Risk Factors Associated With the Frequency of Seizure Attack on People Living With Epilepsy at Felege Hiwot Referral Hospital; Application of A Linear Mixed Model
Received: 01-Nov-2022 / Manuscript No. jart-22-82843 / Editor assigned: 03-Nov-2022 / PreQC No. jart-22-82843 (PQ) / Reviewed: 17-Nov-2022 / QC No. jart-22-82843 / Revised: 19-Nov-2022 / Manuscript No. jart-22-82843 (R) / Accepted Date: 21-Nov-2022 / Published Date: 26-Nov-2022
Abstract
Background: The frequency of seizure attacks, in people living with epilepsy, is one of the most common and serious brain disorders. It affects more than 70 million people in the world, including approximately 10 million people annually in Sub-Saharan Africa. In Ethiopia, it affects about 29.5 per 1000 population. It has major physical, psychological, and economic effects by reducing an individual’s quality of life. The main objective of this study was to identify risk factors associated with the frequency of seizure attacks in people living with epilepsy in North-West Ethiopia.
Methods: A retrospective cohort study design was conducted on 131 people living with epilepsy who satisfied the inclusion criterion in the neurologic clinic at Felege Hiwot specialized and Referral Hospital, Bahir Dar, Ethiopia. A secondary data source was used for the current investigation. The data were collected using the patient’s chart whose follow-ups were between November 2014 and 31 December 2019. Based on the lowest AIC and BIC values, the appropriate linear mixed-effect model was selected for data analysis.
Results: Among the predictors, follow-up times (β= -0.088; 95% CI; (-9.395685e-02, -8.161152e-02), p-value<0.01), duration of time between seizure onset and diagnosis (β= 0.003; 95% CI; (0.002, 006), p-value=0.0042), and people living with epilepsy whose belief was can be cured from the disease at the start of taking antiepileptic medication reduced the frequency of seizure attack (β= -0.054; 95% CI; (-1.033209e-01, -4.189269e-2, p-value= 0.0338). Age at seizure onset (β= -0.003; 95% CI; (-5.095402e-03, -4.979875e-04), p-value=0.0175=) people with intellectual disability (β= 0.081; 95% CI; (2.479245e-02, 1.366274e-01), p-value= 0.0050), and people having a history of febrile convulsion (β= 0.071; 95% CI; (8.792496e-03, 1.324884e-01), p-value= 0.0255) statistically affected the frequency of seizure attack on people living with epilepsy. Poor adherent individuals and those having a family disease history were also highly affected by the repeated occurrence of seizure attacks.
Conclusion: One way to reduce the frequency of seizure attacks is free to access to anti-seizure medications. Attention should be given to patients with a history of head injury, patients who came later after seizure onset, those people having a high frequency of seizure attacks at the beginning of diagnosis, those with intellectual disabilities, and those who have a family seizure history.
Keywords
Addiction research; Addiction therapy; Frequency of seizure attacks; Linear Mixed Model; Seizure freedom; people living with epilepsy.
List of Abbreviations
ASMs=Anti-seizure Medication; AIC = Akaki information criteria; BIC= Bayesian information criteria; LRT=likelihood ratio test; CI= confidence interval
Introduction
Epilepsy is one of the most chronic non-communicable diseases of the brain which is the condition of at least two unprovoked seizures occurring more than 24 hours apart; one unprovoked seizure and diagnosis of an epilepsy syndrome [1, 2]. Epilepsy is a disorder of the brain characterized by the repeated occurrence of seizures.
Epilepsy is usually diagnosed after a person has had at least two seizures that were not caused by some known medical conditions, such as alcohol withdrawal or extremely low blood sugar [2]. It is known that the characterizations of recurrent seizures need long-term treatment periods [3].
Globally, about 70 million people living with epilepsy are affected with a high frequency of seizure attacks, with 50.4 per 100,000 people newly diagnosed per year with a prevalence of 5 to 8 cases per 1000 depending on the age group of people living with epilepsy.
Around 85% of the people living with epilepsy, affected by highfrequency of seizure attacks, are from developing countries, and about 100 million people experienced at least one seizure attack in their lives [4-6]. Seizure attacks, for people living with epilepsy, in Sub-Saharan African countries like Ethiopia also affect approximately 10 million people annually and it has a high prevalence in the study area [7].
People living with epilepsy frequently suffer from repeated occurrences of seizures and because of this; they have poor health outcomes and serious physical, psychological, social, and economic effects. Although seizure attack is a treatable condition with cheap medication, the treatment gap varies from 10% in developed countries to 75 % in low-income countries [8].
