Risk Factors for Mortality among COVID-19 Patients: Nationwide Cohort Study of Mongolia
Received: 06-Feb-2023 / Manuscript No. DPO-23-88804 / Editor assigned: 09-Feb-2023 / PreQC No. DPO-23-88804 (PQ) / Reviewed: 23-Feb-2023 / QC No. DPO-23-88804 / Revised: 02-Mar-2023 / Manuscript No. DPO-23-88804 (R) / Accepted Date: 02-Mar-2023 / Published Date: 09-Mar-2023 DOI: 10.4172/2476-2024.8.1.210
Abstract
Background: Through this first large retrospective cohort study in Mongolia, we tried to provide some useful information for predicting the character of Coronavirus disease 2019 (COVID-19) patients.
Materials and methods: Adult inpatients with COVID-19 were retrospectively analyzed from national, provincial, and municipal health reports from April 1, 2020 to October 1, 2021.
Results: 554 non-survivor and 161 survivors, for a total of 715 patients were included in the final analysis. Female patients accounted for 51.5% of all patients. The mean age was 65.5 (18-100) years, and patients in the non-survivor group were much older than those in the survivor group (57 years vs. 69 years, p<0.001). Most of the cases in the non-survivor group had unvaccinated (139; 25%). The top five symptoms in all patients were cough (78.3%), dyspnea (74.5%), fever (39.9%), chest pain (46.3%), and fatigue (26.9%). Factors of comorbidity such as cardiovascular disease (p<0.001), hypertension (p<0.001), and cancer (p=0.003), were statistically significant. Patients with hypertension (OR: 5.065, 95% CI, 3.065-8.368, p<0.001) were significantly different between survivor and non-survivor groups.
Conclusion: Elderly, dyspnea, cough, chest pain, cardiovascular disease, and hypertension were the major predictors of COVID-19 patient mortality in the multivariate analysis. From these findings, improving the infection situation in Mongolian patients may require greater attention and improvement in the management of the character of patients in COVID-19 patients. However, in an environment with limited economic resources like our country, high costs could be restrictive in Mongolia.
Keywords: SARS-CoV-2; COVID-19; Risk factor; Mortality
Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the virus responsible for Coronavirus Disease 2019 (COVID-19), was transmitted to humans in Wuhan, China reported on November 17, 2019 [1-5]. Due to the lack of data in one of the most influenced areas by the COVID-19 pandemic, the result of Mongolia profits the management. Mongolia is the region with a high prevalence of non- communicable diseases, which are risk factors for SARS-CoV-2 infection [6,7]. COVID-19 is an emerging infectious disease with poor evidence associated with disease characteristics and seemed to be affected by multiple factors such as patient characteristics, geography, and difference in social systems [8-14]. The direction of the research is as follows. First, we focused specifically on Mongolian data, as most published reports on COVID-19 were from China, and patients’ characters associated with COVID-19 vary widely among geographic regions. Mongolia has a vast land area, and a diverse population, and is located in neighboring China where the SARS-CoV-2 infection occurred. COVID-19 has affected unequally in Mongolia compared to other countries. Therefore, it is necessary to adjust the risk of COVID-19 based on the situation in Mongolia. We have created data aimed at characterizing the SARS-CoV-2 infected patients who died in Mongolia. Through this first large retrospective cohort study in Mongolia, we tried to provide some useful information for predicting the character of COVID-19 patients.
Materials and Methods
Adult inpatients with COVID-19 were retrospectively analyzed from national, provincial, and municipal health reports from April 1, 2020 to October 1, 2021. All patients were laboratory-confirmed positive cases of SARS-CoV-2 by Real-Time Transcriptase-Polymerase Chain Reaction (RT-PCR) of nasopharyngeal swab samples. We excluded those under 18 years old, with incomplete medical records, and survivors. The study was approved by the Institutional Ethics Committee of the Mongolian National University of Medical Sciences (No2021/3-08).
Data collection
Demographic data about the age and sex of cases, as well as chronic comorbidities and date of symptoms onset, hospital admission, SARS-CoV-2 infection diagnosis confirmation, and death, were compiled. Risk factors of mortality, including sex, age, vaccination, symptoms, and comorbidities, were evaluated among COVID-19 patients.
Statistical analysis
Multivariable logistic regression was used to evaluate risk factors among patients using SPSS version 22.0 (SPSS Inc., Chicago, III, USA). Univariate analysis of categorical variables was performed using the Chi-square test, while an independent sample t-test/Mann-Whitney U test was used for continuous data. Multivariable analysis using logistic regression was performed for the factors found to be significant in the univariate analysis. Covariates with a P value ≤ 0.05 in the univariate analysis were included in the multivariate analysis. All statistical tests were two-sided and P ≤ 0.05 was considered significant.
