Risk Variables of Neonatal Clavicular Fracture and the Role of Ultrasound in Its Diagnosis
Received: 20-Jun-2018 / Accepted Date: 18-Jul-2018 / Published Date: 24-Jul-2018 DOI: 10.4172/2572-4983.1000160
Keywords: Newborn; Clavicular Fracture; Ultrasound
Introduction
Birth trauma is one of the main causes of neonatal morbidity and mortality [1,2]. Fracture of the clavicle occurs in up to 4.5% of vaginal births and accounts for approximately 90% of all obstetrical fractures with equivalent sex and side distribution [3-5]. The clavicle is easily fractured because of its subcutaneous, relatively anterior location and frequent exposure to transmitted forces. Also, the lack of muscular and ligamentous support makes it more vulnerable to injury [6]. The diagnosis is suspected by clinical examination and confirmed by plain radiographs [7]. Although displaced clavicular fractures are relatively easily diagnosed clinically, non-displaced fractures may be apparent only after callus formation or if all neonates are subjected to radiography or ultrasonography, or multiple physical examinations [8,9]. A fractured clavicle in a newborn can often be difficult to diagnose because it is often asymptomatic and can also be confused with other common diagnoses such as brachial plexus palsy, congenital pseudoarthrosis, and congenital muscular torticollis [10]. The most common sign is lack of active, spontaneous movement of the affected upper extremity arm. Crepitus, a palpable bony abnormality, or discoloration over the fracture site and asymmetric Moro reflex may be observed [11]. Neonatal clavicle fractures generally heal uneventfully, can be treated non-operatively and have an overall excellent prognosis [4]. An apparent fracture of the clavicle at birth does not always indicate birth trauma, since neonatal injury can also occur after normal vaginal delivery or cesarean section in the absence of an obvious traumatic delivery. It has been suggested that some clavicular fractures may be the result of preexisting fetal conditions rather than any unusual forces exerted at delivery [1,5,9,12]. Syndromes involving chromosomes 11, 18, and 22 have been reported with congenital defects of the clavicle, and congenital pseudarthrosis of the clavicle may be present at birth [13]. Many studies were performed to clarify the possible risk factors for birth fractures of the clavicle [4,5,12,14,15]. In recent years, US has already been used to diagnose neonatal clavicle fractures [8]. Because US may show poorly ossified neonatal bones better than radiographs, displaying indirect signs of fracture, such as signs of hematoma or detachment of the periosteum, evaluation of soft tissue such as muscle edema, tendon and joint functions, localizing the interposition of soft tissues between fracture fragments preoperatively and because it lacks ionizing radiation; this technique seems to be an excellent alternative to radiography [16]. The aim of the current study was to analyze the incidence of fracture of clavicle in newborn infants following normal delivery, the associated risk factors and the evaluation of the accuracy of ultrasonography (US) in diagnosing this fracture.
Patients and Methods
This observational prospective study was conducted in AL-Khafji Joint Operation (KJO) Hospital, Kingdom Of Saudi Arabia during the period from August 2013 to September 2016. During this period, there were no changes in the institutional policy regarding management of delivery or the criteria for diagnosis of neonatal clavicular fracture. From 7560 deliveries during the period of the study (5120 vaginal deliveries and 2440 CS), 48 cases diagnosed clinically and radiologically with fracture clavicle of them 43cases were included in our study as we excluded 2 cases delivered by cesarean section, one case with osteogenesis imperfect and 2 patients with multiple congenital anomalies.
Inclusion criteria: Database of the Departments of Neonatology and Obstetric was reviewed for all cases delivered by spontaneous vaginal delivery in the occipito-anterior position and singleton-term pregnancy. Exclusion criteria: Babies delivered by CS and those with multiple deformities.
All variables were compared with a control group of an equal number of healthy infants born immediately before or after each affected infant and delivered by the same obstetrical team.
All newborns included in the study undergo routine physical examination twice during the first 24 h of birth and later before discharge from the hospital. In the postnatal period, the infants were followed up at the neonatology outpatient clinic for various problems including monitoring for jaundice and feeding problems.
Diagnostic criteria for neonatal clavicular fracture include inspection for asymmetry of the clavicular bones, absence of the supraclavicular notch and local edema or hematoma; by palpation for crepitus and local tenderness reflected by the baby’s cry.