Approximately 80–90% of people living with epilepsy have frequently attacked by the occurrence of seizures and this further leads to exacerbation of social isolation, unemployment, dependent behavior, psychological issues, and reduced quality of life [9]. Maintaining a seizure-free state for people living with epilepsy with a cost-effective approach is a crucial activity that an individual should follow it [10, 11].
In Ethiopia, the frequency of seizure attacks for people living with epilepsy is a major public health problem, which affects about 29.5 per 1000 population [12]. A study conducted in northern Gondar in Ethiopia indicates that people living with epilepsy face different social, psychological, and physical problems as a result of their frequent seizure attacks which may include stigma and discrimination [13]. Other studies in Ethiopia with regard to the cause and forms of treatment show that there is a widespread belief that the cause of epilepsy is demon possessions or ancestors’ spirits and this hinders the patients not to use modern anti-seizure medications (ASMs) [14]. Traditional treatments are commonly used in Ethiopia and only 1.6% had been treated with modern antiepileptic medication in rural communities and 13% in the urban community of the country [15].
One of the previous studies indicates that about 58% of the people living with epilepsy developed generalized tonic-clonic seizures frequently. Among these, 23.2% of them increased the accident of intellectual disabilities, death, and developed drug resistance [16]. Most of the studies conducted previously in the study area focused on the severity of the case and didn’t investigate risk factors associated with the frequency of occurrence of seizures [17]. Knowing the risk factors associated with the frequency of seizure attacks among people living with epilepsy helps health practitioners and families of patients to reduce its recurrence [17]. Different studies conducted on people living with epilepsy are cross-sectional and these methods cannot handle the complications that happened because of repetitions of seizure attacks while there are known difficulties to use these methods, verifying their assumptions, and interpreting the results correctly [17, 18]. Such approaches ignore different sources of correlation due to repeated seizure attacks (frequency of seizure attack). Ignoring the source of correlation has several consequences which cause higher false positive rates, invalid confidence intervals, and underestimating the standard errors [18]. Therefore, the current study aimed to investigate risk factors associated with the frequency of seizure attacks in people living with epilepsy under treatment in Felege-Hiwot Hospital, Bahir Dar, Ethiopia.
Materials and Methods
Study area and Study design: A retrospective cohort study design was conducted for the current investigation on people with epilepsy. The study was conducted with relevant information, recorded by health staff during treatment, from the medical charts of people living with epilepsy. The study was conducted at Felege-Hiwot specialized hospital, in northwest Ethiopia. This hospital serves as a specialized, teaching and referral hospital for people who came from different district hospitals in the surrounding areas of north-western Ethiopia. It is the only governmental hospital in the study area that delivers treatment for people living with epilepsy. The hospital also provides a training service for health practitioners/students for apprenticeships from various health institutions, including Bahir Dar University, Ethiopia.
Source of population and data collection procedures: People living with epilepsy who started anti-seizure medication (ASMs) at Felege-Hiwot Hospital were used as a source of the population for this study. The study exclusively used secondary sources. For the current study, the data were collected by trained health staff within the hospital from the medical chart of people with epilepsy at the hospital whose follow-ups were from November 2014 up to 31 December 2019. Therefore, a data extraction checklist was designed by the authors in consultation with health staff within the hospital.
Sample size and sampling procedures: In the study area, among the total of 1652 newly registered people living with epilepsy reported by the neurologic clinic at the hospital in the study period, only 131 of them had at least two seizure attacks during the study period and satisfied the inclusion criteria to be included in this study. The consort flow diagram for selecting samples who satisfied the inclusion criterion is shown in Figure1. Hence, the purposive sampling technique was used for the current study. Since the study design was retrospective/ longitudinal, people living with epilepsy with at least two seizure attacks were included in this study.
Inclusion criterion: People living with epilepsy, who had at least two seizure attacks and started their anti-seizure medications within the hospital were included in the current study. On the other hand, People living with epilepsy under treatment who had no frequent seizure attacks (less than two seizure attacks) approved by the health staff were excluded from this study (Figure 1).
Variables under study: The response variable for this study was the frequency of seizure attacks on people living with epilepsy. This variable was recorded every six months for people living with epilepsy. Hence, the data were collected at equal intervals of period. The potential predictor variables consist of socio-demographic and clinical variables. The potential predictor variables for the current investigation are indicated in Figure2. The categories of variables are indicated in Table1 (results section) (Figure 2).
