Rising Emergency Admissions in the UK and the Elephant in the Room
Received: 29-Jul-2016 / Accepted Date: 05-Aug-2016 / Published Date: 12-Aug-2016 DOI: 10.4172/2161-1165.1000261
Abstract
Growth in emergency medical admissions in the UK is not following trends consistent with the assumed mechanisms of growth. Is ‘policy-based evidence’ ignoring the existence of very large outbreaks of a novel infectious agent?
Keywords: Emergency care systems; Acute medicine; Deaths/mortality; Dementia; Epidemiology
164452Introduction
It is clear that the demand on the NHS in the UK is rising, and that innovation is required to meet the demand in cost effective ways. Rising numbers of elderly people require non-acute solutions to their end-of-life care [1].
However, it is intrinsically incorrect to assume that deficiencies (real or perceived) in how health care services may be currently delivered are in some way causative of rising demand, rather than contributory to rising demand.
In this respect, my interest in unusual growth in emergency medical admissions was triggered in the early 1990’s when a series of ‘events’ in 1993, 1996 and 1999 led to a period of very high and unexplained growth. The literature surrounding these events has been recently reviewed [2], and unexpected evidence for spatiotemporal patterns similar to those expected from an infectious event has since emerged [3-6].
Actual versus expected growth
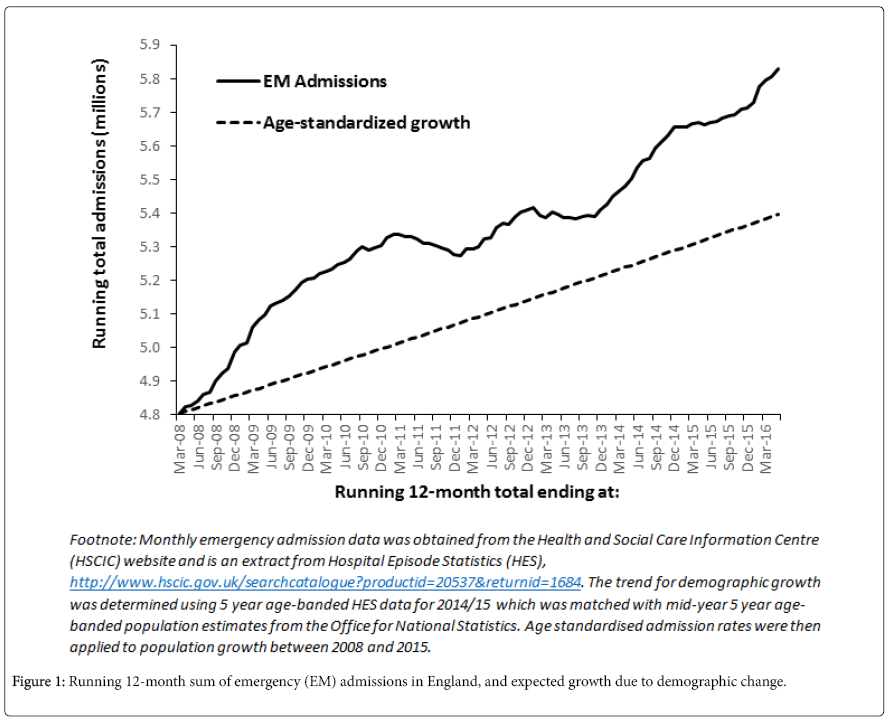
As an example of the disparity between actual and expected growth in emergency admissions, Figure 1 shows a running 12 month total of emergency admissions in England commencing with the 12 month period April 2007 to March 2008. By definition, each point on a running 12 month total chart increments forward by 1 month and gives the running total, hence the second data point in this chart is the total from May 2007 to April 2008, etc.
One of the benefits of a running 12 month total is that underlying seasonality is largely removed from the trend, and that sudden and unexpected step-like changes in activity are revealed as a ramp with onset of the step-change at the foot of the ramp (Figure 1). Also displayed on Figure 1 is the increase in emergency admissions expected due to the ageing population (change in the total population plus change in the age structure).
This chart clearly shows that demand is rising far faster than implied by population growth and change in the age structure, and also partly explains why emergency services are currently struggling to deal with the demand since current staffing and physical capacity have not risen in parallel.
