Review Article on Antimicrobial Resistance Worldwide
Received: 22-Dec-2023 / Manuscript No. jcidp-23-120851 / Editor assigned: 25-Dec-2023 / PreQC No. jcidp-23-120851(PQ) / Reviewed: 08-Jan-2024 / QC No. jcidp-23-120851 / Revised: 12-Jan-2024 / Manuscript No. jcidp-23-120851(R) / Published Date: 19-Jan-2024
Abstract
Antimicrobial is a substance includes antibiotic, anti-fungal, anti-parasite, anti-viruses, that use for the prevention, treatment, of diseases, history of antimicrobial by Egyptians scientist and classification of antimicrobial in a tabular form and some pathological condition related to antimicrobial resistance e.g tuberculosis, urinary tract infection, Typhoid, some key point regarding antimicrobial resistance, and Image related all antimicrobial resistance showed and some mechanism causes of resistance antimicrobial agent, definition of antimicrobial resistance, is an occur when bacteria, fungi, viruses, parasite, change over period and longer response spread, severe illness and death, and factors that influences all anti-microbial resistance and world health organization response regarding antimicrobial resistance, that aims to guide policy makers researchers funder to implementing partners industry, civil society in generating new evidence to inform antimicrobial resistance, and take some review data analysis and graphical showed from region word areas percentage of mortality rate by 2050 AMR, and how to control antimicrobial resistance, by environmental hygiene control and follow medical professional instruction before taken antibiotics, due to avoided risk of resistance of antimicrobial. Also conclusion properly environmental sanitation, using antibiotic by medical professional prescribed, make sure keep diagnosis before start given antibiotics, if reduce the risk factors of resistance antimicrobial agent.
Introduction
Antimicrobial-including antibiotics, antivirals, anti-fungal and anti-parasitic-all are medicines used to prevent and treat infections in humans, animals and plants infection, Despite proposal initiatives in recent decades, the world has failed to keep with microbes becoming increasingly resistant it’s so called Antimicrobial Resistance (AMR) any antibiotic use contributes to have no effect. AMR is thus an unavoidable phenomenon undermine the effectiveness of basic and modern medicine and is effecting people from birth to death [1-10].
Antibacterial Strategic based on metal uptake the rise antibiotic resistance require new strategic to development novel antimicrobial give that bacteria require metal uptake for their survival and proliferation drug that target these uptake path way are a promising approach this section explores how specific metal uptake path way bacteria can used and provides examples of antibiotics that use this strategy.
Also Antimicrobial Resistance (AMR) poses a serious global threat of growing concern to human, animal and environmental health this due to the emergency spread and persistence of multi drug resistance (AMR) bacteria or super bugs MDR bacteria exist across the animal, human an environmental triangle or niche and there is interlinked sharing of these pathogens in this triad.
History
Antimicrobial was practice use almost 2000 years, ancient Egyptians and ancient Greeks used specific molds and plant extracts for treat infection.
In 19th era, microbiologist such as Louis Pasteur and Jules Francois Joubert analyzed antagonism between some bacteria and discussed the merits of controlling this interaction in medicine [11-20].
The Alexander Fleming on September 3, 1928 was isolated staphylococcus separated in to colonies do to the antimicrobial fungus penicillium rubens.
Classification of antimicrobial
• Antibacterial
• Antivirus
• Antifungal
• Anti-parasite
Disinfectants: is an agent used destroyed microorganism in nonliving surfaces. e.g chlorine, calcium, phenol, quatensry ammonium compound etc.
Antiseptic: is also applying by living surfaces or during surgery to reduce the infection. e.g Hydrogen peroxide, isopropyl alcohol, chlorhexidine etc.
What is anti-bacteria?
Is an agent that used for the kill or inhibits the growth of bacteria.
Spectrum activities
• Narrow spectrum
• Broad spectrum
Mode of action
• Bacteriacidal
• Bacteriastatic (Table 1)
| S/n | Classification of Antibiotics | Mode of Action | Mechanism of Action |
|---|---|---|---|
| 1 | Bete lactam: e.g penicillin, cephalosporin. | Bacteriacidal | Bacteria cell wall inhibit |
| 2 | Microlide: e.g Azithromycin,erythromycin | Bacteriastatic | Inhibit Bacteria protein synthesis |
| 3 | Aminoglycoside: e.g Amikacin, Streptomycin | Bacteriacidal | Inhibit Bacteria protein synthesis |
| 4 | Tetracycline: e.g Doxycycline,minocycline | Bacteriastatic | Inhibit Bacteria protein synthesis |
| 5 | Fluroquenolones: e.g Ciprofloxacin, levofloxacin | Bacteriacidal | Target of Bacteria DNA |
| 6 | Sulfanamide: e.g Sulfadiazine,sulfadoxine | Bcteriastatic | Inhibit folic Acid Synthesis |
Table 1: Classification of antibiotics and their uses.
