Research Article Open Access
Review of Common Pathogens in Deep Sternal Wounds, Blood Stream and Bone Infections in Patients Following Sternotomy: A 10 Year Follow up
Michal Benkler, Ori Shulman, Yoav Avrahamy, David Mendes, Yoav Erosh, Ron Fishel, David Ben Harosh, Amos Leviav and Dana Egozi*
The Department of Plastic and Reconstructive Surgery, Kaplan Medical Center, Rehovot, Israel
- *Corresponding Author:
- Dana Egozi
The Department of Plastic and Reconstructive Surgery
Kaplan Medical Center, Rehovot, Israel
Tel: 97289441294
E-mail: danaeg@clalit.org.il
Received date: July 12, 2017; Accepted date: July 27, 2017; Published date: July 30, 2017
Citation: Benkler S, Shulman O, Avrahamy Y, Mendes D, Erosh Y, et al. (2017) Review of Common Pathogens in Deep Sternal Wounds, Blood Stream and Bone Infections in Patients Following Sternotomy: A 10 Year Follow up. J Infect Dis Ther 5:327. doi: 10.4172/2332-0877.1000327
Copyright: © 2017 Benkler M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Background: Deep sternal wound infections, mediastinitis and sternal osteomyelitis are devastating and life-threatening complications of median-sternotomy incisions after cardiac surgical procedures. The incidence of surgical wound infection in sternotomies is relatively high among heart disease patients since these patients are burdened with a high number of risk factors compared to the general population.
Purpose: This study focusses on microbiological data of deep sternal wounds, alongside blood and bone cultures to help define early and appropriate antibiotic therapy following debridement and reconstructive surgery. Furthermore, this study discusses whether antibiotic treatment of sepsis can rely on preliminary wound cultures.
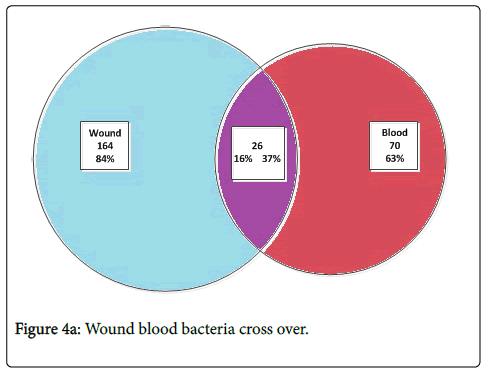
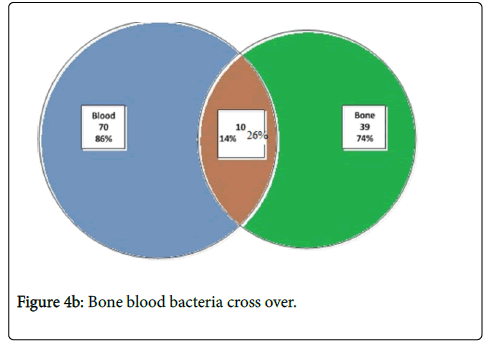
Results: The most commonly cultured organism from deep sternal wound infections was Staphylococcus and the most commonly cultured Gram-negative organism was Pseudomonas. All Gram-negative organisms combined together represented approximately 50% of all cultures. We found that 37% of blood culture pathogens were initially found in wound cultures, and 14% of blood culture organisms were first identified in bone cultures. From a different prespective, 16% of the organisms isolated from the wound and 26% of the organisms isolated from the bone were later found to involve the blood.
Conclusions: The initial antibiotic regimen should be broad spectrum, covering both Gram-positive and Gram-negative organisms. We demonstrate that for osteomyelitis of the sternum, antibiotic treatment for a relatively short period of two weeks is adequate alongside thorough debridement and reconstruction with a vascularized soft tissue flap (pectoral major). Furthermore, the initial antibiotic regimen during sepsis may partially rely on preliminary wound cultures since a third of the pathogens found in the blood were first identified in wound cultures.
