Case Report Open Access
Right Sided Colonic Varices: 2 Cases and Review of the Literature
Erwin-Jan M. van Geenen* and Geert JA
Department of Gastroenterology and Hepatology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
- Corresponding Author:
- Erwin-Jan M. van Geenen
Department of Gastroenterology and Hepatology, Radboud University Nijmegen Medical Center
Nijmegen, The Netherlands
Tel: 0031636170086
E-mail: erwin.vangeenen@radboudumc.nl
Received Date: July 9, 2015 Accepted Date: October 13, 2015 Published Date: October 20, 2015
Citation: van Geenen EM, Geert JA (2015) Right Sided Colonic Varices: 2 Cases and Review of the Literature. J Gastrointest Dig Syst S13:009. doi:10.4172/2161-069X.1000S13-009
Copyright: © 2015 van Geenen EM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Colonic varices (CV) are a rare cause of lower gastrointestinal bleeding. Although approximately 90 cases of CV have been reported, mainly in bleeding patients with portal hypertension, the prevalence of (asymptomatic) CV is likely to be underestimated.
Study/Results: We report two cases of portal hypertension related colonic varices and a literature review of colonic varices. These cases demonstrate the two clinical extremities: hardly any complaints versus medically refractory rectal blood loss and anemia, which ultimately needed surgical intervention.
Conclusion: Colonic varices are rare and more prevalent in patients with liver cirrhosis. Especially in this group, rectal bleeding and anemia with normal upper GI investigations, should be investigated with a colonoscopy. Treatment of CV is not well established and depends on the etiology and severity of clinical presentation.
Keywords
Colon; Varices; Portal hypertension; Liver cirrhosis
Case 1
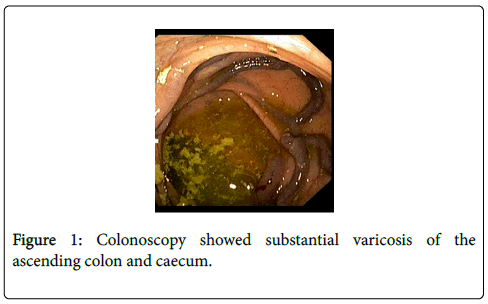
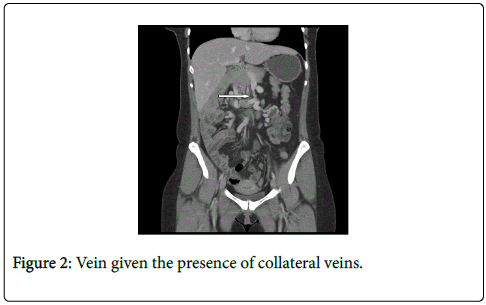
A 34-year-old woman with a history of chronic diarrhea that had started during the third trimester of pregnancy was referred for colonoscopy to the endoscopy unit. She reported a change in stool color suggestive for melaena . Six months before, she had given birth to a healthy son. Laboratory results including CRP, hemoglobin, and serum creatinin were within normal ranges. She reported no abdominal pain or discomfort. During pregnancy at 26 weeks she was admitted to the hospital because of diffuse mild right-sided abdominal pain radiating to the back. Abdominal ultrasound revealed no evidence for gallbladder stones or other abnormalities (Figure 1). These complaints gradually subsided and therefore no additional abdominal imaging was performed. Unexpectedly, colonoscopy showed substantial varicosis of the ascending colon and caecum. Because of her previous complaints, recent pregnancy and colonic varices, portal hypertension was suspected and an abdominal computer tomography (CT) with intravenous contrast was ordered, which showed a longstanding thrombosis of the superior mescenteric, vein given the presence of collateral veins (Figure 2, arrow). The patient was refered to the outpatient vascular medicine clinic to rule out clotting disorders, which indeed were not identified. Multi-disciplinary consultation (vascular surgeon, internist, gastroenterologist) resulted in the decision not to start anti-coagulants. At this point, i.e. six months after her colonoscopy, her hemoglobin has remained stable, the diarrhea has subsided and there are no remaining abdominal complaints.