Factors influence antibiotic resistance
• Ovar prescribtion of antibiotic.
• Pateint not finish their treatment
• Over using antibiotic in livestock and fish farming.
• Lack of sanitation and poor hygiene.
• What is Poor infection control in clinical and hospital.
Antivirus
Is a substance that can be used for the treating of viruses. e.g. Acyclovir, cidofovir, foscarnet, penciclovir, ganciclovir, brivudin etc (Table 2).
| S/N | Classification of Antivirus | Enzymes/Mechanism | Targets/Strategies |
|---|---|---|---|
| 1 | Anti-herpes virus: e.g Acyclovir, vidarabine | polymerase | Viral enzymes |
| 2 | Anti-Influenza virus: e.g zanamivir,Amantadine | Neuraminidase | Virus enzymes |
| 3 | Anti-hepatitis virus: nonselective drugs e.g adefovir dipivoxil, Ribavir | Capping enzymes, immune response | Cellular target |
| 4 | Drug for papilloma: virus e.g imiquimod | Banding to viral glycoprotein | Immuno precipitation |
Table 2: Classification of Antivirus.
What is Anti-fungal?
Is a substance that against fungal infection, like skin. Triazole Anti-fungal: fluconazole, itraconazole, terconazole, Voriconazole etc. e.g. like-Imidazole anti-fungal: ketaconazole miconozolesulconozole, bifonazole, lanaconazole etc (Table 3).
| S/N | Classification Antifungal | Mode of Acton | Mechanism of Action |
|---|---|---|---|
| 1 | Antibiotics e.g Amphotericin B, Griseofulvin | Banding to ergosterol fungicidal | Disruption of spindle and cytoplasmic microtubule fuction. |
| 2 | Antimetabolites e.g flucytosine (5-FC) |
Inhibit of RNA/DNA protein synthesis | Inhibit fungal protein synthesis by replacing uracil with fluro uracil in fungal RNA. |
| 3 | Azoles e.g Imidazole: clitrimazole, miconozole & Triazole: fluconozole, voriconozole | Inhibit of lanosterol 14 alpha –demethyiase fungistatic | Inhibit of cytochrome P450. |
| 4 | Allylamine :terbinafine | Inhibiting ergosterol synthesis. fungicidal | Inhibit ergo sterol synthesis by inhibiting the enzymes squalene exp expoxidase |
| 5 | Other topical agent e.g Benzoic Acid, Undercylenic acid | Miscellaneous, varied |
Table 3: Classification of Antifungal.
What is Anti parasite?
Is a group of substance they can be used for the treatment of diseases coursed by parasite, including protozoa, helminthic. Anti- Helminthic: Albendazole, mebendazole, metronidazole, tinidazole,etc. Anti-Protozoa: quinine, pyramethamine, artemisinin, primaquine etc. can’t cost on national and global economies (Table 4).
| S/N | Classification of Anti Parasite | Mode of Action | Mechanism of Action |
|---|---|---|---|
| 1 | Anti-protozoa:e.g metronidazole, Tinidazole, | Destroy protozoa Inhibit the growth and ability to reproduce | Inhibit protozoa folic acid synthesis. |
| 2 | Anti-malaria: e.g Quinine, artemisinin, |
Inhibit the action heme polymerase. | Interfering with the digestive of haemoglobin in the blood stage of the malaria life cycle, |
| 3 | Anti-helmentic: e.g Albendazole, mebendazole, | Inhibit ion of polymerization of beta- botulin into micro tubule followed by inhibition of glucose uptake and transport. | Block micro tubule functions of parasites and mammalian cells. |
| 4 | Anti-amobiosis: e.g Chloroquine, tinidazole, metronidazole | Intermediate metabolized compound are formed and bind DNA and inhibit protein synthesis, coursing cell death | Diffuses in to the organism, inhibit protein synthesis by interacting with DNA, and cause a loss of helical DNA structure and strand breakage. |
Table 4: Classification of Anti-Parasite.
Pathological condition related to antibiotics
• Typhoid
• Tuberculosis (TB)
• Urinary Tract Infection (UTI)
Typhoid
Typhoid is an infection that spread through contaminated food and water, cousin by salmonella typhi that change the physiological function of the body.
Symptoms: High fever, headache, abdominal pain, weakness, vomiting, loose of stools.