Results
Clinical characteristics of cases can be shown in Table 1 and 2. 554 non-survivor and 161 survivors, for a total of 715 patients were included in the final analysis. Female patients accounted for 51.5% of all patients. The mean age was 65.5 (18-100) years, and patients in the non-survivor group were much older than those in the survivor group (57 years vs. 69 years, p<0.001). Most of the cases in the non-survivor group had unvaccinated (139; 25%). The top five symptoms in all patients were cough (78.3%), dyspnea (74.5%), fever (39.9%), chest pain (46.3%), and fatigue (26.9%). Factors of comorbidity such as cardiovascular disease (p<0.001), hypertension (p<0.001), and cancer (p=0.003), were statistically significant. In regression analysis are shown in Table 2. Older age (OR: 1.034, 95% CI: 1.018-1.051, p<0.001), patients with dyspnea (OR: 5.209; 95% CI, 3.218-8.433, p<0.001), patients with fever (OR: 0.489, 95% CI, 0.305–0.784, p<0.001), patients with headache (OR: 0.334; 95% CI, 0.205-0.543, p<0.001), patients with loss of taste and smell (OR: 0.142; 95% CI, 0.073–0.275, p<0.001), patients with sputum production (OR: 0.509; 95% CI, 0.283–0.917, p=0.025), and patients with sore throat (OR: 0.466; 95% CI, 0.251–0.865, p=0.016) were identified as significant between survivor and non-non-survivor groups. Patients with hypertension (OR: 5.065, 95% CI, 3.065-8.368, p<0.001) were significantly different between survivor and non-survivor groups. However, cardiovascular disease (OR: 1.184, 95% CI, 0.654-2.144 p=0.576) and cancer (OR: 0.772, 95% CI, 0.274–2.177, p<0.001) were not significant.
| Variable | Survivor (n=161) | non-Survivor (n=554) | p-value | |
|---|---|---|---|---|
| Age | - | 57 (26-96) | 69 (18-100) | <0.001 |
| - | Gender | 0.293 | ||
| Female | - | 77 (47.8%) | 291 (52.5%) | - |
| Male | - | 84 (52.2%) | 263 (47.5%) | - |
| Vaccination | <0.001 | |||
| Unvaccinated | - | 28 (17.3%) | 139 (25.0%) | - |
| Sinopharm | - | 42 (26.0%) | 361 (65.1%) | - |
| Pfizer | - | 10 (6.2%) | 20 (3.6%) | - |
| Sputnik V | - | 2 (1.2%) | 11(1.9%) | - |
| AstraZeneca | - | 2 (1.2%) | 8 (1.4%) | - |
| Unknown | - | 77 (48.1%) | 15 (3.0%) | - |
| Dyspnea | <0.001 | |||
| yes | 49 (47.3%) | 413 (74.5%) | - | |
| no | 112 (52.7%) | 141 (25.5%) | - | |
| Cough | 0.002 | |||
| yes | 107 (66.4%) | 434 (78.3%) | - | |
| no | 54 (33.6%) | 120 (21.7%) | - | |
| Fever | <0.001 | |||
| yes | 104 (64.6%) | 221 (39.9%) | - | |
| no | 57 (35.4%) | 333 (60.1%) | - | |
| Headache | <0.001 | |||
| yes | 74 (45.9%) | 126 (22.7%) | - | |
| no | 87 (54.1%) | 428 (77.3%) | - | |
| Chest pain | 0.04 | |||
| yes | 60 (37.2%) | 257 (46.3%) | - | |
| Symptoms | no | 101 (62.8%) | 297 (53.7%) | - |
| Fatigue | 0.377 | |||
| yes | 49 (30.4%) | 149 (26.9%) | - | |
| no | 112 (69.6%) | 405 (73.1%) | - | |
| Loss of taste and smell | <0.001 | |||
| yes | 57 (35.4%) | 28 (5.0%) | - | |
| no | 104 (64.6%) | 526 (95.0%) | - | |
| Sputum production | <0.001 | |||
| yes | 45 (27.9%) | 76 (13.7%) | - | |
| no | 116 (72.1%) | 478 (86.3%) | - | |
| Sore throat | <0.001 | |||
| yes | 38 (23.6%) | 62 (11.2%) | - | |
| no | 123 (76.4%) | 492 (88.8%) | - | |
| Diabetes mellitus | 0.713 | |||
| yes | 43 (26.7%) | 140 (25.2%) | - | |
| no | 118 (73.3%) | 414 (74.8%) | - | |
| Cardiovascular disease | 0.001 | |||
| yes | 26 (16.1%) | 162 (29.2%) | - | |
| Comorbidity | no | 135 (83.9%) | 392 (70.8%) | - |
| Hypertension | <0.001 | |||
| yes | 26 (16.1%) | 313 (56.5%) | - | |