Case 2
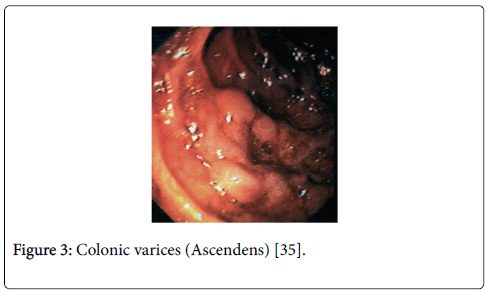
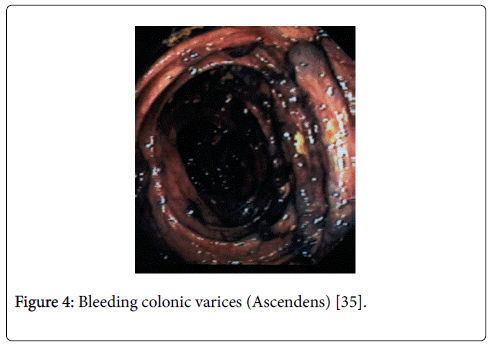
A 58-year-old man with a history of an uncomplicated appendectomy was referred to our outpatient clinic because of melaena and anemia. Apart from fatigue the patient had no medical complaints and used no medication. Physical investigation revealed no abnormalities. Laboratory investigation showed a hemoglobin of 6,8mmol/l. Barium colonography showed no abnormalities. Gastroscopy revealed two submucosal varices in the cardia and post bulbular (Figure 3), without any sign of (recent) bleeding. Endoscopic ultrasound showed multiple collateral veins in the gastric, pancreatic and oesophageal area. Initially, the anemia resolved with a wait and see policy. However, within 2 months the patients presented with recurrent anemia and colonoscopy was performed, which showed major varices in the caecum and ascending colon (Figure 4). Otherwise, the colon and terminal ileum appeared normal Because of suspected portal hypertension, a CT-abdomen was performed, which showed thrombosis of the portal and splenic vein, with extensive collateral vein formation. Propanolol was started in order to reduce the portal pressure. However, the patient remained transfusion dependent (more than 3 units of packed cells per week) and therefore other options were discussed. Because continuous infusion of octreotide (50 mcg/hr) for 1 week initially seemed to decrease the blood loss, we embarked on a trial with the long-acting formulation was started (Octreotide LAR 30 mg/month), but without success. Due to the substantial portal occlusion a transjugular intrahepatic portosystemic shunt (TIPS) was considered technically challenging and eventually a mesocaval shunt was constructed (mesenteric- testicular vein anastomosis), which resulted in a significantly decreased erythrocyte transfusion rate (currently one unit per 2 to 3 weeks). Additional shunting of remaining collateral and abdominal wall veins will be considered in case of increased bleeding.
Discussion
Colonic varices (CV) are part of the spectrum of portal colopathy, and, as one of our cases shows, anemia and bleeding in this entity can be quite profound. CV, which were first reported in 1954 [1], are a rare cause of lower gastrointestinal bleeding, with a reported incidence of 0.07% [2]. The most common sites for colonic varicosis are the rectum and cecum [3]. The etiology of CV can be classified mainly into two groups: Portal hypertension and Idiopathic (familial and non-familial).
Almost 75% of allcases of CV are caused by portal hypertension, as in our two patients [3,4]. Embryologically derived anastomoses betweenthe portal and systemic venous systems exist in the esophagus, terminal ileum, colon, retroperitoneum, and anterior abdominal wall . In general the coronary-azygous anastomosis is the most pronounced, and this favors the development of esophageal varices in the setting of portal hypertension. It has been hypothesized that colonic varices in patients with portal hypertension arise in patients in whom the colonic anastomosis is highly developed [5].
