Right Non-Valvular Intraventricular Endocarditis with Pubic Osteomyelitis in an Elderly Non-Drug-User with No Medical History
Received: 29-Mar-2023 / Manuscript No. jcidp-23-93535 / Editor assigned: 31-Mar-2023 / PreQC No. jcidp-23-93535 / Reviewed: 14-Apr-2023 / QC No. jcidp-23-93535 / Revised: 21-Apr-2023 / Manuscript No. jcidp-23-93535 / Published Date: 28-Apr-2023 DOI: 10.4172/2476-213X.1000178
Abstract
Non-valvular right-sided endocarditis is a rare disease. We present the case of a 70-year-old woman with no history of surgery, dental treatment, or drug use who developed groin pain and fever, turning out to have Staphylococcus aureus bacteremia, right-sided intraventricular endocarditis, and pubic osteomyelitis forming an abscess.
Keywords
Echocardiography; Right-sided endocarditis; Intraventricular; Non-valvular; Osteomyelitis pubis; Staphylococcus aureus
Case Presentation
A 70-year-old woman was transported by ambulance after being found lying down on the sidewalk. She was alert with right groin pain and a body temperature of 38.4℃, without fracture of the bone or apparent source of the fever, and was sent home. Three days later, she was admitted to the hospital due to positive blood culture of GPC in clusters. At admission, vital signs were: blood pressure of 106/85 mmHg, pulse of 111 beats/min, breathing frequency 20 breaths/min, blood oxygen saturation of 94% while breathing ambient air, and body temperature of 37.7℃. On physical examination, heart and lung sounds were normal. Oral cavity was clean with no apparent decayed tooth. Janeway lesion or Osler nodes were absent. Tenderness in the right groin and pubic tubercle region as well as numerous scratches on the dry skin in the extremities were notable. She had no medical, surgical, dental, or intravenous drug use history. She was taking no medication or supplement. She did not smoke or drink alcohol.
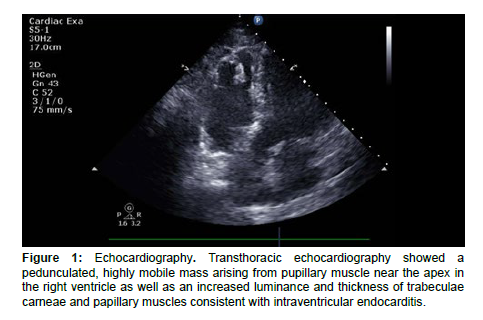
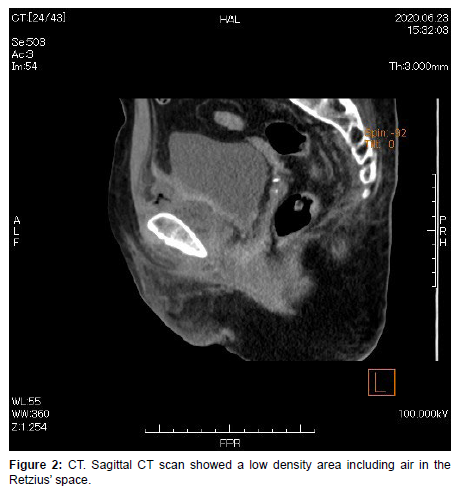
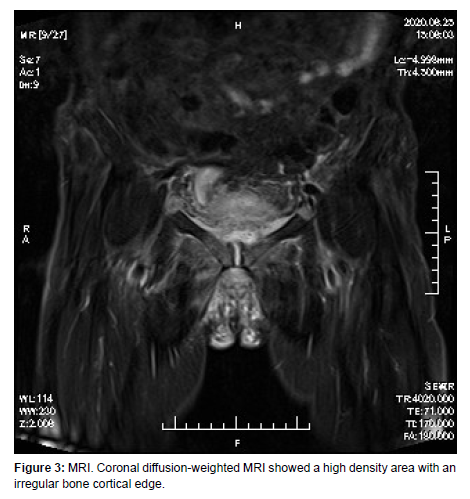
Blood tests revealed elevated white blood cell counts of 10,700/ μl with 84% neutrophils and C-reactive protein of 24.84 mg/dL. Blood glucose was 156 mg/dl with HbA1c of 5.8%. Chest X-Ray and electrocardiography were unremarkable. Blood culture grew methicillinsensitive Staphylococcus aureus. Transthoracic echocardiography (TTE) revealed a pedunculated, highly mobile mass arising from pupillary muscle near the apex in the right ventricle (Figure 1, Video 1) with a width of 9.6mm and length of 18.6mm. TTE showed neither tricuspid regurgitation nor ruptured papillary muscle, nor apical RV wall motion abnormalities, nor RV apical aneurysm. Abdominal CT and MRI (Figures 2 and 3) revealed pubic osteomyelitis with abscess formation. Contrast-enhanced CT of the chest and abdomen showed no apparent thromboembolism and tumor.
With two major criteria in the Modified Duke’s criteria satisfied, a diagnosis of right-sided non-valvular IE was made. Intravenous vancomycin was immediately started, switched to cephazolin after the sensitivity tests and the negative second blood culture confirmed. Warfarinization was also started with concern of possibility the floating mass could be thrombosis. Serial imaging studies during hospital stay showed persisting but not worsening vegetation. Patient recovered without complication after four-week treatment and was discharged on foot with continued cephalexin.