| no | 135 | 241 (43.6%) | - | |
| Cancer | 0.003 | |||
| yes | 20 (12.4%) | 31 (5.6%) | - | |
| no | 141 (87.6%) | 523 (94.4%) | - | |
Table 1: Comparisons of clinical characteristics between the survivor and non-survivor 19 (n=715)
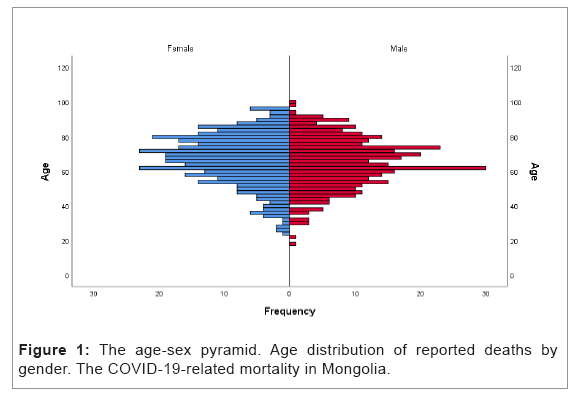
Of the 667 trackable cases shown that 667 cases were x-rayed, and 127 were Computed Tomography (CT) (Table 3). In contrast, there was no Magnetic Resonance Imaging (MRI). 554 patients had performed x-ray of these, 553 (99.82%) patients with abnormalities in the non-survivor group. Of the 77 chest CT scans, 76 (98.7%) showed abnormalities such as ground-glass opacities or consolidation and 1(1.3%) patient had entirely normal chest CT examinations in the non-survivor group (Figure 1).
Vaccination reduced the SARS-CoV-2 infection ratio to (OR: 0.999, 95% CI: 0.999-1.000, p>0.001) compare with unvaccinated group. Sinopharm and AstraZeneca has reduced SARS-CoV-2 infection ratio to (OR: 0.403, 95% CI: 0.170-0.953, p=0.038; OR: 0.039, CI: 0.020-0.078, p<0.001, respectively) compare with unvaccinated. However, other types of vaccination were not statistically significant (Table 4).
Discussion
Patients characters, symptoms, and comorbidities of COVID-19
In our report, we found elderly and dyspnea may influence the motility of COVID19 patients. However, fever, headache, loss of taste and smell, and sputum production, etc. are common clinical symptoms of COVID19 patients. Our results were also similar to those previously reported and elderly, dyspnea, cough, and chest pain was significantly more frequent in patients infected with SARS-CoV-2 [15-17].
COVID-19 patients have a wide range of diseases, from asymptomatic to extremely severe cases. World Health Organization (WHO) reported that the majority of COVID-19 patients (about 80%) are asymptomatic or mild, 15% are severe, require oxygen, and 5% are critical cases that require mechanical ventilation [18-20]. Therefore, COVID-19 and other common colds can be difficult to distinguish due to their similar initial symptoms [21-23].
Further, several previous studies have shown that the appearance of comorbidities such as elderly, cardiac disease, diabetes, chronic lung disease, and obesity contribute to severe outcomes [12,14,24-28]. The initial stages of COVID-19 patients were managed in China and further management procedures were performed globally [29]. On the other hand, our report is the first to examine the correlations of patient-related factors to the COVID-19 patient rate in Mongolia, and in this respect, this report provides new knowledge. Our study showed that risk factors for cardiovascular disease and hypertension are also important risk factors for severe COVID-19. In particular, hypertension has been reported as a common comorbidity of COVID-19, especially among patients with more serious diseases. In a cohort of 138 inpatients with COVID-19, the reported hypertension rate was 31% [30]. Further, Kong, et al. reported that 22.6% had hypertension [31]. In a large series of COVID-19 patients, of 3335 Italian patients died in the hospital where the clinic charts could be analyzed. Only 136 deaths (4.1%) did not have a pathological report, while 493 (14.8%), 716 (21.5%) and 1990 (59.7%) had one and two, respectively. Reported to have one or at least three chronic diseases. Of these, hypertension is the most frequently reported comorbidity, followed by diabetes and ischemic heart disease [30].