Keywords
Deep sternal wound infection; Microbiological cultures– sternum; Wound & blood; Antibiotic treatment protocol; Duration of antibiotic treatment; Sepsis
Background
Deep sternal wound infection (DSWI), mediastinitis and sternal osteomyelitis (SOM) are major complications of median sternotomy incisions after cardiac surgical procedures (coronary artery bypass graft (CABG) or heart valve repair or replacement surgery). These complications are all associated with prolonged hospitalization, increased healthcare costs and impaired quality of life, representing an economic and social burden. DSWI, as defined by the CDC’s (standardized centers of disease control) surveillance criteria, involves the layers beneath the skin and subcutaneous tissue. It presents with purulent drainage from the deep layer or surgical wound dehiscence on the background of fever, localized pain or tenderness and an abscess or other observable evidence of infection on direct examination, histopathology and radiology. According to the CDC’s classifications, the infection of surgical wounds of sternotomies should be defined as (A) superficial if only the skin and subcutaneous tissue are involved, (B) deep when the infection reaches the sternum but does not involve it and (C) organ/space when sternal SOM or mediastinitis occurs [1]. Many mechanisms have been proposed to explain the development of sternal wound infections. Theories include inadequate sternal fixation leading to instability and dehiscence of the overlying skin incision [2], inadequate surgical drainage or localized ischemic osteomyelitis [3]. Numerous risk factors have been suggested including: hypertension, ischemic heart disease, diabetes, emergent surgery for acute myocardial ischemia, smoking and re-operation. The incidence of superficial surgical wound infection in sternotomies should be similar to that in any clean surgical procedure (i.e. approximately 2%). However, the infection rate is roughly three times this value among heart disease patients due to their higher number of risk factors compared to the general population [4-6]. The rate of sternal wound infection varies in different reports ranging from 0.15%-8%, with the majority reporting an average of 3% for both superficial and deep sternal wound infection. Of note, the mortality rate incidence ranges between 10-52% [7-12]. The prevalence of positive blood cultures was found to be significantly higher among deep sternal wound infection patients in comparison with superficial surgical wound infection patients. Successful management requires early recognition based on a high index of suspicion, detailed physical examination, appreciation of the clinical signs and symptoms, timely imaging studies and prompt surgical therapy [1]. Although several therapeutic strategies are currently used in clinical practice, there is a lack of evidence-based surgical consensus for treating this surgical complication. In most cases, treatment involves surgical revision with debridement of all foreign bodies as well as infected and necrotic tissue, which gives rise to abundant dead space. Subsequent reconstruction with vascularized soft tissue flaps, such as omentum or pectoralis major muscle, may be utilized. Alternatively, open dressing and vacuum-assisted therapy may be used [5,7,10]. Despite widespread infection control practices and routine antibiotic prophylaxis, the incidence of deep sternal wound infection has remained stable over time. Little is known about the optimal antibiotic management and data is scarce, in particular regarding the duration of therapy which can range from a few weeks to a few months, depending on the severity of the infection and the presence of osteomyelitis. Early microbiological diagnosis and the use of appropriate antibiotic therapy should improve outcomes by allowing targeted antibiotic treatment, thereby improving morbidity and mortality. This study focuses on the microbiological data of deep sternal wound, bloodstream infections and osteomyelitis to determine the appropriate empiric antibiotic treatment. Furthermore, the relevance and utility of early sternal wound and bone cultures to predict the pathogen during sepsis were analyzed.
Materials and Methods
A ten year retrospective analysis (2005-2014) of microbiological data was conducted in the department of Plastic and Reconstructive Surgery, at the Kaplan Medical Center, under the Helsinki committee permission number 205-14-KMC. A demographic analysis of mean age, sex and risk factor stratification (hypertension, ischemic heart disease, diabetes mellitus, emergent surgery for acute myocardial ischemia, smoking and re-operation) was performed, and data regarding previous operations (CABG, heart valve repair or replacement surgery) was collected.