All the clinically suspected cases of clavicular fracture were confirmed diagnosis by plain-X ray. Blind ultrasonography (US) was done to all confirmed cases to evaluate its accuracy in diagnosing this fracture
Data collected for analysis included the following:
1. Prenatal history: Maternal age, height, weight, parity, presence of gestational diabetes and sonographic fetal weight estimation and gestational age.
2. Perinatal history: Premature rupture of the membranes, shoulder dystocia, induction of labor, duration of second stage, defined as the time from full dilatation to delivery, the need for oxytocic augmentation of uterine contractions, use and type of analgesia or anesthesia and performance of episiotomy.
3. Postnatal examination: Apgar score at 1 and 5 minutes, infant sex, measurements including birth weight, length and head circumference, presence of neonatal morbidity including Erb palsy and birth trauma
Radiological assessment:
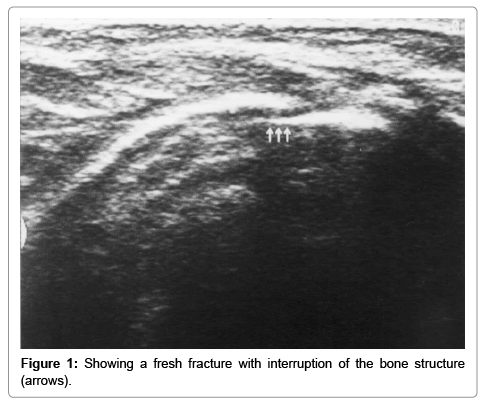
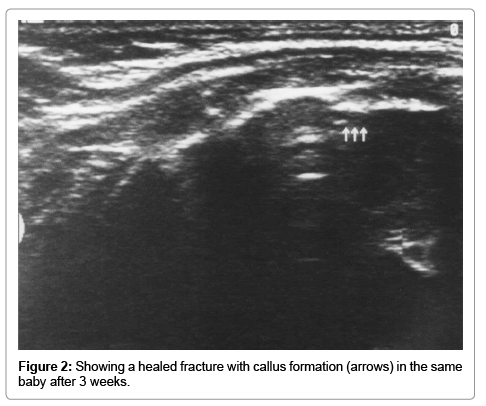
Conventional standard radiographs were done to all cases suspected clinically to have clavicular fracture. Real-time ultrasound examination was carried out in all suspected cases by radiology consultant with a standard US machine (Samsung Medison SonoAce X8, Korea) equipped with a small 7.5 MHz linear array Transducer using longitudinal views aligned to the clavicle. Discontinuity, axial deviation, periosteal lesions, hematomas and soft-tissue changes were recorded. During the examination, the infant was laid on his or her back so that the operator was looking down on the shoulder. The mother held the arm. Both shoulders were examined, starting with the clinically unaffected side. Callus, as a sign of bone healing, could be seen with time in all patients. The mean age of the infants at the time of ultrasound examination was two days and when a fracture was detected, the infant was re-examined clinically and by ultrasound at six weeks of age by orthopedic physician.
Statistical Analysis
Data were presented as mean ± standard deviation (X ± SD) or percentage (%). The means of two groups were compared using student’s t test. The odds ratio (OR) and 95% confidence interval (95% CI) were calculated for clavicular fracture susceptibility in relation to the studied risk factors. All data were analyzed using Epi Info statistical software, version 6.2 (WHO, Geneva, Switzerland) and Statistical Package for Social Sciences, version 22.0 (IBM Corp., Armonk, NY, USA).
P value <0.05 was considered statistically significant.
Results
Our study enrolled 43 cases delivered vaginally (0.84 % of all vaginal deliveries) with confirmed clavicular fracture clinically and radiologically. Twenty-five patients had fracture in the right side while 18 were on the left side with the medial third fracuture affected in all patients. Of these patients 20 were females (46.5%) and 23 were males (53.5 %). The control group were age, sex, and ethnicity-matched to patients (P>0.05).