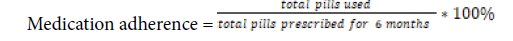
Medication adherence was categorized as good adherence if a patient used 95% of the pills taken from the hospital, Fair adherence if a patient used 85-95% of the pills taken from the hospital otherwise poor adherence. Adherence was computed as follows;
Statistical Data Analysis
The changes or variations were conducted at individual or group patterns over time. The advantage of longitudinal data over crosssectional studies is that it helps to see both group and individual effects over time and has more statistical power [19, 20]. Exploratory data analysis was conducted to detect individual trends throughout the study period. Univariable and multivariable data analyses were also conducted to assess the significant predictors in the current investigation. All predictor variables were considered in univariable data analysis to identify the statistically significant variables at 25% significance variables and those statistically significant ones at 25% were also considered in multivariable data analysis.
The covariance structure for the current investigation was also assessed. To identify the appropriate covariance structure, the commonly used covariance structures namely independence (IND), compound symmetry (CS), first-order autoregressive AR (1), Toeplitz (Toep), and unstructured (UN) were considered. Among the potential covariate structures indicated above, the first-order autoregressive (AR (1)) covariance structure was selected due to its smallest AIC and BIC compared to the others. Similar to covariance structures, an appropriate random effect model was also selected by using the likelihood ratio test and this indicates that the model with random intercept and the random slope was a better fit for the given data. This model allows the intercept and coefficient to vary randomly among individuals.
Data analysis was conducted using R software. The study was conducted for 60 months in such a way that the data was recorded every six months. Exploratory data analysis was also conducted in order to assess various associations and patterns exhibited in the data. Additionally, the individual profile plots, mean structure plots, and variance plots were obtained in order to assess the pattern at individual and group levels [21]. The plotting of the occurrence of a seizure over time and graphs of different subgroups/categories were included in the investigation to illustrate the relationship between the expected occurrences of a seizure in people living with epilepsy.
Results
Descriptive results on socio-demographic variables
The categorical socio-demographic variables under study are indicated in Table1. Table1 shows that about 61.8% of the patients were male, 70.2% of them had a family disease history, 74% of patients developed an intellectual disability, 20.6% of them had a history of febrile convulsion, and about 69.5% believed to cure when they took ASMs (anti-seizure medication). Among the study subjects, 34.4% of them took traditional drugs to cure the disease, 20.6% of the patients got head injuries, and 57.3% of patients got free medication source. Among the patients, about 74% of them took monotherapy anti-seizure medication at the beginning of follow-ups, 39.7% were high adherent patients whereas 30.5% were low adherent patients.
The covariates under the current investigation are also summarized in Table2. Table 2 indicates that the average baseline age of participants included in this study was 30.5 with a standard deviation of 12.5 years. The average duration of time between seizure onset and diagnosis was 12.93 weeks. The average of ASMs at the initial time was 100.04 mg of drugs (Tables 1 and 2).
| Variables | Category | Frequency(n) | Percentage (%) |
|---|---|---|---|
| Sex | Female | 50 | 38.2 |
| Male | 81 | 61.8 | |
| Residence | Urban | 65 | 49.6 |
| Rural | 66 | 50.4 | |
| Religion | Protestant | 4 | 3.1 |
| Orthodox | 105 | 80.2 | |
| Muslim | 22 | 16.8 | |
| Marital status | Single | 62 | 47.3 |
| Married | 42 | 32.1 | |
| Divorced | 21 | 16.0 | |
| Widowed | 6 | 4.6 | |
| Education level | Illiterate | 62 | 47.3 |
| religious school | 7 | 5.3 | |
| Primary | 28 | 21.4 | |
| Secondary | 20 | 15.3 | |
| Tertiary | 14 | 10.7 | |
| Occupation | Gov't employee | 19 | 14.5 |
| Student | 11 | 8.4 | |
| Farmer | 45 | 34.4 | |
| Skilled labour | 20 | 15.3 | |
| Others | 36 | 27.5 | |
| Family History | No | 92 | 70.2 |
| Yes | 39 | 29.8 | |
| Intellectual disability | No | 97 | 74.0 |
| Yes | 34 | 26.0 | |
| History of Febrile seizure | No | 104 | 79.4 |
| Yes | 27 | 20.6 | |
| Co-morbidity | No | 97 | 74.0 |
| Yes | 34 | 26.0 | |
| Belief of cure from the disease | No | 40 | 30.5 |
| Yes | 91 | 69.5 | |
| Traumatic brain | No | 104 | 79.4 |
| Yes | 27 | 20.6 | |
| Medication Sources | Free | 56 | 42.7 |
| Payment | 75 | 57.3 | |
| Adherence Level | poor | 40 | 30.5 |
| Fair | 39 | 29.8 | |
| Good | 52 | 39.7 |
Table 1: Descriptive result of epileptic patients.
| Variables | Minimum | Maximum | Mean | Std. Deviation | Variance | |
|---|---|---|---|---|---|---|
| Baseline age at registration(years) | 18.00 | 66.00 | 30.5038 | 12.50300 | 156.325 | |
| Duration of time b/n seizure onset and diagnosis | 0.166 | 58 | 12.93 | 13.97 | 195.16 | |
| Dose of ASMs at initial(mg) | 30.00 | 600.00 | 150.0000 | 107.04780 | 11459.231 | |
Table 2: Description of continuous variables.