Consistent with these data, an analysis of 44,672 confirmed COVID-19 cases from Wuhan, China, showed increased case fatality in the presence of cardiovascular disease (10.5%) and hypertension (6.0%) [32]. In the Italian retrospective case series, hypertension, regardless of age, is the most common comorbidity of COVID-19 patients referred to the Intensive Care Unit (ICU), with a global prevalence of 49%, followed by cardiovascular disease (21%) and hypercholesterolemia (18%) [33]. The prevalence of hypertension was also higher in critically ill patients who died in the intensive care unit (ICU) compared to individuals discharged from the ICU [33]. Therefore, the findings of our data also support previous data that individuals with cardiovascular disease and hypertension may have a tendency to mortality of COVID-19 patients and that treatment of these diseases may improve prognosis.
In our report, cancers were significantly found in survivors of COVID-19 patients (Table 1). Recent reports have shown that the tumor microenvironment such as Tumor Infiltrating Lymphocytes (TILs) and macrophages is an important factor in tumor growth and development [34-38]. The immunosuppressive status of some cancer patients, whether caused by the disease itself or the treatment, increases their risk of mortality. Immunosuppression may also induce cancer patients from developing serious complications due to infection, causing delays in treatment and unnecessary hospitalizations, which could negatively affect patients. After the initial innate response, a specific adaptive immune response is required to eliminate COVID-19 [39,40]. However, lymphopenia, an independent poor prognostic indicator in COVID-19 patients is common and therefore likely to happen in cancer patients receiving aggressive treatment, the required immune response is weakened [41,42]. In the COVID-19 pandemic, cancer patients are considered a highly hazardous group due to immune systems disorders caused by both tumor growth and anti-cancer treatment [43-47]. A cohort study of 28 COVID-19 cancer patients reported that Stage IV patients showed a higher proportion of infected patients. They assume that patients with later-stage cancer may be more susceptible to SARS-CoV-2 [29,44,48,49]. Therefore, our results are inconsistent with these previous results. This may be due to the Mongolian social system. Compared to the vast territory of Mongolia, there are small numbers of hospitals, which have radiographic diagnostic equipment, which mostly exist in Ulaanbaatar (half of Mongolia’s population lives in this city). Even if symptoms of infectious diseases are observed, patients are not possible to be hospitalized for appropriate diagnosis and treatment due to the symptoms of COVID-19 patients may resemble a usual infection as we mention above. On the other hand, cancer patients can be preferentially admitted and receive sufficient treatment not only for COVID-19 but also for general infectious diseases. These may have caused our results to conflict with other reports.
COVID-19 and radiographic equipment
In our data, we found a significantly high ratio of abnormal findings in both x-rays and CT in non-survival patients (Table 2). Nevertheless, many sources now acknowledge that radiographic findings are more sensitive than RT-PCR in detecting SARS-CoV-2 and the previously reported cases could have a SARS-CoV-2 infection because of a false negative PCR test [50,51]. Ai, et al. reported that compared to RT-PCR, chest CT imaging may be a more reliable, practical, and rapid method to diagnose and assess COVID-19 patients, especially in the epidemic area. With RT-PCR results as a reference in 1,014 patients, the sensitivity, specificity, and accuracy of chest CT in indicating SARS-CoV-2 infection were 97%, 25%, and 68%, respectively [50]. In contrast, the positive rate of RT-PCR assay for throat swab samples was 59%. Further, Kohli, et al. reported that commonality of CT findings regardless of RT--PCR status in a large cohort of 2,581 patients and due to its high sensitivity with quick turnaround time is a very useful support method for RT--PCR [51]. These previous reports and our data suggest that the mortality risk of COVID-19 patients can be reduced by advanced diagnostic equipment.
| Risk factors | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P value | OR | 95% CI | p value | |
| Age | 3.081 | 2.120-4.479 | <0.001 | 1.034 | 1.018-1.051 | <0.001 |
| Gender | 0.828 | 0.583-1.177 | 0.294 | - | - | |
| Symptoms | ||||||
| Dyspnea | 6.695 | 4.550-9.852 | <0.001 | 5.209 | 3.218-8.433 | <0.001 |
| Cough | 1.825 | 1.243-2.681 | 0.002 | 1.399 | 0.814-2.402 | 0.224 |
| Fever | 0.364 | 0.252-0.524 | <0.001 | 0.489 | 0.305-0.784 | <0.001 |
| Headache | 0.346 | 0.240-0.500 | <0.001 | 0.334 | 0.205-0.543 | 0.001 |
| Chest pain | 1.457 | 1.-16-2.089 | 0.041 | 1.073 | 0.665-1.731 | 0.772 |
| Fatigue | 0.841 | 0.572-1.235 | 0.377 | - | - | - |
| Loss of taste and smell | 0.097 | 0.059-0.160 | <0.001 | 0.142 | 0.073-0.275 | <0.001 |
| Sputum production | 0.41 | 0.269-0.624 | <0.001 | 0.509 | 0.283-0.917 | 0.025 |
| Sore throat | 0.408 | 0.260-0.639 | <0.001 | 0.466 | 0.251-0.865 | 0.016 |
| Comorbidity | ||||||
| Diabetes mellitus | 0.928 | 0.623-1.382 | 0.713 | - | - | - |
| Cardiovascular disease | 2.146 | 1.357-3.392 | 0.001 | 1.184 | 0.654-2.144 | 0.576 |
| Hypertension | 6.744 | 4.291-10.598 | <0.001 | 5.065 | 3.065-8.368 | <0.001 |
| Cancer | 0.418 | 0.231-0.755 | 0.004 | 0.772 | 0.274-2.177 | 0.624 |
| OR: Odds Ratio | ||||||
Table 2: Impact of risk factors for survivors and non-survivors.