Although approximately 90 cases of CV have been reported, mainly in bleeding patients with portal hypertension, the prevalence of (asymptomatic) CV is likely to be underestimated. In a study of 92 cirrhotic transplant candidates, portal hypertensive colopathy (PHC) and CV were found in respectively: 23.9% and 7.6% [6]. These findings were confirmed by an Italian study that reported 54% PHC and 31% CV in cirrhotic patients [7]. This study revealed no relation between the etiology/severity of cirrhosis and the presence of PHC/CV [7].
Portal hypertension (PH) can be classified in the following groups:
Pre-hepatic, i.e. hypertension of the portal venous system in the absence of liver cirrhosis: (partial)occlusion by external or internal compression of: mesenteric vein [8,9], the portal vein [10-12] splenic vein [13-15] or the complete splenomesenterico-portal axis. Associated conditions are: venous thrombosis (clotting disorder, chronic or acute pancreatitis, pancreatic cancer), and external compression (pancreatic cancer, pseudocysts, retroperitoneal fibrosis)
Hepatic: mainly by cirrhosis [16-22], and schistosomiasis, sardoidosis, sinusoidal obstruction syndrome
Post-hepatic: Budd-chiari, Inferior cava caval obstruction [23], right side heart failure
Idiopathic portal hypertension [24].
Most symptomatic cases of PH and CV present with either anemia or rectal blood loss. However, in our first case the patient presented with right abdominal pain and anemia. The only case-report that described abdominal pain (right lower quadrant) was in a patient with PH and CV based on superior mesenteric vein thrombosis [8], like in our case number 1. It is striking that in no other etiologies of PH and associated CV, abdominal pain is mentioned, like in our first case. One could speculate that pain in SMV thrombosis can arise from more acute and pronounced local ischemia and/or edema, than from other causes of PH.
Idiopathic CV can be classified in a familial and non-familial group [25,26]. Approximately one third of the reported cases of idiopathic colonic varices appear to have a familial component. The incidence of PH CV is equal in males and females [26]. By comparison, idiopathic colonic varices occur more commonly in males than in females. While the majority of non-idiopathic colonic varices have a segmental distribution, half of the reported idiopathic cases are pan-colonic [26].
The treatment of colonic varices is not well established because of scarcity of clinical trials and guidelines. Treatment is dictated by the underlying etiology, severity of the bleeding, as well as the distribution of the varices. In non-severe-cases of anemia a wait and see policy is most appropriate. In transfusion dependent patients, medical, local or surgical therapy is reported. Portal decompression is appropriate in patients with portal hypertension, and has included: beta blocker [18,23] somatostatin infusion/ octreotide [23,27], vascular stenting (TIPS and portal vein stenting) [12,17,19] and heparine [8]. Local control therapy included: catheter embolization [16,19], cyanoacrylate infusion [19,22], argon plasma coagulation [21], and ligation [11,20]. In case of splenic vein occlusion all reported cased advocated a splenectomy [13-15]. And, in uncontrollable cases (or pan-CV) a (partial) colectomy can be performed [9,11].
There is little evidence for an association between pregnancy and portal vein thrombosis [28]. However, in patients with right abdominal pain with or without rectal blood loss and especially in patients with clotting disorders, a pre-hepatic thrombosis of one of the portal tracts should be suspected and ruled out if no explanation of symptoms can be found. In our patient anemia and abdominal pain were mild to moderate, and improved within two weeks. Therefore, no additional investigations were performed, because these (CT-scan, colonoscopy) might possible harm the fetus. The second case of CV was also PHT induced. However, the clinical presentation was more pronounced and medical therapy failed. At that time a TIPS was considered to be technically challenging and surgical portal vein decompression resulted in a significant milder transfusion dependency. However, several large case series have confirmed the feasibility, safety and efficacy of TIPS for the treatment of non-tumoral PVT in liver cirrhosis [29-34]. The rate of technical success is high (75–100%) [29-34]. Once TIPS is successfully inserted, 87–100% of PVT patients can achieve portal vein recanalization [29-34]. Therefore, today, a TIPS most be considered in medical refractory patients with PHT and CV with acute/chronic anemia.