The current investigation indicates that as follow-up time increased by one unit, the expected frequency of seizure attacks decreased. For instance, the expected frequency of seizure attacks at the baseline was 7.51 with a standard deviation of 8.91, and at the tenth visit (the last visit); it was reduced to 0.4 with a standard deviation of 0.41.
The repeated measurement for each individual over time indicates that there was a visible pattern for all people with epileptic seizures. The individual profile plot also shows that there was larger variability at the beginning/commencement of ASMs and this variability decreased over time or becomes minimal at the end. Hence, their variation of occurrence of a seizure was larger at the initial time and comes closer and closure to each other at the end. The result of this investigation revealed that the expected frequency of seizure attacks for some patients was going down, while it was going up for others over time points. This implies that not all the patients responded the same to ASMs treatment and this magnifies the relevance of the random component of a mixed effects model to address the random effects part in addition to fixed effects
Inference for statistical significant variables
Univariable data analysis was performed in order to see the effect of each covariate on the study variable as shown in Table 3 (Tables 3 and 4).
Fixed Effect |
Coefficients( |
Standard Error |
p-value |
|---|---|---|---|
(Intercept) |
0.9531 |
0.049 |
<0.0010 |
Follow up times |
-0.088 |
0.003 |
0.2010 |
Age of participants |
-0.743 |
0.873 |
0.0435 |
Intellectual Disability |
0.081 |
0.028 |
0.0350 |
Belief of individuals to be Cured from seizure |
-0.054 |
0.025 |
0.2380 |
Presence of co-morbidity |
0.076 |
0.026 |
0.1341 |
| Traumatic brain |
0.543 |
0.691 |
0.842 |
History of febrile convulsion |
0.071 |
0.031 |
0.2050 |
Age at seizure onset |
-0.003 |
0.00116 |
0.1750 |
Dose of ASMs used at initial time |
0.0005 |
1.04*10-4 |
0.0810 |
Family disease history |
0.05396 |
0.026 |
0.0419 |
Drug Addiction history before diagnosis |
0.0499 |
0.0322 |
0.1244 |
Sex |
0.0093 |
0.025 |
0.7064 |
Duration of time b/n seizure onset and diagnosis |
0.0033 | 0.0012 |
0.2042 |
| Medication drug source | 0.06195 | 0.03009 | 0.2395 |
| Medication Adherence level |
-0.10976 |
0.0349809 | 0.0017 |
Table 3: Univariable data analysis.
Fixed Effects |
Coefficients( |
S.E |
95%CI |
p-value |
|
|---|---|---|---|---|---|
Lower |
Upper | ||||
(Intercept) |
0.9531 |
0.049 |
0.8557696, |
1.050234 |
<0.001* |
Follow up times |
-0.088 |
0.003 |
-9.395685e-02 |
-8.161152e-02 |
<0.001* |
Intellectual Disability(Ref.=No) |
|||||
Yes |
0.081 |
0.028 |
2.479245e-02 |
1.366274e-01 |
0.0050* |
Cure belief(Ref.=NO) |
|
|
|
|
|
Yes |
-0.054 |
0.025 |
-1.033209e-01 |
-4.189269e-03 |
0.0338* |
Presence of Co-morbidity(Ref.=No) |
|||||
Yes |
0.076 |
0.026 |
2.453096e-02 |
1.273038e-01 |
0.0041* |
History of febrile convulsion(Ref.=No) |
|||||
Yes |
0.071 |
0.031 |
8.792496e-03 |
1.324884e-01 |
0.0255* |
Age at seizure onset |
-0.003 |
0.00116 |
-5.095402e-03 |
-4.979875e-04 |
0.0175* |
Dose of ASMs in mm |
0.0005 |
1.04*10-4 |
2.835888e-04 |
6.948991e-04 |
<0.001* |
Family disease history(Ref.=No) |
|||||
Yes |
0.05396 |
0.026 |
1.059110e-01 |
2.012778e-03 |
0.0419* |
Drug Addiction history before diagnosis(Ref.=No) |
|||||
Yes |
0.0499 |
0.0322 |
-1.391967e-02 |
1.135582e-01 |
0.1244 |
Duration of time b/n seizure onset and diagnosis |
0.0033 | 0.0012 | 0.0015 |
0.0058 |
0.0042* |
| Medication drug source(Ref.=Free) | |||||
| Payment | 0.06195 | 0.03009 | 0.0028 | 0.12111 | 0.0395* |
| Medication Adherence level(Ref.=Poor) | |||||
| Fair adherence Good adherence |
-0.10976 |
0.0349809 |
-0.2074832 |
-0.08861044 |
0.0017* |
-0.196804 |
0.0447064 |
-0.2852631 |
-0.108344704 |
<0.001* |
|
| Random Effects | |||||
|
|
Estimated value |
Lower |
Upper | ||