Treatment: Ciprofloxacin, amaoxicilin, ceftrioxone, cholorophenicol, cotrimaxazole. These are resistance for the typhoid fever, occur if the bacteria change in repose to use of these medicine.
TB
Tuberculosis serious condition course by mycobacterium, primary attack lungs that change the physiological function of the body (Figure 1).
Symptoms: Fatigue, fever, loose of appetite, weigh loose, dry cough with blood, shortness of breath, swollen lymph nodes.
Types of TB: pulmunary Tb, skeletal Tb, Brain Tb, GIT Tb, miliary Tb,
Treatment of Tb
First line drugs: Rafampin, isoniazid, ethambutol, pyranamide, streptomycin etc.
Second line drugs: levofloxacin, moxifloxacinamikacin, bedaquiline, cycloserine, kanamycin etc.
UTI
Urinary Tract Infection is a serious infection course by E. coli bacteria usually attack upper and lower urinary track. Upper urinary track: kidney & Lower urinary track: bladder.
Symptoms: Pelvic pain, increased urge to urinate, pain with urination and blood in urine, Kidney infection, Back pain, nausea, vomiting, fever.
Treatment of UTI: Fluroquenolones, penicilin, cotrimaxazole, tetracycline, cephalosprin, amoxicillin etc.
Antimicrobial resistance (AMR)
Is an occur when bacteria, fungi, viruses, parasites, change over period and longer response to the medicines making infections harder to treat and increasing the risk of diseases spread, severe illness and death.
Keypoint
• Resistance (AMR) is world health and development threat.
• WHO was declared (AMR) is part of top 10 world public health
• Lack of clean water and proper sanitation
• Without effective antimicrobial the success of modern medicine in treating diseases, including major surgery and cancer chemotherapy, would be at increased risk.
Why antimicrobial resistance?
Antimicrobial mostly resistance naturally, genetically occur, and lack of proper used antimicrobial especially antibiotic, over used one class of antibiotic, escaped dose, environmental and sanitation hazard.
Antibacterial resistance such as antibiotics
Example anti TB drugs Rafampin. Is an anti TB drug broad spectrum used combine drugs treatment due to avoided resistance e.g. isoniazid, ethambutol, pyrazinamide. Was discovered in 1965, marketed in Italy in 1968 and approved in United State in 1971.
Mechanism of action: Rafampin usually inhibit bacterial DNA and dependent RNA polymerase.
Resistance Rafampin is a broad subject not the mechanism of clinical resistance, nearly always due to genetic change in the β sub unit bacteria RNA Polymerase. In particular mycobacterium Tb interestingly, change in the same codons of the consensus.
Side effect: hepatotoxicity, inching, flushing, drowsiness, headache,difficulty concentration etc (Figure 2).
Note: Before given Rafampin should being test the liver function and amount of blood in the body.
Antivirus Resistance
Is a substance used for the treatment of viruses that courses infection and illness such as: influenza, genital herpes, immunodeficiency virus (HIV), Anti viruses working, a viruses courses infection by entering host cell and making copies of itself (replicating). Antivirus drugs block the viruses ability to replicate.
Courses resistance antivirus
The less amount viruses but is always there, if you miss prescribed doses of an antiviral or stop treatment too son the virus may multiplying again As may replicates the virus genetic make-up mutate change. Sometime viruses responding for previously antivirals effective for no known reason called spontaneous resistance (Figure 3).
Note: People who take antiviral for long time treatment chronic viral infection like HIV, Genital herpes, hepatitis B or hepatitis C are more risk for virus resistance. Also people have compromised immune system due to autoimmune diseases, organ transplant, cancer treatment chemotherapy more risk of antiviral resistance
Antifungal resistance
Agent: It help body to get rid certain fungal infection; they treat fungal like skin yeast infection, athletes foot, itch, and ring worm.
Why Anti-fungal resistance?
Improper used anti-fungal drugs: e.g. skip doses, stop treatment when you get partial relief, or receive doses low, that fungus may get chance fighting off the medicines effects.
Natural resistance: never respond to anti-fungal.
Spontaneous resistance: fungus stops responding to once effective drugs for no known reason.
Transmitted resistance: if spreads contagious drugs resistance fungal infection to someone else, that person now has not respond anti-fungal, even they have never used the medicine (Figure 4).
Why anti-fungal resistance is serious global issues?
Because it has greatly limit treatment option, if the anti-fungal does not respond to one of the three classes of anti-fungal drugs, the other option may be less effective, some medication course more severe potentially toxic side effect.
Who is risk to development anti-fungal resistance?
People leimmuneak system, AIDS, cancer, organ transplant, stem cell (bone marrow) transplant.