However, in Mongolia, there are few medical facilities equipped with CT, and MRI, and most of them only evaluate respiratory diseases by x-ray. Our available 715 cases showed that, 667 cases were x-rayed, 127 were CT and there was no MRI (Table 3). Further, as chest x-ray was regarded as an insensitive tool, the American College of Radiologists and the Fisher Society have suggested that imaging is not advised for patients who tested positive by RT-PCR who were asymptomatic or have mild symptoms and a CT scan should be performed for patients with a progressive disease course [52,53]. Rousen, et al. reported that a total of 190 chest x-rays were obtained for the 88 patients with a total of 59 (31%) abnormal chest x-rays and 85% of the COVID-19 patients had negative chest x-rays [54,55]. Therefore, our country’s radiographic diagnosis must be improved in the future, but it may depend on the social and financial situation in Mongolia.
| Survivor (n=161) | non-Survivor (n=554) | p value* | ||
|---|---|---|---|---|
| X-ray | 113 (70.1%) | 554 (100%) | <0.001 | |
| Normal | 13 (8.0%) | 1 (0.18%) | - | |
| Abnormal | Consolidation | 3 (1.8%) | 42 (7.58%) | - |
| GGO | 101 (62.3%) | 508 (91.7%) | - | |
| GGO/consolidation | 0 (0%) | 3 (0.54%) | - | |
| CT | 50 (31.0%) | 77 (13.9%) | <0.001 | |
| Normal | 1 (0.6%) | 1 (0.2%) | - | |
| Abnormal | Consolidation | 11 (6.8%) | 49 (8.8%) | - |
| GGO | 36 (22.4%) | 16 (2.9%) | - | |
| GGO/consolidation | 2 (1.2%) | 11 (2.0%) | - |
Chi square*, CT: Computed Tomography, GGO: Ground Glass Opacity
Table 3: Frequency of imaging in the COVID-19 patients.
| Vaccinations | OR | 95% CI | p value |
|---|---|---|---|
| Unvaccinated | Reference | - | |
| Vaccinated | 0.999 | 0.999-1.000 | 0.002 |
| Types of vaccination | |||
| Unvaccinated | Reference | - | |
| Sinopharm | 0.403 | 0.170-0.0.953 | 0.038 |
| Pfizer | 1.108 | 0.232-5.274 | 0.898 |
| Sputnik V | 0.806 | 0.162-3.998 | 0.792 |
| AstraZeneca | 0.039 | 0.020-0.078 | <0.001 |
| OR: Odds Ratio | |||
Table 4: Impact of vaccinations for COVID-19 patients.
Conclusion
From our data, elderly, dyspnea, cough, chest pain, cardiovascular disease, and hypertension were the major predictors of COVID-19 patient mortality in the multivariate analysis. From these findings, improving prognosis in Mongolian patients may require greater attention and improvement in the management of characters of patients with COVID-19. However, in an environment with limited economic resources like our country, high costs could be restrictive in Mongolia.
Our study has several limitations. First, Mongolia is in a special position to monitor the effects of SARS-CoV-2 vaccines as four approved ones including the BNT-162b2 (BioNTech/Pfizer) mRNA vaccine, the BBIBP-CorV (Sinopharm), inactivated whole virus vaccine, and the vector vaccines Gam-COVID Vac (Gamaleya Research Institute) and ChAdOx1-S (AstraZeneca), have been available. Therefore, there is heterogeneity in performed vaccines. However, most of the vaccines used were BBIBP-CorV (Sinopharm), so we could not find out the difference between the vaccines. Although the vaccination rate has not been performed in a total of 56.9% of citizens in our data (Dec 2021) which is similar to some of the countries. Second, several variables such as the detail of CT and MRI data, optimal use and efficacy of antivirals and antibiotics, adherence to high levels of supportive therapies, or others could not be exhaustively analyzed in this study as data were collected by only electronic medical records. However, a large sample size from our country supports the internal validity of our results.