Explaining the trend
Figure 1 requires some further explanation. Firstly, the magnitude of the change during the ‘2008 event’ was slightly exaggerated due to ongoing growth in zero day stay emergency ‘admissions’ arising out of the 2002 A and E four-hour target [7]. However, the contribution from this factor diminished over time such that while emergency admissions increased 3.8% between 2013/14 and 2014/15, the proportion of these which were zero day stay only rose one percentage point from 27.4% to 28.4% respectively [8]. These figures are apposite since the two years span the 2014 ‘event’, and the peculiar increase therefore arises more so from overnight stay admissions than from zero day stay admissions.
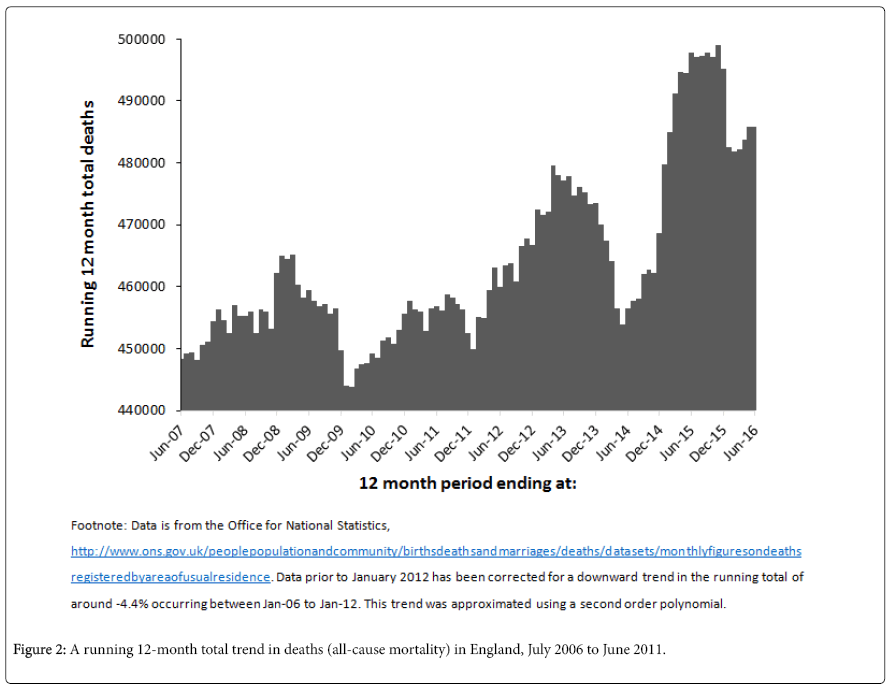
Secondly, while the initiation for the 2012, 2014 and 2016 ‘events’ may be obvious those for 2008 and 2010 are not. These dates have been identified by a parallel change in the total number of deaths (all-cause mortality) occurring at these points [9], and this is demonstrated in Figure 2. In addition, the onset of these events are also marked by a sudden increase in emergency department (ED) attendances, an unexpected increase in NHS staff sickness absence [10], and a wobble in the gender ratio at birth [11]. The assumptions within the calculation of hospital mortality also appears to be invalidated by these events [12]. The 2008 event was also marked by unexplained increases in GP referral which swept across the whole UK (not just England) [13]. While this increase in GP referral is more subdued during the other events, changes in the ratio of follow-up to first attendance also occur in parallel to the changes in deaths, medical admissions and A and E attendances [10]. It would also seem that the unexplained growth in emergency admissions is matched by a parallel unexplained growth in adult appendicitis (especially with increasing age), with inflections in the trends at the onset of the ‘events’ [14]. These events can be traced back to the 1950’s [9], and cannot be attributed to a recent period of austerity in health and social care budgets, as some have claimed [15]. Although along with other factors; austerity may well be a contributory but not a causative factor [2].
The next intriguing fact is that during these events both deaths and medical admissions show evidence for spatial spread within the UK. Such differences in the point of onset can be observed at both local authority level and at very small area level within each local authority, i.e. there is both inter- and intra-local authority spread [3-6]. Factors relating to acute admission thresholds (and counting of zero day stay admissions) have been excluded as a possible cause. This was achieved by investigating the small area behaviour within the catchment population of a number of acute hospitals during the 2008, 2010 and 2012 events [3-6,10]. Hence Figure 1 is actually a composite picture of small-area changes across the whole of England.