Anti-parasites resistance
Resistance is genetic ability to survive treatment with an antiparasite medication it was generally effect against those parasite in the past, after an Animal is treated with an anti-parasite drugs, the susceptible parasite die and the resistance paradise survive to pass on resistance genes to their offspring (parasite are often called worm and anti-parasite drug are often called dewormers).
Factors contribute to Resistance anti parasite
• The biology of the parasite.
• Strength of the infected.
• The practices used to treat parasite.
• Properties of the particular anti-parasite used for treatment at any moment.
• Certain livestock management practices.
Note: Science shows that anti-parasite resistance however, this naturally resistance may be showed down.
Resistance anti-malaria drug:
The emergency drug resistance parasite poses one of the greatest threats to malaria control and result in increased malaria morbidity and mortality. Artemesinin based combination therapies (ACTS) are recommended first line treatment for uncomplicated P. falciparrum malaria and are by must malaria endemic countries.
Therefore multiple drug resistance malaria recommended for use are e.g. Mefloqueine, halofantrine and quinine with tetracycline, and also artesunate, atovaquone and proguanil is highly effective well tolerated treatment (Figure 5).
Mosquito parasite
WHO about antimicrobial resistance world health organization agenda for antimicrobial resistance in human health prioritizes almost 40 research topic for evidence generation inform policy by 20230. It aims to guide policy makers researchers founders, to implementing partners industry civil society in generating new evidence to inform antimicrobial resistance policies and intervention as part of efforts to address antimicrobial resistance in the human health, especially infection cause by WHO bacteria pathogen and WHO fungal pathogen with critical importance for antimicrobial resistance such as candida auris and Drug resistance treatment of mycobacterium tuberculosis.
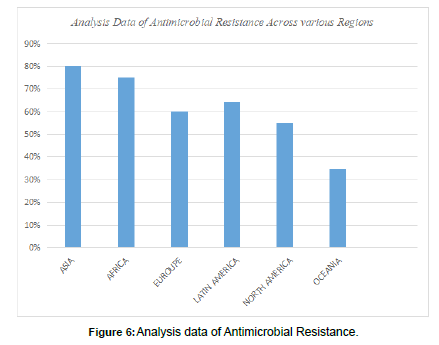
Data analysis for antimicrobial resistance
Different regions area percentage of antimicrobial resistance mortality rate by 2050. By used region area of the worldwide and taken the percentage of the resistance of antimicrobial at the difference region areas worldwide that is in mortality rate by 2050, the region areas of the worldwide are below (Table 5):
S/N |
Region areas of AMR | Amount of resistance | % of resistance |
|---|---|---|---|
| 1 | ASIA | 4,330,00 | 80% |
| 2 | AFRICA | 4,150,00 | 75% |
| 3 | EUROPE | 390,000 | 60% |
| 4 | LATIN AMERICAN | 392,000 | 64% |
| 5 | NORTH AMERICAN | 317,000 | 55% |
| 6 | OCEANIA | 22,000 | 35% |
Table 5: Table of mortality rate by 2050 AMR Region areas.
• Asia
• Africa
• Europe
• Latin American
• North American
• Ocenia
All these are part of the region that antimicrobial resistance, but any regions have different antimicrobial that highly resistance in their areas.
e.g Asia: Asia have issues of streptococcus pneumoniae have be found in Asia country, particularly erythromycin resistance increases dramatically many in Asian countries 75%.
African: African have issues of Ampicillin 84.5% and cotrimaxazole 68.5% among the Gram negative bacilli (30) Gram positive cocci show resistance to Nalidixic acid (81%) and with E. coli showing high as 84% resistance to ampicillin and 68% to Cotrimoxazole.
Europe: Escherichia coli resistance to major antibiotic is increases in almost all countries in Europe.
Latin American: Latin American has issues resistance of carbapenem resistance according to the surveillance data from Latin American.
North American: by data pointed out that have issues of fluoroqueinolone resistance of E.coli has be reported in 92 member state out of 194 and 5 out of 6 WHO global regions.
Oceania: according to the 2014 surveillance reported based on 2011/12 data,resistance of K pneumoniae isolated third generation cephalosporin in Kiribati was 1%,only one reported of carbapenem resistance was identified and in o.7% isolated from hospital, also salmonella spp studied about typhoidal salmonella was from eastern Highland province 58%(22/38) of isolates were resistant to chloramphenicol, 37% (14/38) to kanamycin, 53% (20/38) ampicillin (Figure 6).
Control of AMR
• Use of antibiotic by a certified health professional.
• Never demand antibiotic if your health workers say you do not need them.
• Always follow your health workers advice when using antibiotics.
