions decrease, resulting in abnormal gastric motility or gastroparesis.
Methodology and Findings
Database searches were conducted using title words and key words. Studies were evaluated and summarized in a narrative review. To guard against biased reporting, we chose and evaluated studies that stated concepts clearly and had concise conclusions. We also did not evaluate meta-analyses, as they can potentially contain discrepant results. The following databases were used to search for relevant articles:
• PubMed incl. MEDLINE by OVID
• ScienceDirect by Elsevier
• SciVerse by Elsevier
• EMBASE by Elsevier
• Evidence Based Medicine (EBM) reviews
• Web of Science by Thomson Reuters
Our hypothesis was as follows: In a state of diabetes and hyperlipidemia, the expression of the CGRP receptors CRLR, RAMP1 and Adrenomedullin receptor RAMP2 will be decreased. Based on the literature available we conclude that CGRP may play a significant role in improving gastroparesis. However more studies need to be conducted in preclinical animal models to prove our hypothesis.
Pharmacological studies have shown that intervention affecting CGRP and Adrenomedullin receptors have had an effect on gastroparesis. Luo and others found that using an antagonist of the CGRP receptor increases gastric blood flow, thus promoting gastric motility, and supporting the hypothesis that altering the expression of receptors affects the gastroparesis seen in diabetes and hyperlipidemia. In contrast, Cottrell and others also found that employing a CGRP receptor antagonist halted contraction and relaxation, thus possibly slowing motility, possibly contributing to gastroparesis. Due to these conflicting studies, more studies should be conducted to prove our hypothesis.
Conclusions
According to the discussed literature, having inadequate amounts of CGRP appears to be pathogenic. In healthy females, CGRP levels are higher; but, stomach emptying is slower when compared with men [19]. However, in diabetes, CGRP levels decrease, therefore, it could be leading to the pathogenesis of gastroparesis [17,18]. More in-depth studies are warranted to investigate the role of CGRP in both health and disease. Future research should first focus on the levels of CGRP and CGRP receptor components in diabetic/idiopathic patients. Next, research should examine the gastric functions in these patients as it relates to these CGRP levels and sex steroid hormones. This can assist in establishing another cause of gastroparesis and be beneficial in developing treatments.
Acknowledgements
We thank the Meharry Medical College Center of Excellence for providing the stipend for the medical student.
References
- Buckles DC, McCallum RW (2003) New approaches for gastroparesis. Advanced Studies in Medicine 3: 39-44.
- (2014) American Diabetes Association Genetics of diabetes.
- (2014) American Diabetes Association Type 1diabetes.
- Asghar S, Claussen B, Hussain A, Hydrie M.Z.I (2010) Type 2 diabetes and obesity: A review. Journal of Diabetology 2: 1-7.
- Gangula PR, Chinnathambi V, Hale AB, Mukhopadhyay S, Channon KM, et al. (2011) Impairment of nitrergic system and delayed gastric emptying in low density lipoprotein receptor deficient female mice.Neurogastroenterol Motil 23: 773-773e335.
- Altaf MA, Sood MR (2008) The nervous system and gastrointestinal function.Dev Disabil Res Rev 14: 87-95.
- Yin J, Chen JD (2010) Gastrointestinal motility disorders and acupuncture.Auton Neurosci 157: 31-37.
- Ravella K, Al-Hendy A, Sharan C, Hale AB, Channon M,et al. (2013) Chronic estrogen deficiency causes gastroparesis by altering neuronal nitric oxide synthase function. Digestive Diseases and Sciences 58: 1507-1515.
- Thota C, Yallampalli C (2005) Progesterone upregulates calcitonin gene-related peptide and adrenomedullin receptor components and cyclic adenosine 3’5’-monophosphate generation in Eker rat uterine smooth muscle cell line. Biology of Reproduction 72: 416-422.
- Gangula PR, Lanlua P, Bukoski RD, Wimalawansa SJ, Yallampalli C (2004) Mesenteric arterial relaxation to calcitonin gene-related peptide is increased during pregnancy and by sex steroid hormones.Biol Reprod 71: 1739-1745.
- Gangula PR, Chauhan M, Reed L, Yallampalli C (2009) Age-related changes in dorsal root ganglia, circulating and vascular calcitonin gene-related peptide (CGRP) concentrations in female rats: Effect of female sex steroid hormones. Neuroscience Letters 454: 118-123.
- Ghatta S, Nimmagadda D (2004) Calcitonin gene-related peptide: Understanding its role. Indian Journal of Pharmacology 36: 277-283.
- Bartho L, Benko R, Holzer-Petsche U, Holzer P, Undi S (2008) Role of extrinsic afferent neurons in gastrointestinal motility. European Review for Medical and Pharmacological Science 12: 21-31.
- Luo X, Liu B, Dai Z, Yang Z, Peng J (2013) Stimulation of calcitonin gene-related peptide release through targeting capsaicin receptor: A potential strategy for gastric mucosal protection. Digestive Diseases and Sciences, 58, 320-325.
- Cottrell GS, Alemi F, Kirkland JG, Grady EF, Corvera CU, et al. (2012) Localization of calcitonin receptor-like receptor (CLR) and receptor activity-modifying protein 1 (RAMP1) in human gastrointestinal tract.Peptides 35: 202-211.
- Chauhan M, Gangula PR, Wimalawansa SJ, Yallampalli C (2004) Studies on the effects of the N-terminal domain antibodies of calcitonin receptor-like receptor and receptor activity-modifying protein 1 on calcitonin gene-related peptide-induced vasorelaxation in rat uterine artery.Biol Reprod 70: 1658-1663.
- Wang LH, Zhou SX, Li RC, Zheng LR, Zhu JH (2012) Serum levels of calcitonin gene-related peptide and substance p are decreased in patients withdiabetesmellitusandcoronaryarterydisease.JournalofInternationalMedical Research 40: 134-140.
- Selim MM, Wendelschafer-Crabb G, Redmon JB, Khoruts A, Hodges JS (2010) Gastric mucosal nerve density: A biomarker for diabetic autonomic neuropathy? Neurology 75: 973-981.
- Gangula PR, Sekhar KR, Mukhopadhyay S (2011). Gender bias in gastroparesis: Is nitric oxide the answer? Digestive Diseases and Sciences 56: 2520-2527.
- Zárate N, Mearin F, Wang XY, Hewlett B, Huizinga JD (2003) Severe idiopathic gastroparesis due to neuronal and interstitial cells of Cajal degeneration:pathological findings and management Gut 52: 966-970.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 18849
- [From(publication date):
April-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 14130
- PDF downloads : 4719