Microbiological data was collected from bone cultures (taken during surgery), wound cultures (swabs taken during hospitalization or outpatient facilities), blood cultures and resistant bacteria cultures (Meticilin resistant Staphylococcus aureus (MRSA) and Imipenem resistant Gram negative rods, Pseudomonas, Acinetobacter and Klebsiella. Cultures were examined using the Bactec 9240 system (Bacton Dickinson) and tested for susceptibility to different antibiotics in a VITEK automated identification system according to the clinical and laboratory standards institute. All patients in this study underwent radical debridement of infected bone and soft tissue and subsequent reconstruction with pectoralis major muscle flaps for the management of DSWI and SOM. In addition, they received empirical broad-spectrum antimicrobial agents, with successive antibacterial treatment based on preliminary and final culture results together with drug sensitivity testing. If sepsis was suspected, broad spectrum antibiotics were started, later to be modified based on the sensitivity of the bacteria cultured.
Patients were divided into four groups, based on the duration of the antibiotic therapy following surgery: (1) patients receiving antibiotics for a duration of up to one week, (2) patients receiving antibiotics for a duration of up to two weeks, (3) patients receiving antibiotics for a duration of up to three weeks, (4) patients receiving antibiotics for a duration longer than three weeks (and up to a maximum of 42 days).
We examined the microbiological data of bacteria cultured from the wound and bone in comparison to bacteria later present in blood cultures (throughout the hospitalization stay), to determine the rate of specific organisms involved in DSWI or SOM to later crossover to involve the blood and also to define how many of the positive blood cultures were first found in DSWI cultures. Every bacteria cultured (from the blood or the surgical wound) was calculated once (n=1), even if it was cultured multiple times and on several occasions.
Results
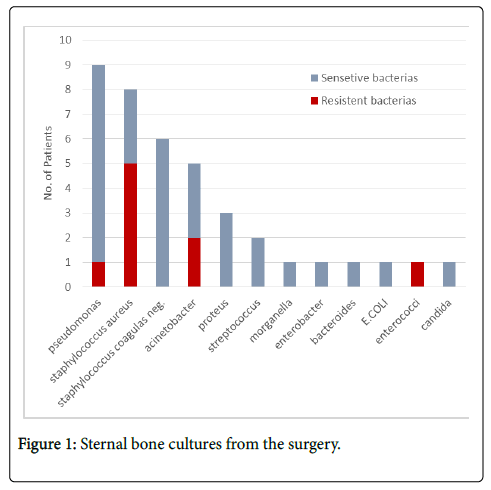
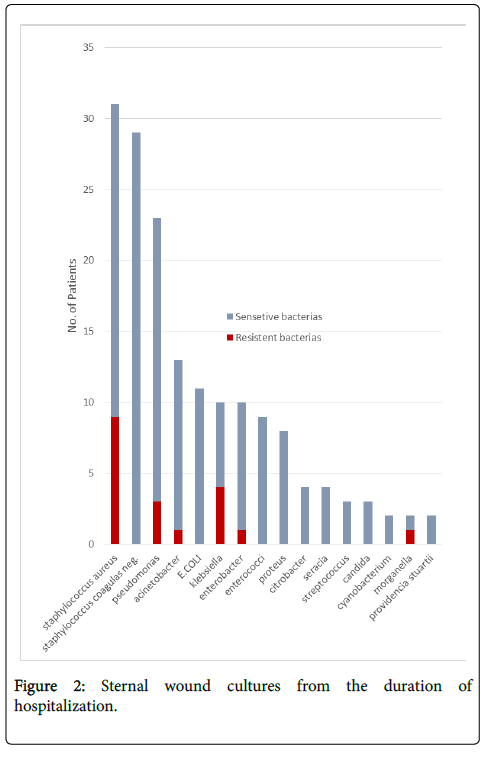
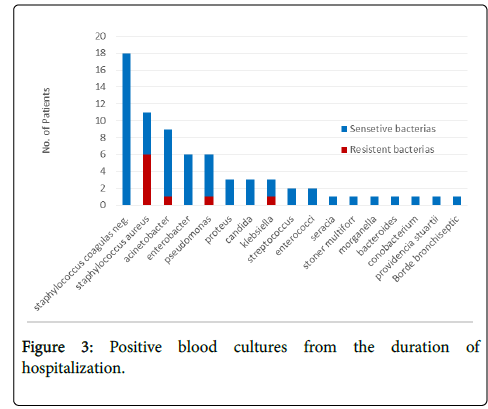
Seventy six patients with DSWI or SOM following sternotomy were found. Over half the patients were male (61%), with an average age of 68 years (44-88 years). 60% suffered from high blood pressure, 50% from ischemic heart disease, 35% from diabetes, 30% had emergent surgery for acute myocardial ischemia (MI), 25% were smokers and 6% required re-operation. CABG was most prevalent among our patients (79%), in comparison with mitral\aortic valve replacement (17% and 8% respectfully). All patients underwent surgical debridement and reconstruction with a pectoralis major advancement muscle flap and received broad-spectrum antibiotic treatment started at the time of diagnosis, preoperative and postoperative according to the patient’s condition. Reconstruction was predominantly performed using the left pectoralis major muscle advancement flap (71% compared to 19% using he right and 10% using bilateral pectoralis major muscle advancement