Sd intercept(b0i) |
0.325433347 |
|
0.280848221 |
0.37709644 |
|
Sd (Time(b1i ) |
0.008330061 |
|
0.006725442 |
0.01031753 |
|
Cor (b0i ,b1i,) |
-0.962755 |
-0.978813 |
-0.753933 | ||
| Residual | 0.2122029 | 0.200931 | 0.2241076 | ||
| *stands for statistical significant variable, ASMs stands for ant-seizure medication at initial time | |||||
Table 4: Multivariable data analysis using linear mixed model results.
All predictors except the sex of participants and traumatic brain were significant at a 25% level of significance in Table 3. Hence, all predictors except sex should be considered for data analysis to identify statistically significant ones for the frequency of seizure attacks in multivariable data analysis as shown in Table 4.
Among the potential predictor variables, those that were significant in univariate data analysis and included in the multivariable analysis are indicated in Table 4. The multivariate data analysis was conducted using the selected random intercept and random slope model with an unstructured covariance structure.
Table 4 revealed that for a unit increase in follow-up times, the expected frequency of seizure attacks was decreased by 0.088 keeping all other variables constant(β=-0.088, 95% CI:( -9.395685e-02, -8.161152e-02) and p-value <0.01).
Comparing the study variables between intellectual disabilities and non-disabilities, the expected frequency of seizure attacks for intellectual disabilities was increased by 0.081 as compared to nondisabled ones, keeping other variables constant (β=0.081, 95% CI: (2.479245e-02, 1.366274e-01) and p-value =0.005).
The belief of people living with epilepsy plays a significant role in the reduction of the frequency of seizure attacks. Hence, the expected frequency of seizure attacks for individuals who believed that the disease can be cured with treatment was decreased by 0.054 as compared to patients who believed that it can’t be cured, keeping all other variables constant (β= -0.054, 95% CI:(-1.033209e-0, -4.189269e- 03 ) and p-value= 0.0338).
The expected frequency of seizure attacks for people living with epilepsy, who had other diseases (co-morbidity), was increased by 0.076 as compared to patients without co-morbidity, keeping the other things constant (β= 0.076, 95% CI:( 2.453096e-02, 1.273038e-01) and p-value =0.0041).
The expected frequency of seizure attacks for people living with epilepsy, and having febrile convulsion history, was increased by 0.076 as compared to patients without febrile convulsion history, keeping all other conditions constant (β= 0.071, 95% CI: (8.792496e-03, 1.324884e- 01 ) and p-value =0.0255).
The age of participants at seizure onset also significantly affected the frequency of seizure attacks. Hence, as the age of people living with epilepsy at seizure onset increased by one year, the expected frequency of seizure attacks was decreased by 0.003, keeping all other conditions constant(β = -0.003, 95% CI: (-5.095402e-03, -4.979875e-04 ) and p-value = 0.0175).
The dose of anti-seizure medication at the initial time plays a significant role in the reduction of the frequency of seizure attacks. Hence, as the dose of anti-seizure medication increased by a hundred mm of drug, the expected frequency of seizure attack was also increased by 0.0005 given all other covariates constant (β= 0.0005, 95% CI: (2.835888e-04, 6.948991e-04) and p-value < 0.01).
Similarly, the expected frequency of seizure attacks for people living with epilepsy who had a family disease history was increased by 0.054 as compared to individuals without a family disease history, keeping another thing constant (β= 0.06195, 95% CI: (0.0028, 0.12111) and p-value = 0.0395).
As the duration of time between seizure onset and diagnosis increased by one week, the expected seizure attacks were increased by 0.0033, keeping all other covariates constant (β=0.0033, 95% CI: (0.0015, 0.0058) and p-value =0.0042).