Further research is necessary to elucidate the mechanism and characteristics of COVID-19 patients. Our data will contribute to a better understanding of COVID-19 patients in a similar developing country and probably help in the guidance of research and treatment strategies.
Authors contributions
T Jamiyan and H Kuroda contributed equally to this work; T Jamiyan, H Kuroda and B Enkhbat collected clinical and pathological information; H Kuroda and T Jamiyan analyzed the data and wrote the manuscript; B Enkhbat, N Mendsaikhan and U Gotov made critical revisions to the manuscript; H Kuroda and T Jamiyan designed the study; T Jamiyan gave the final approval of the manuscript for publication. All authors read and approved the final manuscript.
Conflict of interests
No conflict of interests is declared
References
- Li Q, Guan X, Wu P, Wang X, Zhou L, et al. (2020) Early transmission dynamics in Wuhan, china, of novel coronavirus-infected pneumonia. N Engl J Med 382:1199-1207.
[Crossref] [Google Scholar] [PubMed]
- Li X, Zai J, Wang X, Li Y (2020) Potential of large "first generation" human-to-human transmission of 2019-nCoV. J Med Virol 92: 448-454.
[Crossref] [Google Scholar] [PubMed]
- Chen L, Liu W, Zhang Q, Xu K, Ye G, et al. (2020) RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg Microbes Infect 9:313-319.
[Crossref] [Google Scholar] [PubMed]
- Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, et al. (2020) Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med 382:970-971.
[Crossref] [Google Scholar] [PubMed]
- Song F, Shi N, Shan F, Zhang Z, Shen J, et al. (2020) Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 297:E346.
[Crossref] [Google Scholar] [PubMed]
- Chimeddamba O, Peeters A, Walls HL, Joyce C (2015) Noncommunicable disease prevention and control in Mongolia: A policy analysis. BMC Public Health 15:660.
[Crossref] [Google Scholar] [PubMed]
- Dugee O, Munaa E, Sakhiya A, Mahal A (2017) Mongolia's public spending on non-communicable diseases is similar to the spending of higher-income countries. Health Aff (Millwood) 36: 918-925.
[Crossref] [Google Scholar] [PubMed]
- Ali MM, Malik MR, Ahmed AY, Bashir AM, Mohamed A, et al. (2020) Survival analysis of all critically ill patients with COVID-19 admitted to the main hospital in Mogadishu, Somalia, 30 march-12 June 2020: Which interventions are proving effective in fragile states?. Int J Infect Dis114:202-209.
[Crossref] [Google Scholar] [PubMed]
- Sedighi I, Fahimzad A, Pak N, Khalili M, Shokrollahi MR, et al. (2022) A multicenter retrospective study of clinical features, laboratory characteristics, and outcomes of 166 hospitalized children with coronavirus disease 2019 (COVID-19): A preliminary report from lranian Network for Research in Viral Diseases (INRVD). Pediatr Pulmonol 57:498-507.
[Crossref] [Google Scholar] [PubMed]
- Dini G, Montecucco A, Rahmani A, Barletta C, Pellegrini L, et al. (2022) Clinical and epidemiological characteristics of COVID-19 during the early phase of the SARS-CoV-2 pandemic: a cross-sectional study among medical school physicians and residents employed in a regional reference teaching hospital in Northern Italy. Int J Occup Med EnvironHealth 34:189-201.
[Crossref] [Google Scholar] [PubMed]
- Lechien JR, Chiesa-Estomba CM, De Siati DR, Horoi M, Le Bon SD, et al. (2020) Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 277:2251-261.
[Crossref] [Google Scholar] [PubMed]
- Tamura RE, Said SM, de Freitas LM, Rubio IGS (2021) Outcome and death risk of diabetes patients with COVID-19 receiving pre-hospital and in-hospital metformin therapies. Diabetol Metab Syndr 13:76.
[Crossref] [Google Scholar] [PubMed]
- Moga S, Teodorescu A, Ifteni P, Gavris C, Petric PS (2021) Inflammatory response in SARS-CoV-2 infection of patients with schizophrenia and long-term antipsychotic treatment. Neuropsychiatr Dis Treat 17:3053-3060.
[Crossref] [Google Scholar] [PubMed]
- Zhang T, Huang WS, Guan W, Hong Z, Gao J, et al. (2020) Risk factors and predictors associated with the severity of COVID-19 in China: a systematic review, meta-analysis, and meta-regression. J Thorac Dis 12:7429-7441.
[Crossref] [Google Scholar] [PubMed]
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, et al. (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708-20.
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, et al. (2020) Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J 55:2000547.