flaps). Sternal bone cultures were sent during surgery, of which 39 (52%) where found to be positive for the following bacteria Pseudomonas, Staphlococcus aurreus, Staphlococcus coagulas negative, Acinetobacter, Proteus, Streptococcus, Morganella, Enterobacter, Bacteroides, Escherichia coli, Enterococci, Candida (Figure 1). Of which, resistant bacteria were found in 23% including - Pseudomonas, Staphlococcus aureus, Acinetobacter, Enterococci (Figure 1). Positive sternal wound cultures (from the duration of hospitalization) were found among 58 patients, with a total of 164 bacteria cultured - Staphlococcus aurreus, Staphlococcus coagulas negative, Pseudomonas, Acinetobacter, Escherichia coli, Klebsiella, Enterobacter, Enterococci, Proteus, Citrobacter, Seracia, Streptococcus, Candida, Cyanobacterium, Morganella, Providencia stuartii (Figure 2). With 11% of the cultured bacteria being resistant - Staphlococcus aurreus, Pseudomonas, Acinetobacter, Klebsiella, Enterobacter, Morganella (Figure 2). Positive blood cultures were found among 36 patients from a total of 70 bacterial cultures including - Staphlococcus coagulas negative, Staphlococcus aureus, Acinetobacter, Enterobacter, Pseudomonas, Proteus, Candida, Klebsiella, Streptococcus, Enterococci, Seracia, Stoner multiforr, Morganella, Bacteroides, Conobacterium, Providencia stuartii, Borde bronchiseptic. With 12% resistant bacteria-Staphlococcus aureus, Acinetobacter, Pseudomonas, Klebsiella (Figure 3). We compared the organisms isolated from the blood with those isolated from the wound and found that 37% of the bacteria from blood cultures were first detected in the sternal wound. From a different prespective, 16% of the organisms cultured from the wound were later found to spread into the bloodstream. When we compared the organisms isolated from the blood with those isolated from the bone and found that 14% of blood cultures were first detected in the bone culture and 26% of the organisms isolated from the bone were later found to spread into the bloodstream. The patients were divided into four groups based on the duration of antibiotic therapy following surgery. Half the patients (50%) had antibiotic therapy for less than a week. Seventeen percent had antibiotic therapy for a period of up to two weeks, 21% for a period of up to three weeks and 13% had antibiotic treatment for more than three weeks (to a maximum duration of 42 days) (Figure 4a and 4b). The majority (67% of the patients) received antibiotic treatment for a period of less than two weeks. 86% of the patients that were discharged from the hospital had completely closed sternal wound or a mild dehiscence of the surgical wound upon discharge. With only, 14% complicated with a fistula requiring re-hospitalization for antibiotic treatment or surgical debridement. Ten patients died during hospitalization (13%), two from DSWI complications (sepsis and hemothorax) and eight from other causes (e.g. aspiration pneumonia, respiratory failure and renal failure). Long term follow-up (with a median of 9 months, and up to 3 years and 2 months maximum duration) was favored in most cases.