The source of medication also significantly affected the frequency of seizure attacks. The expected frequency of seizure attacks for those people living with epilepsy who got anti-seizure medication with payments was increased by 0.062 as compared to those individuals who got the treatment medication freely, keeping all the other things constant (β= 0.05396, 95% CI: (1.059110e-01, 2.012778e-03) and p-value = 0.0419).
Adherence level had a significant effect on the expected frequency of seizure attacks. Hence, the expected frequency of seizure attacks for good adherent people living with epilepsy was decreased by 0.1968 as compared to low adherent patients, keeping the other variables constant (β = -0.196804, 95% CI: (-0.2852631, -0.108344704), p-value<0.01)
In the random part of the model, the correlation between random intercept and random slope (-0.962755) shows that the people living with epilepsy who had frequent seizures initially had small slopes, which suggests that people living with epilepsy who had a high frequency of seizure attack at the initial time reduced at a greater rate as follow up times increased.
Discussion
The current investigation identified important predictor variables for the variation in the frequency of epileptic seizures. The longitudinal study, conducted in the current investigation, revealed that follow-up times have a significant contribution to the decrease in the frequency of seizure attacks. Hence, the frequency of seizure attacks decreases as visiting time/follow-ups increase and this is agreed with the results obtained in one of the previous studies [22].
Intellectual disability statistically and significantly affects the frequency of seizure attacks. Hence, intellectually disabled people living with epilepsy have a high frequency of seizure attacks as compared to those without disabilities. This result is supported by one of the previous studies [22].
The belief of people living with epilepsy plays a significant role in the reduction of the frequency of seizure attacks. Hence, the expected frequency of seizure attacks for individuals who believed that the disease can be cured with treatment was decreased as compared to patients who believed that it can’t be cured. This result agreed with results obtained from one of the previous studies [23]. However, the current result contradicted the results obtained in one of the other studies, which states that no difference between the two groups [24]. The potential reason for this difference may be a difference in study subjects taken in different areas or different cultures, methods of study, length of the study, and sample size. This needs further investigation.
The expected frequency of seizure attacks for people living with epilepsy, who had other diseases (co-morbidity), had a high frequency as compared to patients without co-morbidity. Hence, people living with epilepsy who had a co-morbidity experience have a high frequency of seizure attacks as compared to non-co-morbidity experience, this result is in line with the studies conducted previously [7].
Patients who have a history of febrile convulsions have a high frequency of epileptic seizures. This result is supported by another study [25] but it is contradicted by another previously conducted study [26]
Age has an effect on the expected frequency of seizure attacks, which indicates that as the age of people at seizure onset increases, the frequency of epileptic seizures decreases which is supported by another study [27].
The dose of ASMs taken at the commencement of their treatment had a significant effect on the variable of interest. Patients with a high dose of initial medication treatment have a higher frequency of epileptic seizures as compared to low medication treatment. Hence, patients should start treatments with a lower dose of ASMs. This result is similar to one of the previous studies [28].
People living with epilepsy who have a family disease history are significantly affected by the frequency of seizure attacks; hence, patients with a family disease history have a high frequency of seizure attacks as compared to those without a family disease history. This result is similar to one of the results obtained in the previous studies [29].
People with a long duration of time between seizure onset and diagnosis and those people living with epilepsy having an intellectual disability are associated with a high frequency of seizure attacks. Hence, people living with epilepsy who come late for diagnosis after the onset of a seizure have a high frequency of seizure attacks. The result obtained in the current study is supported by another study [30]. Intellectually disabled people living with epilepsy have high-frequency seizure attacks as compared to those without intellectually disabled ones. This result is supported by another study conducted previously [31].
People living with epilepsy who got free access to medication treatment have better improvement with regard to the frequency of seizure attacks. This agreed with one of the previous studies [17].
Medication adherence prescribed by the health staff has a significant effect on the frequency of seizure attacks. People whose medication adherence is taken according to the prescription given by the health staff, have a low frequency of epileptic seizures as compared to those individuals who take medication drugs/pills out of the prescription given by the health staff. This result is similar to one of the previous studies [32]. Hence, individuals whose adherence was taken out of the prescription given by the health staff are categorized as non-adherent people and have a high frequency of seizure attacks [32,33].
Conclusion
The expected frequency of seizure attacks in people living with epilepsy was high at the commencement of ASMs and decreased over time because of the treatment and adherence to ASMs. Hence, the disease is treatable and manageable for highly adherent people living with epilepsy considering the proper medications described by the health staff.
The adherence level in the current investigation revealed that there was a higher frequency of seizure attacks for people living with epilepsy at the commencement of their treatment and a rapid reduction of the frequency for people with high adherence levels as compared to pooradherent people with epilepsy.