Lastly, in a running 12-month total chart the recurring ‘ramp-like’ features which appear to be associated with periods of high growth, are in fact indicative of explosive growth. This explosive growth occurs in an almost step-like fashion, such that the foot of the ramp marks a sudden transition to higher admission rates, i.e. in a running total a sudden increase in admission rates takes 12 months for the stepchange to be fully reflected in the running 12-month total. It is this sudden change in admission rates (and persons approaching death) which overwhelms the resources in both secondary, primary and social care.
Whatever else may or may not be happening, it is also becoming increasingly clear that those suffering from neurological disorders (Alzheimer’s disease, dementia and Parkinson’s disease) are especially prone to dying during the periods delineated by these events [16,17].
The Link between Deaths and Admissions
While deaths in Figure 2 generally revert back to the baseline after each event/outbreak (see below for discussion of the 2016 event), it is evident that emergency admissions (Figure 1) attempt to revert back but the next outbreak lifts the total to a new high before this can fully occur. Something similar to a persistent infection appears to be occurring. Deaths and emergency admissions are primarily linked via the fact that emergency admissions mainly occur during the last 6 months of a person’s life [1,18], hence it is the marginal changes in total deaths (as opposed to age-standardized mortality) which lead to marginal changes in emergency admissions. During these events there are somewhere in excess of 10 additional emergency admissions for every additional death [2,19].
However, there are additional differences between Figures 1 and 2. Firstly, deaths mainly occur in those aged over 85 while admissions occur mainly above age 65, hence the two Figures reflect the impact of the events/outbreaks on different age groups. This mismatch between ages therefore appears to partly explain the differences in behaviour between Figures 1 and 2. In addition, those who die can no longer be admitted, while those infected (but still alive) can go on to have further admissions.
A Further Outbreak in 2016
Since 2000 these events appear to have occurred every two years and both Figures 1 and 2 indicates the possibility of a 2016 outbreak. Tables 1 (England and Wales) and 2 (London) gives the likely dates for onset of the 2016 event/outbreak in the 80 largest regions and counties in England and Wales and also for London. Typical spread between regions and counties is seen in Tables 1 and 2. Both West Midlands and Yorkshire and the Humber appear to have the highest proportion (46% of counties/cities) of early initiation in Feb-16. Also included at the bottom of Table 1 are the results for the local authority areas in Berkshire where the spread of this agent was studied in detail during the 2012 event/outbreak [3]. As in this previous study, Slough appears to initiate early in the outbreak [3]. Table 2 also appears to confirm previous results for a generally later start for these outbreaks in London [9], which has the lowest population average age in the UK, with 45% of local authority areas initiating after April 2016.
| Region | County | 16-Feb | 16-Mar | 16-Apr | 16-May | 16-Jun | 16-Jul |
|---|---|---|---|---|---|---|---|
| England | Entire Country | → | |||||
| East | Cambridgeshire | → | |||||
| East | Central Bedfordshire | → | |||||
| East | Essex | → | |||||
| East | Hertfordshire | → | |||||
| East | Norfolk | → | |||||
| East | Suffolk | → | |||||
| East | Entire Region | → | |||||
| East midlands | Derby | → | |||||
| East midlands | Leicester | ||||||
| East midlands | Leicestershire | → | |||||
| East midlands | Lincolnshire | → | |||||
| East midlands | Northamptonshire | → | |||||
| East midlands | Nottingham | → | |||||
| East midlands | Nottinghamshire | → | |||||
| East midlands | Entire Region | → | |||||
| London | Barnet | → | |||||
| London | Bromley | → | |||||
| London | Croydon | → | |||||
| London | Outer London | → | |||||
| London | Entire Region | → | |||||
| North east | County Durham | → | |||||
| North east | Newcastle on Tyne | → | |||||
| North east | Sunderland | → | |||||
| North east | Tyne and Wear | → | |||||
| North east | Entire Region | → | |||||
| North west | Bolton | → | |||||
| North west | Cumbria | → | |||||
| North west | Greater Manchester | → | |||||