• Environmental hygiene.
Prevention of Antimicrobial Resistance (AMR)
• Screening for diagnosis.
• Antibiotic prescribed by the patient required.
• Follow antibiotic guideline.
• Infection control e.g antiseptic, hand hygiene, use personal protective equipment and cleaning equipment room. • Antibiotic come under schedule H so avoid use as OTC medicine.
Conclusion
Make sure to control environmental sanitation and follow instruction of medical professional during prescription, also don taken any antibiotics without diagnosis that is proper investigation of actually pathological Diseases in the patient body, and avoid safe medication.
References
- Smith A, M’ikanatha NM, Read AF (2015)Antibiotic resistance: a primer and call to action.Health Commun 30: 1–27.
- Caron WP, Mousa SA (2010)Prevention strategies for antimicrobial resistance: a systematic review of the literature.Infect Drug Resist 3: 25–33.
- Ricciardi W, Giubbini G, Laurenti P (2016)Surveillance and control of antibiotic resistance in the Mediterranean region.Mediterr J Hematol Infect Dis 8: 2016036.
- Asokan GV, Asokan V (2016)Bradford Hill’s criteria, emerging zoo noses, and one health.J Epidemiol Glob Health 6: 125–129.
- Van Puyvelde S, Deborggraeve S, Jacobs J (2018)Why the antibiotic resistance crisis requires a one health approach.Lancet Infect Dis 18: 132–133.
- National Academies of Sciences, Engineering, and Medicine (2017)Combating antimicrobial resistance: a one health approach to a global threat: proceedings of a workshop. Washington, DC: The National Academies Press.
- Harbarth S, Balkhy HH, Goosens H, Jarlier V, Kluytmans J, et al.(2015) Antimicrobial resistance: one world, one fight!Antimicrob Resist Infect Control 4.
- Robinson TP, Bu DP, Carrique-Mas J, Fèvre EM, Gilbert M, et al. (2016) Antibiotic resistance is the quintessential one health issue.Trans R Soc Trop Med Hyg 110: 377–380.
- Kmietowicz Z (2019)NHS will test “pay for usefulness” model to stimulate research.BMJ 366: l4610.
- O’Neill J (2016)Tackling drug-resistant infections globally: final report and recommendations.The review on antimicrobial resistance. Wellcome Trust. HM Government.
- Bassetti M, Poulakou G, Ruppe E, Bouza E, Van Hal SJ, et al.(2017) Antimicrobial resistance in the next 30 years, humankind, bugs and drugs: a visionary approach.Intensive Care Med 43: 1464–1475.
- World Bank (2017)Drug-resistant infections: a threat to our economic future. Washington, DC: World Bank. License: Creative Commons Attribution CC BY 3.0 IGO, 2017.
- Smith R, Coast J (2013)The true cost of antimicrobial resistance.BMJ 346.
- Leal J, Conly J, Henderson EA, Manns BJ (2017) How externalities impact an evaluation of strategies to prevent antimicrobial resistance in health care organizations.Antimicrob Resist Infect Control 6: 53.
- Daulaire N, Bang A, Tomson G, Kalyango JN, Cars O (2015) Universal access to effective antibiotics is essential for tackling antibiotic resistance.J Med Law Ethics 43: 17–21.
- Xie R, Zhang XD, Zhao Q, Peng B, Zheng J (2018) Analysis of global prevalence of antibiotic resistance in Acinetobacter baumannii infections disclosed a faster increase in OECD countries.Emerg Microbes Infect 7: 31.
- Magee JT, Heginbothom ML, Mason BW (2005)Finding a strategy: the case for co-operative research on resistance epidemiology.J Antimicrob Chemother 55: 628–633.
- Nadimpalli M, Delarocque-Astagneau E, Love DC, Price LB, Huynh BT, et al.(2018) Combating global antibiotic resistance: emerging one health concerns in lower- and middle-income countries.Clinl Infect Dis 66: 963–969.
- Richardson LA (2017)Understanding and overcoming antibiotic resistance.PLoS Biol 23: 2003775.
- Rather IA, Byung-Chun K, Bajpai VK, Park YH (2017) Self-medication and antibiotic resistance: crisis, current challenges, and prevention.Saudi J Biol Sci 24.
Indexed atGoogle Scholar Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Umar AI, Yadav R (2024) Review Article on Antimicrobial Resistance Worldwide. J Clin Infect Dis Pract 9: 227.
Copyright: © 2024 Umar AI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 1047
- [From(publication date): 0-2024 - Dec 01, 2025]
- Breakdown by view type
- HTML page views: 755
- PDF downloads: 292