The peripartum characteristics of the studied groups are shown in Table 1. There were no statistically significance difference between cases and controls groups regarding maternal age (30.9 ± 7.4 versus 31.2 ± 5.5 years), parity (2.2 ± 1.4 versus 2.1 ± 1.8 deliveries) and maternal weight (66.7 ± 9.2 versus 68.3 ± 8.5 kg). On the other hand, significant differences were found between the 2 groups regarding maternal height, the duration of second stage of labor, peripartum sonographic fetal weight estimation and neonatal birth length (P<0.05) (Table 1).
| Risk factor | Total | Proportion exposed (n,%) | OR | 95% CI | P value |
|---|---|---|---|---|---|
| Shoulder dystocia | |||||
| Cases | 43 | 11 (0.26) | 7.05 | 1.46-34.08 | 0.01 |
| Controls | 43 | 2 (0.045) | |||
| Birth weight >4000 g | |||||
| Cases | 43 | 13 (0.30) | 4.2 | 1.25-14.27 | 0.02 |
| Controls | 43 | 4 (0.09) | |||
| Gestational age >40 weeks | |||||
| Cases | 43 | 10 (0.24) | 4.04 | 1.026-15.9 | 0.045 |
| Controls | 43 | 3 (0.07) | |||
| Prolonged 2nd stage of labor | |||||
| Cases | 43 | 9 (0.20) | 5.4 | 1.1-26.8 | 0.038 |
| Controls | 43 | 2 (0.046) | |||
| Nulliparity | |||||
| Cases | 43 | 15 (0.35) | 0.9 | 0.37-2.18 | 0.8 |
| Controls | 43 | 16 (0.37) | |||
| Instrumental delivery | |||||
| Cases | 43 | 3 (0.07) | 1.36 | 0.3-6.5 | 0.7 |
| Controls | 43 | 2 (0.046) | |||
P value<0.05 indicates a significant difference.
Table 1: Peripartum characteristics of the studied groups.
Table 2 demonstrates the prevalence of the risk factors for neonatal clavicular fracture in patients and controls. The risk of clavicular fracture was significantly higher among patients with birth weight greater than 4000 g (OR: 4.2; 95% CI: 1.25 - 14.27; P=0.02), estimated gestational age greater than 40 weeks (OR: 4.04; 95% CI: 1.026 - 15.9; P=0.045), with shoulder dystocia delivery (OR: 7.05; 95% CI: 1.46 - 34.08; P=0.01), and those with history of prolonged second stage of labor (OR: 5.4; 95% CI: 1.1 - 26.8; P=0.038). However, we did not observe any significant association of nulliparity and instrumental delivery with fracture clavicle. Unfortunately, one baby was diagnosed with Erb’s palsy that complicated clavicular fracture with partial resolution at the 6-week follow up. All other cases healed completely without complications.
| Characters | Study group (Χ ± SD) | Control group (Χ ± SD) | t-test | P-value |
|---|---|---|---|---|
| Maternal height (cm) | 160.4 ± 6.6 | 164.3 ± 5.5 | 2.97 | 0.003 |
| Maternal weight (kg) | 66.7 ± 9.2 | 68.3 ± 8.5 | 0.84 | 0.4 |
| Maternal age (years) | 30.9 ± 7.4 | 31.2 ± 5.5 | 0.2 | 0.8 |
| Parity | 2.2 ± 1.4 | 2.1 ± 1.8 | 0.29 | 0.77 |
| Second stage duration (min) | 33.4 ± 34.7 | 20.2 ± 24.5 | 2.04 | 0.044 |
| Estimated fetal weight (gm) | 3621 ± 393 | 3312 ± 482 | 3.26 | 0.001 |
| Neonatal length (cm) | 50.5 ± 1.7 | 49.2 ± 1.8 | 3.44 | 0.009 |
OR: Odds Ratio; CI: Confidence Interval.
P-value<0.05 indicates a significant difference.
Table 2: Distribution of the risk factors of clavicular fracture in patients and controls.
To assess the value of ultrasound in the diagnosis of clavicular fractures, all 43 confirmed cases with neonatal clavicular fracture underwent US clavicles. Analysis of ultrasonographic (US) findings revealed that 18 cases had the characteristic signs of a greenstick fracture (Non-displaced fractures) while 23 patients had complete fractures. The US findings are shown in Table 3. Two cases (5%) revealed no fracture clavicle by ultrasonography although radiographs showed cortical swelling similar to a torus fracture in one case and a faint hairline fracture in the other one. The main radiological findings were interruption of the hyperechoic zone of the clavicle (95%), hypoechoic zone of haematoma (93%) and steps and axial deviation (91%).
| Ultrasonographic findings | n (43), (%) |
|---|---|
| Interruption of the hyperechoic zone of the clavicle | 41 (95) |
| Hypoechoic zone of haematoma | 40 (93) |
| Steps and axial deviation | 39 (91) |
| Visible periosteal lesions | 32 (74) |
| Visible dislocation of bone ends during breathing | 23 (53) |
| Normal finding | 2 (5) |
Table 3: US findings in patients group with radiograph confirmed fracture clavicle.