The increase in follow-up times, the increase of age at seizure onset, high adherence, and the fact that people with epilepsy believed to be cured at the start of taking anti-seizure medication significantly reduced the expected seizures. On the other hand, long duration of time between seizure onset and diagnosis, people with intellectual disabilities, individuals who had a history of febrile convulsion who didn’t have free access to medication, and who had a family disease history associated with a high frequency of seizure attack. Patients with a high dose of an initial drug have a higher frequency of seizures as compared to low-drug users.
The way forward: Patients who experience seizure episodes should visit health facilities immediately and start treatments with a lower amount of anti-elliptic medication. Epileptic patients treated with payments shall be supported by health institutions/governments to decrease the progression rate of seizure attacks. Additionally, health professionals should underline the newly diagnosed people living with epilepsy who are coming to late after seizure onset. People living with epilepsy who have a family history of seizures and febrile seizures should be diagnosed regularly to decrease the progression of seizure attacks.
The results obtained in the current investigation help policymakers and health staff to the amendment of policy issues and proper intervention in reducing the severity of seizures in epileptic patients.
Limitation
This study was not without limitations. The data were taken at one treatment site and including more sites may have additional information. The authors recommend further investigation for future studies by including additional treatment sites.
Declarations
Ethical approval and consent to participate: An ethical approval certificate had been obtained from Bahir Dar University Ethical approval committee, Bahir Dar University, Ethiopia with reference number: RCS/1412/2012. In data collection, there was no written or verbal consent from participants because of the use of secondary data.
Consent for publication: This manuscript has not been published elsewhere and is not under consideration by any other journal. The authors agreed this manuscript be submitted to this journal for publication.
Availability data and privacy regulations: The data used in the current investigation is available to the corresponding authors. The data accessed in the current investigation complied with relevant data protection and privacy regulations, and this study was conducted in accordance with the Declaration of Helsinki.
Funding:
Not applicable
Disclosure:
The author declared that there is no conflict of interest regarding the publication of this manuscript.
References
- Eren-Yazicioglu CY, Yigit A, Dogruoz RE, Yapici-Eser H (2021) Can GLP-1 Be a Target for Reward System Related Disorders? A Qualitative Synthesis and Systematic Review Analysis of Studies on Palatable Food, Drugs of Abuse, and Alcohol. Front Behav Neurosci 14:614884.
- Klausen KM, Thomsen M, Wortwein G, Fink‐Jensen A (2022) The role of glucagon‐like peptide 1 (GLP‐1) in addictive disorders. Br J Pharmacol 179(4):625-641.
- Singh G, Krauthamer M, Bjalme-Evans M (2022) Wegovy (semaglutide): a new weight loss drug for chronic weight management. J Investig Med 70(1): 5-13.
- Jerlhag E (2020) Alcohol-mediated behaviours and the gut-brain axis; with focus on glucagon-like peptide-1. Brain Res 1727: 146562.
- Brunchmann A, Thomsen M, Fink-Jensen A (2019) The effect of glucagon-like peptide-1 (GLP-1) receptor agonists on substance use disorder (SUD)-related behavioural effects of drugs and alcohol: A systematic review. Physiol Behav 206: 232-242.
- Suchankova P, Yan J, Schwandt ML, Stangl BL, Caparelli EC, et al. (2015) The glucagon-like peptide-1 receptor as a potential treatment target in alcohol use disorder: evidence from human genetic association studies and a mouse model of alcohol dependence. Transl Psychiatry 5: e583.
- Pedersen CB, Gotzsche H, Moller JO, Mortensen PB (2006) The Danish Civil Registration System: A cohort of eight million persons. Dan Med Bull 53(4): 441-449.
- Pottegard A, Schmidt SA, Wallach-Kildemoes H, Sorensen HT, Hallas J, et al. (2016) Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol 46(3):798-798f.
- Ankarfeldt MZ, Thorsted BL, Groenwold RH, Adalsteinsson E, Ali MS, et al. (2017) Assessment of channeling bias among initiators of glucose-lowering drugs: A UK cohort study. Clin Epidemiol 9: 19-30.
- Schmidt M, Schmidt SAJ, Sandegaard JL, Ehrenstein V, Pedersen L, et al. (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7: 449-490.
- Schwarz AS, Nielsen B, Nielsen AS (2018) Changes in profile of patients seeking alcohol treatment and treatment outcomes following policy changes. J Public Health 26(1): 59-67.
- Austin PC (2014) The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med 33(7): 1242-1258.