In conclusion, CV are a rare cause of gastrointestinal bleeding, and more prevalent in patients with liver cirrhosis. Especially in this group, rectal bleeding and anemia with normal upper GI investigations, should be investigated with a colonoscopy. On the other hand in asymptomatic patients with CV a PHT work-up and careful family anamnesis is recommended. Treatment of CV is not well established and depends on the etiology and severity of clinical presentation. In case of PHT related CV, a step up approach is proposed: 1. Medical PHT treatment Acute: octreotide, vasopressine, chronic: maintenance: aspecific beta-blockers (Nitrates?), 2. local treatment: Ligation, histoacryl, TIPS, catheter embolization, and 3. Surgery: total/partial colectomy, splenectomy.
References
- (1954) N Engl J Med 250: 434–438
- Han JH, Jeon WJ, Chae HB, Park SM, Youn SJ, et al. (2006) A case of idiopathic colonic varices: a rare cause of hematochezia misconceived as tumor. World J Gastroenterol 12: 2629-2632.
- Hashmonai M, Kopelman D, Engel A, Assalia A (2000) Acute gastrointestinal bleeding from caecal varicosities. Eur J Surg 166: 186-188.
- Klein SD, Hellinger JC, Silverstein ML, Cai Q (2003) Isolated cecal varices as the source of massive lower GI bleeding in a patient with cirrhosis. Am J Gastroenterol 98: 220-221.
- Ganguly S, Sarin SK, Bhatia V, Lahoti D (1995) The prevalence and spectrum of colonic lesions in patients with cirrhotic and noncirrhotic portal hypertension. Hepatology 21: 1226-1231.
- A Nuñez-Martinez O, Gonzalez-Asanza C, Matilla A, Merino B, Rincon D, et al. (2009) Portal hypertensive colopathy is associated with portal hypertension severity in cirrhotic patients. World J Gastroenterol 15: 4781-4787.
- Bresci G, Parisi G, Capria A (2006) Clinical relevance of colonic lesions in cirrhotic patients with portal hypertension. Endoscopy 38: 830-835.
- Navalho M, Duarte I (2008) Superior mesenteric venous thrombosis as a cause of right-side colonic varices: CT and endoscopic findings. Clin Radiol 63: 340-342.
- Ho YP, Lin CJ, Su MY, Tseng JH, Chiu CT, et al. (2005) Isolated varices over hepatic flexure colon indicating superior mesenteric venous thrombosis caused by uncinate pancreatic head cancer--a case report. World J Gastroenterol 11:1886-1889.
- Naef M, Holzinger F, Glättli A, Gysi B, Baer HU (1998) Massive gastrointestinal bleeding from colonic varices in a patient with portal hypertension. Dig Surg 15: 709-712.
- Orozco H, Takahashi T, Mercado MA, Prado-Orozco E, Ferral H, et al. (1992) Colorectal variceal bleeding in patients with extrahepatic portal vein thrombosis and idiopathic portal hypertension. J Clin Gastroenterol 14: 139-143.
- Harville LE, Rivera FJ, Palmaz JC, Levine BA (1992) Variceal hemorrhage associated with portal vein thrombosis: treatment with a unique portal venous stent. Surgery 111: 585-590.
- Van Wijngaarden P, Van der Wiel HE, Tetteroo GW, Bode WA (1997) A patient with gastric fundal varices and colonic varices due to splenic vein thrombosis. Neth J Med 51: 187-191.
- Bradley EL 3rd1 (1987) The natural history of splenic vein thrombosis due to chronic pancreatitis: indications for surgery. Int J Pancreatol 2: 87-92.
- Burbige EJ, Tarder G, Carson S, Eugene J, Frey CF (1978) Colonic varices. A complication of pancreatitis with splenic vein thrombosis. Am J Dig Dis 23: 752-755.
- Ko BS, Kim WT, Chang SS, Kim EH, Lee SW, et al. (2013) A case of ascending colon variceal bleeding treated with venous coil embolization. World J Gastroenterol 19: 311-315.