The sensitivity and specificity of ultrasound in the detection neonatal clavicular fracture were 95.35% (95% confidence interval [CI], 84.19%-99.43%) and 97.50% (95% CI, 86.84%-99.94%) respectively, and the positive and negative predictive values were 97.62% (95% CI, 85.53%-99.65%) and 95.12% (95% CI, 83.43%-98.69%), respectively. Overall, ultrasound Accuracy was 96.39% (95% CI, 89.80%-99.25%) (Table 4, Figures 1 and 2).
| Radiographs | Sensitivity (95%CI) | Specificity (95%CI) | PPV (95%CI) | NPP (95%CI) | Accuracy (95%CI) | |||
|---|---|---|---|---|---|---|---|---|
| True Fracture | True Non Fracture | |||||||
| US | Fracture (+ve test) | 41 (true+ve) | 1 (false+ve) | 95.35% (84.19-99.43%) | 97.50% (86.84-99.94%) | 97.62% (85.53-99.65%) | 95.12% (83.43-98.69%) | 96.39% (89.80-99.25%) |
| Non fracture (-ve test) | 2 (false-ve) | 39 (true-ve) | ||||||
US: ultrasound, PPV: Positive Predictive Value, NPP: Negative Predictive Value.
Table 4: Performance of US in the detection of clavicular fractures compared with X-ray as a standard.
Discussion
The clavicle is the most frequently fractured bone during birth [3,12]. Newborn infants with clavicular fracture rarely have symptoms and most have no long-term problem. Many obstetrical services use fracture of the clavicle as an indicator for quality review of the patient’s care. Furthermore, both the legal and medical communities have tended to equate clavicular fracture with obstetrical mismanagement [5,9]. Birth fracture of the clavicle should be suspected by the presence of risk factors, lack of use of the upper extremity, asymmetrical moro reflex and deformity or tenderness of the clavicle. The condition is made by physical examination and, if necessary, confirmed by radiographs [11].
In our study, Forty-three cases of clavicular fracture were identified among the 5120 vaginal deliveries during the period from August 2013 to September 2016 with an incidence of 0.84%.
In several other studies, the incidence of neonatal clavicular fractures varied from 0.2%, 1.5%, 1.87%, 3.2% to 4.5% [14,15,17-20]. The difference in incidences between centers can be explained by that the obstetric neonatal clavicular fracture is not always diagnosed at birth and approximately 40% of clavicular fractures are not identified until after discharge [21].
Although the fracture clavicle generally heals well without long-term sequelae, our study revealed one baby out of 43 cases of clavicular fracture (2.3%) with Erb’s palsy. In a 5-year retrospective study involving 5847 live births, one of the 60 (1.7%) newborns with clavicular fracture had Erb’s palsy [21]. In another retrospective review of 21,632 live births, clavicular fracture was found in 58 newborns, three (5.2%) of whom had concurrent Erb palsy with good recovery [22]. In a survey of 11,636 neonates admitted to the neonatal nursery, 2.29% had clavicular fracture, and 0.44% had Erb’s palsy [4]. As Erb’s palsy is not our concern in this study, and this incidence may not be true for Erb’s palsy because of small sample size.