- Gibson JE, Hubbard RB, Smith CJP, Tata LJ, Britton JR, et al. (2009) Use of Self-controlled Analytical Techniques to Assess the Association Between Use of Prescription Medications and the Risk of Motor Vehicle Crashes. Am J Epidemiol 169(6): 761-768.
- Petersen I, Douglas I, Whitaker H (2016) Self controlled case series methods: an alternative to standard epidemiological study designs. Bio Med J 354: i4515.
- Thomsen M, Holst JJ, Molander A, Linnet K, Ptito M, et al. (2019) Effects of glucagon-like peptide 1 analogs on alcohol intake in alcohol-preferring vervet monkeys. Psychopharmacology (Berl) 236(2): 603-611.
- Jerlhag E (2018) GLP-1 signaling and alcohol-mediated behaviors; preclinical and clinical evidence. Neuropharmacology 136(Pt B): 343-349.
- Urban NBL, Kegeles LS, Slifstein M, Xu X, Martinez D, et al. (2010) Sex differences in striatal dopamine release in young adults after oral alcohol challenge: a positron emission tomography imaging study with [11C]raclopride. Biol Psychiatry 68(8):689-696.
- ten Kulve JS, Veltman DJ, van Bloemendaal L, Groot PFC, Ruhé HG, et al. (2016) Endogenous GLP1 and GLP1 analogue alter CNS responses to palatable food consumption. J Endocrinol 229(1):1-12.
- ten Kulve JS, Veltman DJ, van Bloemendaal L, Barkhof F, Drent ML, et al. (2015) Liraglutide Reduces CNS Activation in Response to Visual Food Cues Only After Short-term Treatment in Patients With Type 2 Diabetes. Diabetes Care 39(2): 214-221.
- Filippatos TD, Panagiotopoulou TV, Elisaf MS (2014) Adverse Effects of GLP-1 Receptor Agonists. Rev Diabet Stud 11(3-4): 202-230.
- Gage SH, Munafo MR, Smith GD (2016) Causal Inference in Developmental Origins of Health and Disease (DOHaD) Research. Annu Rev Psychol 67:567-585.
- Carvalho AF, Heilig M, Perez A, Probst C, Rehm J (2019) Alcohol use disorders. Lancet 394(10200): 781-792.
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, et al. (2015) Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72(8): 757-766.
- Mohler-Kuo M, Foster S, Gmel G, Dey M, Dermota P (2015) DSM-IV and DSM-5 alcohol use disorder among young Swiss men. Addict Abingdon Engl 110(3): 429-440.
- Plana-Ripoll O, Pedersen CB, Agerbo E, Holtz Y, Erlangsen A, et al. (2019) A comprehensive analysis of mortality-related health metrics associated with mental disorders: a nationwide, register-based cohort study. Lancet Lond Engl 394(10211):1827-1835.
- Rehm J (2011) The risks associated with alcohol use and alcoholism. Alcohol Res Health 34(2):135-143.
- Schuckit MA (2009) Alcohol-use disorders. Lancet 373(9662):492-501.
- Heikkinen M, Taipale H, Tanskanen A, Mittendorfer‐Rutz E, Lähteenvuo M, et al (2021) Real‐world effectiveness of pharmacological treatments of alcohol use disorders in a Swedish nation‐wide cohort of 125 556 patients. Addiction 116(8):1990-1998.
- Maisel NC, Blodgett JC, Wilbourne PL, Humphreys K, Finney JW (2013) Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: when are these medications most helpful?. Addiction 108(2): 275-293.
- Jerlhag E (2020) Alcohol-mediated behaviours and the gut-brain axis; with focus on glucagon-like peptide-1. Brain Res 1727: 146562.
- Holst JJ, Seino Y (2009) GLP-1 receptor agonists: Targeting both hyperglycaemia and disease processes in diabetes. Diabetes Res Clin Pract 85(1):1-3.
- Nilsson M, Gjedde A, Brock B, Gejl M, Rungby J (2018) The effects of incretin hormones on cerebral glucose metabolism in health and disease. Neuropharmacology 136:243-250.
- Volkow ND, Wise RA, Baler R (2017) The dopamine motive system: implications for drug and food addiction. Nat Rev Neurosci 18(12):741-752.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Mekonnen Y, Belay DB, Tegegne AS (2022) Risk Factors Associated With the Frequency of Seizure Attack on People Living With Epilepsy at Felege Hiwot Referral Hospital; Application of A Linear Mixed Model. J Addict Res Ther 13: 499.
Copyright: © 2022 Mekonnen Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1479
- [From(publication date): 0-2022 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 1283
- PDF downloads: 196