Discussion
This study, in line with other publications, demonstrates that Staphylococcus is the most commonly cultured organism from deep sternal wound infection (bone cultures alongside wound cultures). The most commonly cultured Gram-negative organism was Pseudomonas and all Gram-negative organisms combined together represented approximately 50% of all cultures. Therefore, the empiric antibiotic treatment of choice should be broad spectrum covering both Gram positive and negative bacteria. Since MRSA was found amongst 20% of the Staphylococcus aureus infections, a combination of vancomicin along with an antibiotic that is active against a range of Gram-negative organisms (Quinolone, aminoglycosides, carbapenems or cephalosporins with anti-pseudomonal activity) should be initiated, later to be modified based on the sensitivity of the cultured bacteria. It is noteworthy, that only 10% of Gram-negative bacteria were found to be resistant to Carbapenem. Recent studies have shown that first line empiric treatment of sternal wound infections is Vancomicin [10,13]. This was based on the high prevalence of gram positive bacteria isolated from deep sternal wound infection tissue specimens. As for gram negative bacteria, despite their low prevalence in these publications, some recommend additionally adding Penicillin (of the B lactamase family), in lieu of their virulent nature [10,13]. Other studies advocate for a less aggressive line of treatment, a prophylactic regimen of Cefazoline alone or in conjunction with Gentamicin/Amikacin, starting sixty minutes prior to the surgical incision to be continued for no longer than 48 h. These studies suggest that vancomycin be reserved mainly for patients with a history of type I allergic reaction (anaphylaxis, urticaria, angioedema, or bronchospasm) to B-lactam agents or when MRSA is of special concern [13,14]. Additional publications demonstrate that the empirical regimen should include agents active against a range of Gram-negative organisms (aminoglycosides, carbapenems or cephalosporins with antipseudomonal activity), an agent active against methicillin-resistant Gram-positive organisms (vancomycin), and metronidazole [2,13-18]. These studies also conclude that the duration of antibiotic treatment should be based upon wound culture results and by clinical picture dynamics. This study demonstrates that in most DSWI or SOM cases (67%), an antibiotic regimen of two weeks following thorough debridement and reconstruction with a muscle flap is sufficient unless severe clinical evidence suggest otherwise.
Recent publications demonstrate that there is a 15-35% treatment failure with a reported mortality rate of 6-20% (with one report reaching up to 47%) during the first year after deep sternal wound infection diagnosis [19-21].
At the conclusion of our study we were able to achieve wound closure or only mild dehisces among 87% of our patients and demonstrated a 13% mortality rate.
Several studies attempted to assess the utility of sternal swab cultures alongside the value of blood cultures in the diagnosis and treatment of SWI. It was revealed that swab and tissue cultures were positive in 82% of patients [22,23]. Superficial swab cultures were predictive of the pathogen in 75% of the cases. Specifically, to Staphylococcus aureus, the positive predictive value of a superficial sternal swab was found to approach 100%. The inclusion of blood cultures predicted the pathogen 82% of the time. It was established that superficial swabs and blood cultures appear to be useful in determining the microbiological etiology of DSWI. Routing testing and reporting of these samples could enable early and targeted antimicrobial therapy in DSWI [24].
Studies focusing on the association between bacteremia’s and sternal wound complications in patients following sternotomies, illustrated a 3.2% incidence of bacteremia among these patients. It was established that the sternal wound was the most common source of bacteremia, accounting for 59% of the infections, with Coagulase-negative Staphylococcus responsible for one half of SWI. It was also stated, that often a positive blood culture was the first manifestation of wound infection, occurring before local signs were manifest, and recommended multiple blood cultures in sternotomy patients [25].