[Crossref] [Google Scholar] [PubMed]
- Fu L, Wang B, Yuan T, Chen X, Ao Y, et al. (2020) Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: A systematic review and meta-analysis. J infect 80: 656-665.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization (WHO) Coronavirus disease (COVID-19) dashboard, www.who.int, 2020.
- Buitrago-Garcia D, Egli-Gany D, Counotte MJ, Hossmann S, Imeri H, et al. (2020) Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med 17:e1003346.
[Crossref] [Google Scholar] [PubMed]
- Oran DP, Topol EJ (2020) Prevalence of asymptomatic SARS-CoV-2 infection: A narrative review. Ann Intern Med 173:362-367.
[Crossref] [Google Scholar] [PubMed]
- Centers for disease control and prevention similarities and differences between flu and COVID-19, www.cdc.gov, 2020.
- Mazzuca C, Falcinelli I, Michalland AH, Tummolini L, Borghi AM (2021) Differences and similarities in the conceptualization of COVID-19 and other diseases in the first Italian lockdown. Sci Rep 11:18303.
[Crossref] [Google Scholar] [PubMed]
- Osman M, Klopfenstein T, Belfeki N, Gendrin V, Zayet S (2021) A comparative systematic review of COVID-19 and influenza. Viruses 13:452.
[Crossref] [Google Scholar] [PubMed]
- Zhao Q, Meng M, Kumar R, Wu Y, Huang J, et al. (2020) The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J MedVirol 92:1915-1921.
[Crossref] [Google Scholar] [PubMed]
- Lim S, Bae JH, Kwon HS, Nauck MA (2021) COVID-19 and diabetes mellitus: from pathophysiology to clinical management. Nat Rev Endocrinol 17:11-30.
[Crossref] [Google Scholar] [PubMed]
- Motaib I, Zbiri S, Elamari S, Haoudar A, Chadli A, el al. (2021) Cardiovascular risk factors and the severity of COVID-19 disease. Cureus 13:e15486.
[Crossref] [Google Scholar] [PubMed]
- Kautzky-Willer A (2021) Does diabetes mellitus mitigate the gender gap in COVID-19 mortality?. Eur J Endocrinol 185:C13-C17.
[Crossref] [Google Scholar] [PubMed]
- Miyazawa D (2021) Why obesity, hypertension, diabetes, and ethnicities are common risk factors for COVID‐19 and H1N1 influenza infections. J Med Virol 93:127-128.
[Crossref] [Google Scholar] [PubMed]
- Zhang L, Zhu F, Xie L, Wang C, Wang J, et al. (2020) Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol 31:894-901.
[Crossref] [Google Scholar] [PubMed]
- Wang D, Hu B, Hu C, Zhu F, Liu X, et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 323:1061-1069.
[Crossref] [Google Scholar] [PubMed]
- Kong KA, Jung S, Yu M, Park J, Kang IS (2021) Association between cardiovascular risk factors and the severity of coronavirus disease 2019: Nationwide epidemiological study in Korea.Front Cardiovasc Med 8:732518.
[Crossref] [Google Scholar] [PubMed]
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA 323:1239-1242.
[Crossref] [Google Scholar] [PubMed]
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, et al. (2020) Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 323:1574-1581.
[Crossref] [Google Scholar] [PubMed]
- Jamiyan T, Kuroda H, Yamaguchi R, Abe A, Hayashi M, et al. (2020) CD68- and CD163-positive tumor-associated macrophages in triple-negative cancer of the breast. Virchows Arch 477:767-775.
[Crossref] [Google Scholar] [PubMed]
- Kuroda H, Jamiyan T, Yamaguchi R, Kakumoto A, Abe A, et al. (2021) Tumor-infiltrating B cells and T cells correlate with postoperative prognosis in triple-negative carcinoma of the breast. BMC Cancer 21:286.
[Crossref] [Google Scholar] [PubMed]
- Jamiyan T, Kuroda H, Yamaguchi R, Nakazato Y, Noda S, et al. (2020) Prognostic impact of a tumor-infiltrating lymphocyte subtype in triple-negative cancer of the breast. Breast Cancer 27: 880-892.
[Crossref] [Google Scholar] [PubMed]
- Kuroda H, Jamiyan T, Yamaguchi R, Kakumoto A, Abe A, et al. (2021) Tumor microenvironment in triple-negative breast cancer: the correlation of tumor-associated macrophages and tumor-infiltrating lymphocytes. Clin Transl Oncol 23:2513-2525.
[Crossref] [Google Scholar] [PubMed]
- Kuroda H, Jamiyan T, Yamaguchi R, Kakumoto A, Abe A, et al. (2021) Prognostic value of tumor-infiltrating B lymphocytes and plasma cells in triple-negative breast cancer. Breast Cancer 28:904-914.