WBC counts and CRP level decreased to normal with negative blood culture and clinical improvement. Patient has been followed-up for 10 months, doing well without recurrence after finishment of oral antibiotics of 8 weeks. The patient was treated with warfarin for three months. Organized vegetation in the right heart and partially destroyed pubic bone will be carefully followed continuously.
Figure 1: Echocardiography. Transthoracic echocardiography showed a pedunculated, highly mobile mass arising from pupillary muscle near the apex in the right ventricle as well as an increased luminance and thickness of trabeculae carneae and papillary muscles consistent with intraventricular endocarditis.
Discussion
Staphylococcus aureus, a Gram-positive bacterium colonizing nares, skin, and the gastrointestinal tract, frequently become more invasive and cause life-threatening infections such as bacteremia, abscesses of various organs, osteomyelitis, endocarditis, and sepsis [1].
Right-sided IE accounts for 5% to 10% of all IE cases and is usually a tricuspid valvular infection seen mainly in intravenous drug abusers in the Western countries [2]. In Japan, right-sided IE is mostly seen in patients with congenital heart diseases. In recent years, IE associated with cardiac implantable electronic devices and indwelling central venous catheters has increased in number. Although the tricuspid valve is involved in almost 90% of right-sided IE, infectious vegetation in other structures such as the pulmonary valve, papillary muscle, or muscular bundle have been reported [3].
Non-valvular cardiac infection most commonly occurs on previously damaged endocardium usually associated with devices such as graft material or pacemakers, or, rarely, on primary tumors such as myxomas. Risk factors include cardiac disease, diabetes mellitus, and malignancy. The clinical presentations of non-valvular IE are subtle and diagnoses are difficult to make, often resulting in delayed treatment and poor survival rates. Complications include peripheral embolisation, cardiac rupture, and pericarditis.
Pubic osteomyelitis accounts for only 2% of all osteomyelitis [4]. It is usually seen among young athletes or as a complication after intrapelvic surgeries. The presence of intense local pain in association with fever should prompt work-up such as blood chemistry, microbiology and diagnostic imaging. Puncture of the infection site or MRI being required for precise diagnosis, pubic osteomyelitis might be easily overlooked or misdiagnosed. To our knowledge, this is the first case of pubic osteomyelitis associated with right-sided non-valvular IE.
In S. aureus bacteremia, prompt identification and eradication of portal of entry and infective/metastatic foci are essential [1]. Although dental and vascular injuries are commonly attributable to endocarditis, chronic skin problems such as dry skin with frequent scratched injury are also possible entries [4]. Chronic scratching leads to worsening of an existing defect in the epidermal barrier, which can allow S. aureus invasion into the bloodstream and subsequent systemic infections. Separate cases of atopic dermatitis-related systemic S.aureus infection, one with infective endocarditis and the other with septic osteomyelitis, have been reported [5]. With no other apparent cause, the entry of Staphylococci in this case may be considered to be deep scratches of dry skin.
We report a rare case of right-sided non-valvular intraventricular endocarditis with pubic osteomyelitis in an elderly woman of no known history of drug abuse, congenital heart disease, or surgical history. Endocarditis should be sought in pubic osteomyelitis associated with Staphylococcus bacteremia if there was no history of injury or surgery. Although difficult to identify, persistent skin scratches could be an entry point, as this case suggests.
Acknowledgements
The authors thank Dr Sugaya, Dr Onoda , Dr Hirata, Ito Municipal Hospital, for his contribution to patient care.
Funding Sources
No funding was received for this article.
Disclosures
The authors have no conflicts of interest to disclose.
References
- Krishna S, Miller LS (2012) Innate and adaptive immune responses against Staphylococcus aureus skin infections. Semin Immunopathol 34:261-280.
- Shmueli H, Thomas F, Flint N (2020)Right-Sided Infective Endocarditis 2020:Challenges and Updates in Diagnosis and Treatment. J Am Heart Assoc 9: e017293.
- Nakauchi Y, Tanigychi M, Miyamura Y (2007) Pulmonary Septic Embolism with Right Side Infectious Endocarditis and Ventricular Septal Defect: A Case Report. J Cardiol 50:383–387.
- Woodun H, Bouayyard S, Sahib S (2020) Tricuspid valve infective endocarditis in a non-IVDU patient with atopic dermatitis. Oxf Med Case Reports 24: 2020:omaa045.
- Patel D, Jahnke MN (2015) Serious Complications from Staphylococcal aureus in Atopic Dermatitis. Pediatr Dermatol 32:792-796.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Manabe T, Tanaka M, Kawai K (2023) Right Non-Valvular Intraventricular Endocarditis with Pubic Osteomyelitis in an Elderly Non-Drug-User with No Medical History. J Clin Infect Dis Pract, 8: 178. DOI: 10.4172/2476-213X.1000178
Copyright: © 2023 Manabe T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1063
- [From(publication date): 0-2023 - Jul 04, 2025]
- Breakdown by view type
- HTML page views: 808
- PDF downloads: 255