According to our findings, when sepsis is suspected antibiotic regimen may partially rely on preliminary wound or bone cultures, since we demonstrated that 37% of blood cultures were identical to prior wound cultures and 14% of blood cultures were identical to prior bone cultures. Additionally, 16% of the organisms isolated from the wound and 26% of the organisms isolated from the bone were shown to later cross over to the blood. No association was found between resistant bacteria and the higher chance for a bacterial crossover from the wound or bone to the blood. However, we only found a small number of resistant pathogens. Other limitation of this study is its retrospective nature and the relatively small number of patients.
Conclusion
This study demonstrates that the most commonly cultured organism from DSWI was found to be Staphylococcus and that all gram negative organisms combined together represent 50% of all cultures. We therefore conclude that a preliminary broad spectrum antibiotic treatment should be directed against gram positive as well as gram negative organisms. We recommend a combination of Vancomicin and an antibiotic that is active against a range of Gram-negative organisms (Quinolone, aminoglycosides, carbapenems or cephalosporins with anti-pseudomonal activity), later to be modified based on the sensitivity of the cultured bacteria. A thorough surgical revision with debridement of all foreign bodies, and reconstruction with vascularized soft tissue flap (such as a pectoral major advancement flap) is crucial to the success of DSWI treatment, followed by antibiotic treatment for a relatively short period of two weeks is adequate unless severe clinical evidence suggest otherwise. Our analysis demonstrates that wound and bone cultures provide important information not only for choosing the antibiotic therapy for perioperative treatment, but also when sepsis is suspected. This assumption was made as 37% of blood cultures were found to be identical to prior wound cultures and 14% to prior bone cultures. Also 16% of the organisms isolated from the wound and 26% of the organisms isolated from the bone were later found to involve the blood.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Alicia J. Mangram, Teresa C. Horan, Michele L. Pearson, Leah C. Silver, William R. Jarvis (1999) Guidelines for prevention of surgical site infection. Infection Control Hospital Epidem 20: 247-278.
- El Oakley RM, Wright JE (1996) Postoperative mediastinitis: classification and management. Ann Thorac Surg 61: 1030-1036.
- Berdajs DA, Trampuz A, Ferrari E, Ruchat P, Hurni M, et al. (2011) Delayed primary versus late secondary wound closure in the treatment of postsurgical sternum osteomyelitis. Interact Cardiovasc Thorac Surg 12: 914-918.
- Softah A, Bedard A, Hendry P, Masters RG, Goldstein W, et al. (2002) Wound infection in cardiac surgery. Annals Saudi Med 22: 105-107.
- Marisa De Feo, Mariano Vicchio, Pasquale Santè, Flavio Cerasuolo, Gianantonio Nappi (2012) Evolution in the treatment of mediastinitis: single-center experience. Asian Cardiovasc Thorac Ann 19: 39-43.
- Filsoufi F, Castillo JG, Rahmanian PB, Broumand SR, Silvay G, et al. (2009) Epidemiology of deep sternal wound infection in cardiac surgery. J Cardiothorac Vasc Anesth 23: 488-494.
- Johan Sjogren, Malin Malmsjo, Ronny Gustafsson, Richard Ingemansson (2006) Poststernotomy mediastinitis: a review of conventional surgical treatments, vacuum-assisted closure therapy and presentation of the Lund University Hospital mediastinitis algorithm. Eur J Cardiothorac Surg 30: 898-905.
- RJ Baskett, CE MacDougall, DB Ross (1999) Is mediastinitis a preventable complication? A 10-year review. Ann Thorac Surg 67: 462-465.
- Kuan-Ming Chiu, Tzu-Yu Lin, Shu-Hsun Chu, Cheng-Wei Lu (2014) Managing Sternal Osteomyelitis with Antibiotic Bead Implantation. Asian Cardiovasc Thorac Ann 14: e41-e42.