A second stage of labor of more than 20 minutes has been associated with shoulder dystocia and possibly birth injuries [23]. In our study, there is positive correlation between the duration of second stage of labor and the incidence of clavicular fracture. These findings were going with the study of Kaplan et al. in which clavicular fracture rate was 1.65% [5], and they found that several variables including duration of second stage of labor, peripartum sonographic fetal weight estimation and neonatal birth length were positively correlated with neonatal clavicular fracture Regarding maternal height, our study revealed that short stature of the mother is another risk factor for clavicular fracture, which can be explained by that low maternal height, is associated with contracted pelvis and obstructed labor with increased incidence of birth trauma and clavicular fracture. In a study done by Gudmundsson et al. [24] they found a highly significant relationship between newborn birth weight and maternal height and the frequency of complications. The criterion for maternal short stature should be definitely based on ethnic groups and must be categorized according to height percentile range rather than absolute height may allow comparison between different populations on the effect on labor outcome [25]. In the present study, no association was found between maternal ages and weight with increasing the risk of neonatal clavicular fracture. Our results were going with the study of Poggi et al. who did not show an independent association between maternal obesity and neonatal birth injury [26]. However, Cedergren et al. found an association between morbidly obese mothers and increased risk of shoulder dystocia and birth injury [27]. Also a study by Ahn et al. concluded that major risk factor of clavicle fracture was vacuum delivery, mother with advanced age and high birth weight [28]. In the present study, we found that macrosomia, birth weight greater than 4000 g, and birth length of more than 52 cm were significantly associated with higher risk of neonatal clavicular fracture. Ozdener et al. showed that birth weight of over 3500 g and to a greater extent over 4000 g, were found to be an independent important factor associated with clavicle fracture [29]. Similar finding was reported by Lai et al. who showed macrosomic babies with birth weight of 4000 g to 4999 g has significant risk factor to developed lavicle fractures [30]. In our study, we found that the incidence of the neonatal clavicular fracture during labor was significantly increased with shoulder dystocia. Mehta et al. [23] concluded in their study that maternal obesity in their population was associated with an increased risk of neonatal injury after shoulder dystocia. During 5-year period, they recorded 206 cases of shoulder dystocia out of 25995 deliveries. Of these, there were 19 cases of Erb’s palsy and 6 cases of clavicular fracture. On the other hand, Beall and Ross [12] in their study was unable to demonstrate an association between clavicular fracture and shoulder dystocia., and reported in their study that neonatal clavicle fracture is associated with infant birth weight greater than 4 kg, but not with the occurrence of objectively defined shoulder dystocia. Also, beall et al. [31] found no correlation between clavicular fracture and shoulder dystocia and they reported that the association with shoulder dystocia may be false or intentional because of an increased tendency to report a shoulder dystocia in a delivery in which a birth injury has been identified. In the present study, we found that increasing gestational age is also positively correlated with clavicular fracture. However, it loses its significance as risk factor when comparing with shoulder dystocia and birth weight. This result is going with results of Roberts et al. who found that gestational age is a risk factor for clavicular fracture at 40 and 41 weeks; and at 42 weeks or greater in stratified analysis considering only gestational age [1]. In this study, we could not confirm that neonatal clavicular fracture was associated with instrumental deliveries (forceps or vacuum extraction). However, A study done by Lam et al. in which they reported 151 of 9540 (1.6%) clavicle fractures occur in their series and it was associated with increased incidence of instrumental delivery and shoulder dystocia [32]. Oppenheim also demonstrated that forceps deliveries and shoulder dystocia have a higher risk to develop clavicle fracture and brachial plexus injury [22]. In our series, we observed, no relation between maternal parity and neonatal clavicular fracture. Same results were found in Hassib et al. study who found an equal number of fracture clavicle cases in both multiparous and nulliparous [33]. On the other hand, Brown found that nulliparous has a higher risk compared to multiparous in developing neonatal clavicle fractured.
Recent studies have focused on the reliability and interest of US for the diagnosis of clavicular fractures in children [34]. One of the first studies of the use of ultrasound for the diagnosis of fractures in the neonate was published by Katz et al, who studied Forty-one cases of clavicle fracture in newborn babies [35]. The babies were examined by both radiographic and ultrasonic methods and they concluded that no substantial difference has been found between these two modalities. They suggested that ultrasound should be the procedure of choice in the diagnosis of clavicle fracture. In our study, we examined the accuracy of US in diagnosing a neonatal clavicular fracture in comparison to X-ray. Overall, sensitivity, specificity, PPV, and NPV of on-site US were, respectively, for the presence (or absence) of fractures: 95.35%, 97.5, 97.62% and 95.12%. US accuracy was 96.39%. One false positive and two false-negative US examinations were found. The three cases of disagreement (false-positives and false-negatives) needed second review of the findings but we did not provide a second reviewer of our primary ultrasound. Our findings are consistent with the results of the study done by balb et al. in which Forty-nine infants with clavicular fractures were examined radiologically and sonographically by independent examiners; and reported that US diagnosis of clavicle fractures in older children in an orthopedic clinic with high diagnostic accuracy 96% for US versus 91% for radiographs [36]. Also, Keith et al. in their study concluded that bedside ultrasound in the pediatric ED can accurately diagnose clavicle fractures when compared to plain radiographs [37]. However, radiography is still indicated in cases of neurological injury and related palsy and for congenital pseudarthrosis of the clavicle [11].