- Finkenstedt A, Graziadei IW, Nachbaur K, Jaschke W, Mark W, et al. (2009) Transjugular intrahepatic portosystemic shunt in liver transplant recipients. World J Gastroenterol 15: 1999-2004.
- Noubibou M, Douala HC, Druez PM, Kartheuzer AH, Detry RJ, et al. (2006) Chronic stomal variceal bleeding after colonic surgery in patients with portal hypertension: efficacy of beta-blocking agents? Eur J Gastroenterol Hepatol 18: 807-808.
- Wiegand N, Pfiffner R, Bauerfeind P (2006) Ascending colonic variceal bleeding. Gastrointest Endosc 63: 1073-1074.
- Misra SP, Dwivedi M (2006) Ligation of a bleeding colonic varix using an upper gastrointestinal endoscope. Endoscopy 38: 657.
- Schafer TW, Binmoeller KF (2002) Argon plasma coagulation for the treatment of colonic varices. Endoscopy 34: 661-663.
- Chen WC, Hou MC, Lin HC, Chang FY, Lee SD (2000) An endoscopic injection with N-butyl-2-cyanoacrylate used for colonic variceal bleeding: a case report and review of the literature. Am J Gastroenterol 95: 540-542.
- Sohn W, Lee HL, Lee KN (2012) Variceal hemorrhage of ascending colon. Clin Gastroenterol Hepatol 10: A24.
- Francois F, Tadros C, Diehl D (2007) Pan-colonic varices and idiopathic portal hypertension. J Gastrointestin Liver Dis 16: 325-328.
- Zaman L1, Bebb JR, Dunlop SP, Jobling JC, Teahon K (2008) Familial colonic varices--a cause of "polyposis" on barium enema. Br J Radiol 81: e17-19.
- Francois F, Tadros C, Diehl D (2007) Pan-colonic varices and idiopathic portal hypertension. J Gastrointestin Liver Dis 16: 325-328.
- Chakravarty BJ, Riley JW (1996) Control of colonic variceal haemorrhage with a somatostatin analogue. J Gastroenterol Hepatol 11: 305-306.
- Perarnau JM, Bacq Y (2008) Hepatic vascular involvement related to pregnancy, oral contraceptives, and estrogen replacement therapy. Semin Liver Dis 28: 315-327.
- Han G, Qi X, He C, Yin Z, Wang J, et al. (2011) Transjugular intrahepatic portosystemic shunt for portal vein thrombosis with symptomatic portal hypertension in liver cirrhosis. J Hepatol 54: 78-88.
- Qi X, Han G, Fan D (2010) The preferable treatment for cirrhotic portal vein thrombosis: anticoagulation or transjugular intrahepatic portosystemic shunt? Hepatology 51: 713-714.
- Blum U, Haag K, Rossle M (1995) Noncavernomatous portal vein thrombosis in hepatic cirrhosis: treatment with transjugular intrahepatic portosystemic shunt and local thrombolysis. Radiology 195: 153-157.
- Van Ha TG, Hodge J, Funaki B (2006) Transjugular intrahepatic portosystemic shunt placement in patients with cirrhosis and concomitant portal vein thrombosis. Cardiovasc Intervent Radiol 29: 785-790.
- Luca A, Miraglia R, Caruso S, Milazzo M, Sapere C, et al. (2011) Short- and long-term effects of the transjugular intrahepatic portosystemic shunt on portal vein thrombosis in patients with cirrhosis. Gut 60: 846-852.
- Perarnau JM, Baju A, D'alteroche L, Viguier J, Ayoub J (2010) Feasibility and long-term evolution of TIPS in cirrhotic patients with portal thrombosis. Eur J Gastroenterol Hepatol 22: 1093-1098.
- Wanten GJ, Nagengast FM (2004) [Diagnostic image (190). A man with melaena. Enteral varices due to portal hypertension]. Ned Tijdschr Geneeskd 148: 1034.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14285
- [From(publication date):
specialissue-2015 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 9893
- PDF downloads : 4392