[Crossref] [Google Scholar] [PubMed]
- Wagner KI, Mateyka LM, Jarosch S, Grass V, Weber S, et al. (2022) Recruitment of highly cytotoxic CD8(+) T cell receptors in mild SARS-CoV-2 infection. Cell Rep 38:110214.
[Crossref] [Google Scholar] [PubMed]
- Paces J, Strizova Z, Smrz D, Cerny J (2020) COVID-19 and the immune system. Physiol Res 69:379-88.
[Crossref] [Google Scholar] [PubMed]
- Yang L, Chai P, Yu J, Fan X (2020) Effects of cancer on patients with COVID-19: a systematic review and meta-analysis of 63,019 participants. Cancer Biol Med 18:298-307.
[Crossref] [Google Scholar] [PubMed]
- Lee J, Park SS, Kim TY, Lee DG, Kim DW (2021) Lymphopenia as a biological predictor of outcomes in COVID-19 patients: A nationwide cohort study. Cancers (Basel) 13:471.
[Crossref] [Google Scholar] [PubMed]
- Liang W, Guan W, Chen R, Wang W, Li J, et al. (2021) Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol 21:335-337.
[Crossref] [Google Scholar] [PubMed]
- Liu C, Zhao Y, Okwan-Duodu D, et al. (2020) COVID-19 in cancer patients: Risk, clinical features, and management. Cancer Biol Med 17:519-527.
[Crossref] [Google Scholar] [PubMed]
- Dai M, Liu D, Liu M, Zhou F, Li G, et al. (2020) Patients with cancer appears more vulnerable to SARS-CoV-2: A multicenter study during the COVID-19 outbreak. Cancer Discov 10:783-791.
[Crossref] [Google Scholar] [PubMed]
- Shi Y, Wang Y, Shao C, Huang J, Gan J, et al. (2020) COVID-19 infection: the perspectives on immune responses. Cell Death Differ 27:1451-1454.
[Crossref] [Google Scholar] [PubMed]
- Jyotsana N, King MR (2020) The impact of COVID-19 on cancer risk and treatment. Cell Mol Bioeng 13:1-7.
[Crossref] [Google Scholar] [PubMed]
- iu Y, Liu L, Wang Y, Du X, Ma H, et al. (2020) Clinical course and characteristics of patients with coronavirus disease 2019 in Wuhan, China: a single-centered, retrospective, observational study. Aging 2:15946-15953.
[Crossref] [Google Scholar] [PubMed]
- Sinha S, Kundu CN (2021) Cancer, and COVID-19: Why are cancer patients more susceptible to COVID-19?. Med Oncol 38:101.
[Crossref] [Google Scholar] [PubMed]
- Ai T, Yang Z, Hou H, Zhan C, Chen C, el al. (2020) Correlation of chest CT and RT-PCR testing for coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology 296:E32-E40.
[Crossref] [Google Scholar] [PubMed]
- Kohli A, Joshi A, Shah A, Jain RD, Gorlawar A, et al. (2021) Does CT help in reducing RT-PCR false negative rate for COVID-19?. Indian J Radiol Imaging 31:S80-S86.
[Crossref] [Google Scholar] [PubMed]
- American College of Radiology (ACR) recommendations for the use of chest radiography and computed tomography (CT) for suspected COVID-19 infection, www.acr.org, 2020.
- Rubin GD, Ryerson CJ, Haramati LB, Sverzellati N, Kanne JP, et al. (2020) The role of chest imaging in patient management during the COVID-19 pandemic: A multinational consensus statement from the Fleischner society. Chest 158:106-116.
[Crossref] [Google Scholar] [PubMed]
- Rousan LA, Elobeid E, Karrar M, Khader Y (2020) Chest x-ray findings and temporal lung changes in patients with COVID-19 pneumonia. BMC Pulm Med 20:245.
[Crossref] [Google Scholar] [PubMed]
- Abu-Halaweh S, Alqassieh R, Suleiman A, Al-Sabbagh MQ, AbuHalaweh M, et al. (2021) Qualitative assessment of early adverse effects of Pfizer–BioNTech and sinopharm COVID-19 vaccines by telephone interviews. Vaccines (Basel) 9:950.
[Crossref] [Google Scholar] [PubMed]
Citation: Jamiyan T, Kuroda H, Mendsaikhan N, Gotov U, Enkhbat B (2023) Risk Factors for Mortality among COVID-19 Patients: Nationwide Cohort Study of Mongolia. Diagnos Pathol Open 8:210. DOI: 10.4172/2476-2024.8.1.210
Copyright: © 2023 Jamiyan T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2379
- [From(publication date): 0-2023 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 2061
- PDF downloads: 318