Conclusion and Recommendation
Our study has several limitations. First, our protocol was based on conventional radiography and not US as the gold standard for diagnosis of neonatal clavicular fractures. Second, all exams were done by trained musculoskeletal radiologists and it could be valuable to have a dedicated US course to evaluate the learning curve of junior radiologists. Finally, a larger patient population would probably have increased the statistical power of our results.
In conclusion, shoulder dystocia and large birth weight remains the main risk factors for obstetric clavicular fracture, although most birth clavicular fracture are unavoidable and unpredictable and the majority occur in uncomplicated normal vaginal deliveries. Given its diagnostic accuracy, minimal pain during examination, and lack of ionizing radiation. Bedside clavicular sonography, when performed by trained radiologists, is an excellent method for confirming a suspected fracture of the clavicle in the neonate when compared to radiography and thus US could be recommended for routine use in NICU in selected cases to avoid radiation exposure. Additional randomized clinical studies comparing US to radiography will be of great interest to consolidate clinical practice.
References
- Roberts SW, Hernandez C, Mabbery MC, Adams MD, Leveno KJ, et al. (1995) Obstetric clavicular fracture: the enigma of normal birth. Obstet Gynecol 86: 978-981.
- Al-Qattan MM, Clarke HM, Curtis CG (1994) The prognostic value of concurrent clavicular fractures in newborns with obstetric brachial plexus palsy. J Hand Surg 6: 729-730.
- McBride MT, Hennrikus WL, Mologne TS (1998) Newborn clavicle fractures. Orthopedics 21: 317-320.
- Peleg D, Hasnin J, Shalev E (1997) Fractured clavicle and Erb’s palsy unrelated to birth trauma. Am J Obstet Gynecol 177: 1038-1040.
- Kaplan B, Rabinerson D, Averch OM, Carmi N, Steinberg DM (1998) Fracture of the clavicle in the newborn following normal labor and delivery. Int J Obstet Gynecol 63: 15-20.
- Pecci M, Kreher JB (2008) Clavicle fractures. Am Fam Physician 77: 65-70.
- Blankenstein A, Ganel A, Salai M (2001) Fracture of the clavicle in the newborn: detection and follow-up by sonography. Akt Traumatol 31: 27-29.
- Kayser R, Mahlfeld K, Heyde C, Grasshoff H (2003) Ultrasonographic imaging of fractures of the clavicle in newborn infants. J Bone Joint Surg Br 85: 115-116.
- Joseph PR, Rosenfeld W (1990) Clavicular fractures in neonates. Am J Dis Child 144: 165-167.
- Anderson K (2003) Evaluation and treatment of distal clavicle fractures. Clin Sports Med 22: 319-326.
- Alzen G, Duque-Reina D, Urhahn R, Solbach G (1992) Radiographic examination of injuries in children: clinical and legal considerations about indications. Dtsch Med Wochenschr 117: 363-367.
- Beall MH, Ross MG (2001) Clavicle fracture in labor: risk factors and associated morbidities. J Perinatol 21: 513-515.
- Beals RK, Sauser DD (2006) Nontraumatic disorders of the clavicle. J Am Acad Orthop Surg 14: 205-214.
- Many A, Brenner SH, Yaron Y, Lusky A, Peyser MR (1996) Prospective study of incidence and predisposing factors for clavicle fracture in the newborn. Acta Obstet Gynecol Scand 75: 378-381.
- Ohel G, Haddad S, Fischer O, Levit A (1993) Clavicular fracture of the neonates: Can it be predicted before birth? Am J Perinat 10: 441-443.
- Chen L, Kim Y, Moore CL (2007) Diagnosis and guided reduction of forearm fractures in children using bedside ultrasound. Pediatr Emerg Care 23: 528-531.
- Levine MG, Holroyde J, Woods JR, Siddiqi TA, Scot N (1984) Birth trauma-incidence and predisposing factors. Obstet Gynecol 63: 792-795.