| North west | Lancashire | → | |||||
| North west | Liverpool | → | |||||
| North west | Manchester | → | |||||
| North west | Merseyside | → | |||||
| North west | Sefton | → | |||||
| North west | Stockport | → | |||||
| North west | Wigan | → | |||||
| North west | Wirral | → | |||||
| South east | Arun | → | |||||
| South east | Buckinghamshire | → | |||||
| South east | East Sussex | → | |||||
| South east | Hampshire | → | |||||
| South east | Kent | → | |||||
| South east | Oxfordshire | → | |||||
| South east | Surrey | → | |||||
| South east | West Sussex | → | |||||
| South east | Entire Region | → | |||||
| South west | Bristol | → | |||||
| South west | Devon | → | |||||
| South west | Dorset | → | |||||
| South west | Gloucestershire | → | |||||
| South west | Somerset | → | |||||
| South west | Wiltshire | → | |||||
| South west | Entire Region | → | |||||
| Wales | Cardiff | → | |||||
| Wales | Swansea | → | |||||
| Wales | Entire Country | → | |||||
| West midlands | Birmingham | → | |||||
| West midlands | Coventry | → | |||||
| West midlands | Dudley | → | |||||
| West midlands | Sandwell | → | |||||
| West midlands | Shropshire | → | |||||
| West midlands | Staffordshire | → | |||||
| West midlands | Stoke-on-Trent | → | |||||
| West midlands | Walsall | → | |||||
| West midlands | Warwickshire | → | |||||
| West midlands | Wolverhampton | → | |||||
| West midlands | Worcestershire | → | |||||
| West midlands | Entire Region | → | |||||
| Yorkshire and humber | Bradford | → | |||||
| Yorkshire and humber | Doncaster | → | |||||
| Yorkshire and humber | East Riding | → | |||||
| Yorkshire and humber | Kirklees | → | |||||
| Yorkshire and humber | Leeds | → | |||||
| Yorkshire and humber | North Yorkshire | → | |||||
| Yorkshire and humber | Rotherham | → | |||||
| Yorkshire and humber | Sheffield | → | |||||
| Yorkshire and humber | South Yorkshire | → | |||||
| Yorkshire and humber | Wakefield | → | |||||
| Yorkshire and humber | West Yorkshire | → | |||||
| Yorkshire and humber | Entire Region | → | |||||
| Monthly deaths in England and Wales by area of residence were obtained from the Office for National Statistics. A running 12-month total was constructed and initiation was assumed to occur in the month after a minimum of deaths was seen in the running 12-month total. | |||||||
Table 1: Likely apparent initiation date for a 2016 outbreak based on monthly deaths. (A Jul-16 date indicates that initiation may occur in or after July 2016. Initiation date for the larger regions will be driven by the largest population groups affected by the outbreak).
| Region | Local Authority | 16-Feb | 16-Mar | 16-Apr | 16-May | 16-Jun | > Jul-16 |
|---|---|---|---|---|---|---|---|
| London | Total | → | |||||
| Inner London | Total | → | |||||
| Inner London | Camden | → | |||||
| Inner London | City of London | → | |||||
| Inner London | Hackney | → | |||||
| Inner London | Hammersmith and Fulham | → | |||||
| Inner London | Haringey | → | |||||
| Inner London | Islington | → | |||||
| Inner London | Kensington and Chelsea | → | |||||
| Inner London | Lambeth | → | |||||
| Inner London | Lewisham | → | |||||
| Inner London | Newham | → | |||||
| Inner London | Southwark | → | |||||
| Inner London | Tower Hamlets | → | |||||
| Inner London | Wandsworth | → | |||||
| Inner London | Westminster | → | |||||
| Outer London | Total | → | |||||
| Outer London | Barking and Dagenham | → | |||||
| Outer London | Barnet | → | |||||
| Outer London | Bexley | → | |||||
| Outer London | Brent | → | |||||
| Outer London | Bromley | → | |||||
| Outer London | Croydon | → | |||||
| Outer London | Ealing | → | |||||
| Outer London | Enfield | → | |||||
| Outer London | Greenwich | → | |||||
| Outer London | Harrow | → | |||||
| Outer London | Havering | → | |||||
| Outer London | Hillingdon | → | |||||
| Outer London | Hounslow | → | |||||
| Outer London | Kingston upon Thames | → | |||||
| Outer London | Merton | → | |||||
| Outer London | Redbridge | → | |||||
| Outer London | Richmond upon Thames | → | |||||
| Outer London | Sutton | → | |||||
| Outer London | Waltham Forest | → |
Table 2: Likely apparent initiation dates for local authority residents in London.
As has been previously noted admissions appear to initiate around one month before deaths [19], i.e. illness precedes eventual death, strongly implicating an infectious aetiology. This is seen in the one-month difference in the inflection (initiation) points between Figures 1 and 2.