- Bettina Khanlari, Luigia Elzi, Laura Estermann, Maja Weisser, Wolfgang Brett, et al. (2010) A rifampicin-containing antibiotic treatment improves outcome of staphylococcal deep sternal wound infections. J Antimicrob Chemother 65: 1799-1806.
- Alex Chaudhuria, Kiran Shekarb, Chris Coulter (2014) Post-operative deep sternal wound infections: making an early microbiological diagnosis. Eur J Cardiothorac Surg 41: 1304-1308.
- Vaska P (1993) Sternal Wound Infections. Advanced Critical Care 4: 475-483.
- Molina JE, Nelson EC, Smith RR (2006) Treatment of postoperative sternal dehiscence with mediastinitis: twenty-four year use of a single method. J Thoracic Cardio-Vascular Sur 132: 782-787.
- Abbas S. Omran, Abbasali Karimi, S. Hossein Ahmadi, Setareh Davoodi, Mehrab Marzban, et al. (2007) Superficial and deep sternal wound infection after more than 9000 coronary artery bypass graft (CABG): incidence, risk factors and mortality. BMC Infect Dis 7: 112.
- Aron F. Popov, Jan D. Schmitto, Ahmad F. Jebran, Christian Bireta, Martin Friedrich, et al. (2011) Treatment of gram-positive deep sternal wound infections in cardiac surgery -experiences with daptomycin. J Cardiothoracic Sur 6: 112.
- Gilbert H.L Tang, Manjula Maganti, Richard D. Weisel, Michael A. Borger (2004) Prevention and management of deep sternal wound infection. Semin Thorac Cardiovasc Surg 16: 62-69.
- Walter H. Merrill, Shahab A. Akhter, Randall K. Wolf, William E. Schneeberger, John B. Flege (2004) Simplified Treatment of Postoperative Mediastinitis. Ann Thorac Surg 78: 608-612.
- Günter Marggraf, Fred H. Splittgerber, Michael Knox, Jürgen Christoph (1999) Mediastinitis after cardiac surgery-epidemiology and current treatment. Eur J Surg Suppl 584: 12-16.
- Jones G, Jurkiewicz MJ, Bostwick J, Wood R, Bried JT, et al. (1197) Management of the Infected Median Sternotomy Wound with Muscle Flaps The Emory 20-Year Experience. Ann Surg 225: 766-776.
- Michael A. Borger, Vivek Rao, Richard D. Weisel, Joan Ivanov, Gideon Cohen, (1998) Deep Sternal Wound Infection: Risk Factors and Outcomes. Ann Thorac Surg 65: 1050-1056.
- Immer FF, Durrer M, Mühlemann KS, Erni D, Gahl B, et al. (2005) Deep sternal wound infection after cardiac surgery: modality of treatment and outcome. Ann Thorac Surg 80: 957-961.
- Luckraz H, Murphy F, Bryant S, Charman C. Susan, Ritchie J (2003) Vacuum-assisted closure as a treatment modality for infections after cardiac surgery. J Thorac Cardiovasc Surg 125: 301-305.
- Okonta KE, Anbarasu M, Agarwal V, Jamesraj J, Kurian VM, et al. (2011) Sternal wound infection following open heart surgery: appraisal of infection, risk factors, changing bacteriologic pattern and treatment outcome. J Thorac Cardiovasc Surg 27: 28-32.
- Chaudhuri A, Shekar K, Coulter C (2012) Post-operative deep sternal wound infections: making an early microbiological diagnosis. Eur J Cardiothorac Surg 41: 1304-1308.
- Kohman LJ, Coleman MJ, Parker FB (1990) Bacteremia and sternal infection after coronary artery bypass grafting. Ann Thorac Surg 49: 454-457.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 3659
- [From(publication date):
August-2017 - Jul 05, 2025] - Breakdown by view type
- HTML page views : 2788
- PDF downloads : 871