- Turnpenny PD, Nimmo A (1993) Fractured clavicle of the newborn in a population with a high prevalence of grand multiparity: Analysis of 78 consecutive cases. Br J Obstet Gynaecol 100: 338-341.
- Walle T, Sorri AH (1993) Obstetric shoulder injury: Associated risk factors, prediction and prognosis. Acta Obstet Gynecol Scand 72: 450-454.
- Perlow JH, Wigton T, Hart J, Strassner HT, Nageotte MP (1996) Birth trauma. A five-year review of incidence and associated perinatal factors. J Reprod Med 41: 754-760.
- Gilbert WM, Tchabo JG (1988) Fractured clavicle in newborns. Int Surg 73: 123-125.
- Oppenheim WL, Davis A, Growdon WA, Dorey FJ, Davlin LB (1990) Clavicle fractures in the newborn. Clin Orthop 250: 176-180.
- Mehta SH, Blackwell SC, Bujold E, Sokol RJ (2006) What factors are associated with neonatal injury following shoulder dystocia? J Perinatol 26: 85-88.
- Gudmundsson S, Henningsson AC, Lindqvist P (2005) Correlation of birth injury with maternal height and birth weight. Br J Obstet Gynaecol 112: 764-767.
- Kara F, Yesildaglar N, Uygur D (2005) Maternal height as a risk factor for Caesarean section. Arch Gynecol Obstet 271: 336-337.
- Poggi SH, Stallings SP, Ghidini A, Spong CY, Deering SH (2003) Intrapartum risk factors for permanent brachial plexus injury. Am J Obstet Gynecol 189: 725-729.
- Cedergren MI (2004) Maternal morbid obesity and the risk of adverse outcome. Obstet Gynecol 103: 219-224.
- Ahn ES, Jong MS, Lee YK, Ko SY, Shin SM, et al. (2015) Neonatal clvicular fracture: Recent 10 year study. Paediatrics International 57: 60-63.
- Ozdener T, Engin-Ustun Y, Aktulay A, Turkcapar F, Oguz S (2013) Clavicular fracture: its prevalence and predisposing factors in term uncomplicated pregnancy. Eur Rev Med Pharmacol Sci 17: 1269-1272.
- Lai SF, Lo TK, Lam YY, Lau WL, Leung WC A Five-year study on maternal characteristics and Neonatal outcomes of clavicular fractures in the newborns: Another piece of reassurance. J Gynaecol Obstet Midwifery 14: 24-30.
- Beall MH, Spong C, McKay J, Ross MG (1998) Objective definition of shoulder dystocia: a prospective evaluation. Am J Obstet Gynecol 179: 934-937.
- Lam MH, Wong GY, Lao TT (2002) Reappraisal of neonatal clavicular fracture: relationship between infant size and neonatal morbidity. Obstet Gynecol 100: 115-119.
- Hassib N, Naji K, Ekuma-Nkama E (1996) Clavicle fracture and brachial plexus palsy in the newborn: Risk factor and outcome. Annals of Saudi Medicine 16: 707-710.
- Brown BL, Lapinski R, Berkowitz GS, Holzman I (1994) Fractured clavicle in the neonate: a retrospective three-year review. Am J Perinatol 11: 331-333.
- Katz R, Landman J, Dulitzky F, Bar-Ziv J (1988) Fracture of the clavicle in the newborn: an ultrasound diagnosis. J Ultrasound Med 7: 21-23.
- Blab E, Geissler W, Rokitansky A (1999) Sonographic management of infantile clavicular fractures. Pediatr Surg Int 15: 251-254.
- Cross KP, Warkentine FH, Kim IK, Gracely E, Paul RI (2010) Bedside Ultrasound Diagnosis of Clavicle Fractures in the Pediatric Emergency Department. Acad Emerg Med 17: 687-693.
Citation: Awadef YF, Abdelsalam NI, Taha SA, Mohamed EA, Hassan MA, et al. (2018) Risk Variables of Neonatal Clavicular Fracture and the Role of Ultrasound in Its Diagnosis. Neonat Pediatr Med 4: 160. DOI: 10.4172/2572-4983.1000160
Copyright: © 2018 Awadef YF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8778
- [From(publication date): 0-2018 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 7893
- PDF downloads: 885