The 2016 event is very concerning. As in previous events, deaths are supposed to revert back to the baseline position following cessation of the event. This does not occur following the 2014 event, and deaths then jump to a new higher level. In a running 12 month total a spike in deaths arising from the Jan-2015 influenza event will have left the running total by Dec-15 (as seen in Figure 2). However, it has been proposed that the 2014 event may have interacted with the influenza outbreak in January 2015, with this interaction possibly potentiated by vaccination of the population (in late 2014) with a poorly matched vaccine [8,19]. This remains conjecture, but requires urgent investigation.
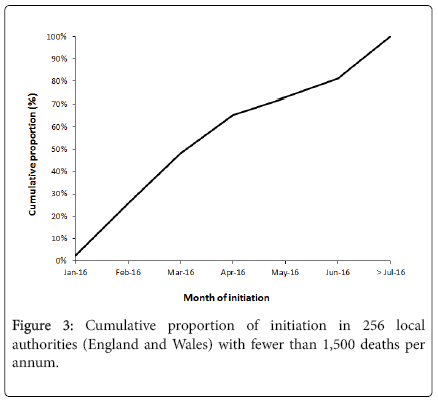
These events/outbreaks show variable levels of synchrony ranging from very low in the 2010 outbreak to very high in the 2014 outbreak. In this respect, Figure 3 suggests that the 2016 outbreak may have exhibited unusually high synchrony with 65% of smaller local authority areas initiating by April 2016. Further investigation is required to examine if the Jan-15 influenza outbreak acted to enhance the synchrony in the 2016 event/outbreak.
An estimate of the increase in deaths due to the 2016 event/outbreak can be determined by extrapolating the slope of the running total to the point 12 months from initiation. Hence in England and Wales deaths actually jumped (step-increase) to around 530,000 per annum, while the baseline position should have been somewhere around 485,000 deaths per annum, i.e. the 2016 event/outbreak has added somewhere around 45,000 extra deaths (and by extrapolation at least 450,000 extra emergency admissions). The figure of 45,000 extra deaths is roughly in line with previous events [2,9]. We need to ask the question as to why are notification of these events/outbreaks being left to an individual researcher rather than the usual route via government agencies, along with appropriate public health measures?
The events are international in scope
A potential criticism of this work is that a genuine infectious outbreak would not be confined to the UK. In this respect the same behaviour has been demonstrated across 27 European Countries [2], and also in Australia, New Zealand and the USA [20,21]. Unpublished analysis reveals the same behaviour in Canadian provinces. Also note that the four counties comprising the UK run separate health care systems with different funding, organisation and policies – yet the same events occur across each country [2].
Conclusion
Clearly something highly unusual is occurring, leading to spurts of far higher growth in both deaths and emergency attendances/ admissions than could otherwise be anticipated. It is mathematically impossible for this behaviour to be replicated in both deaths and emergency admissions (mostly medical), at all levels of geographic size, and roughly synchronously around the world. These events appear to evade traditional disease surveillance methods by virtue of the unique kinetics of spread, and duration of the effects of ‘infection’ [22].
While I have proposed that these unusual events may be due to a novel type of infectious outbreak involving a relatively difficult to transmit agent [19], it is important that others investigate further. We need to uncover root causes, rather than assuming it is all to do with an ageing population and/or deficiencies in the way in which care is delivered [8].
The NHS is a very political arena, and it is suspected that anything which contradicts the policy direction (such as Figures 1 and 2) is never shown to the NHS (or the public) least they question the wisdom of the science behind current policy. Indeed, my attempts to raise this issue with UK government agencies appears to have been met with ‘discreet’ silence, and one can only assume that the discovery is politically embarrassing, and conflicts with the accepted wisdom of ‘policy-based evidence’.
Conflict of Interest
None to declare.
Footnote
In this short opinion piece, it has not been possible to cover all aspects of these events/outbreaks in detail. For further studies including the effects on hospital bed occupancy and health care costs refer to: www.hcaf.biz/2010/Publications_Full.pdf.
Key Messages
What is already known on this subject?
• Emergency admissions and emergency department attendances have been growing faster than expected for many years.
• Social factors and the way in which health and social care are organised are contributory to these trends but not causative.
What might this study add?
• Emergency and unscheduled demand is growing via a series of unexplained spurts or step-like changes.
• These spurts are accompanied by increases in sickness absence and a wobble in the gender ratio at birth.
• Both deaths and medical admissions show small area spread during these events
• Existing mechanisms cannot explain this growth.
References
- Payne G, Laporte A, Deber R, Coyte P (2007) Counting backward to health care’s future: Using time-to-death modelling to identify changes in end-of-life morbidity and the impact of aging on health care expenditures. Milbank Quarterly 85: 213-257.
- Jones R (2015) Recurring Outbreaks of an Infection Apparently Targeting Immune Function, and Consequent Unprecedented Growth in Medical Admission and Costs in the United Kingdom: A Review. Brit J Med Medical Res 6: 735-770.
- Jones R, Beauchant S (2015) Spread of a new type of infectious condition across Berkshire in England between June 2011 and March 2013: Effect on medical emergency admissions. Brit J Med Medical Res 6: 126-148.
- Jones R (2015) Infectious-like spread of an agent leading to increased medical hospital admission in the North East Essex area of the East of England. Brit J Med Medical Res 1: 98-111.
- Jones R (2015) Small area spread and step-like changes in emergency medical admissions in response to an apparently new type of infectious event. FGNAMB 1: 42-54.
- Jones R (2016) Deaths in English Lower Super Output Areas (LSOA) show patterns of very large shifts indicative of a novel recurring infectious event. SMU Medical Journal 3: 23-36.
- Jones R (2009) Trends in emergency admissions. Brit J Healthc Manage 15: 188-196.
- Jones R (2016) The unprecedented growth in medical admissions in the UK: the ageing population or a possible infectious/immune aetiology? Epidemiology (Sunnyvale) 6: 1000219
- Jones R (2015) A previously uncharacterized infectious-like event leading to spatial spread of deaths across England and Wales: Characteristics of the most recent event and a time series for past events. Brit J Med Medical Res 5: 1361-1380.
- Jones R (2015) Are emergency admissions contagious? Brit J Healthc Manage 21: 227-235.
- Jones R (2013) Do recurring outbreaks of a type of infectious immune impairment trigger cyclic changes in the gender ratio at birth? Biomed International 4: 26-39.
- Jones R (2015) A ‘fatal’ flaw in hospital mortality models: How spatiotemporal variation in all-cause mortality invalidates hidden assumptions in the models. FGNAMB1: 82-96.
- Jones R (2012) Increasing GP referrals: collective jump or infectious push? Brit J Healthc Manage 18:487-495.
- Jones R (2015) An unexpected increase in adult appendicitis in England (2000/01 to 2012/13): Could cytomegalovirus (CMV) be a risk factor? Brit J Med Medical Res 5: 579-603.
- Loopstra R, McKee M, Katikireddi S, Taylor-Robinson D, Barr B, Stuckler D (2016) Austerity and old-age mortality in England: a longitudinal cross-local area analysis, 2007-2013. J Roy Soc Med 109: 109-116.
- Jones R, Goldeck D (2014) Unexpected and unexplained increase in death due to neurological disorders in 2012 in England and Wales: Is cytomegalovirus implicated? Med Hypotheses 83: 25-31.
- Jones R (2016) A presumed infectious event in England and Wales during 2014 and 2015 leading to higher deaths in those with neurological and other disorders. J Neuroinfectious Dis 7: 1000213.
- Jones R (2012) End of life care and volatility in costs. Brit J Healthc Manage 18: 374-381.
- Jones R (2016) Is cytomegalovirus involved in recurring periods of higher than expected death and medical admissions, occurring as clustered outbreaks in the northern and southern hemispheres? Brit J Med Medical Res 11: 1-31.
- Jones R (2015) Deaths and international health care expenditure. Brit J Healthc Manage 21: 491-493.
- Jones R (2015) A time series of infectious-like events in Australia between 2000 and 2013 leading to extended periods of increased deaths (all-cause mortality) with possible links to increased hospital medical admissions. InteJ Epidemiologic Res 2: 53-67.
- Jones R (2016) A fatal flaw in mortality-based disease surveillance. Brit J Healthc Manage 22: 143-145.
Citation: Jones RP (2016) Rising Emergency Admissions in the UK and the Elephant in the Room. Epidemiology (Sunnyvale) 6:261. DOI: 10.4172/2161-1165.1000261
Copyright: © 2016 Jones RP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11261
- [From(publication date): 8-2016 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 10337
- PDF downloads: 924