Retrospective analysis of the epidemiology and clinical features of COVID-19 swab positive patients in relation to their imaging characteristics
Received: 10-Jan-2022 / Manuscript No. roa-22-51499 / Editor assigned: 12-Jan-2022 / PreQC No. roa-22-51499(PQ) / Reviewed: 26-Jan-2022 / QC No. roa22-51499 / Revised: 31-Jan-2022 / Manuscript No. roa-22-51499(R) / Published Date: 07-Feb-2022 DOI: 10.4172/2167-7964.1000363
Abstract
Introduction: This retrospective analysis identifies the common radiographic features of COVID-19 pneumonia, by describing the main chest x-ray and CT findings in a selected cohort of patients. The demographics and symptoms at presentation were also obtained to correlate with the national guidance and determine whether there is any statistically significant difference in imaging presentation between demographics.
Methods: Only patients presenting with a positive COVID-19 test who also underwent a chest x ray, CT chest or CT pulmonary angiography were eligible for this study. A total of 332 patients met the criteria, aged from 16 to 98.4 (mean age of 70.5 years) and compromising men and women.
Results: There was a significant difference in the number of abnormal chest X-rays (CXR) between males and females (p= 0.0086). Within these there were no individual symptoms showing significant differences between the sexes. Consolidation with bilateral, basal and peripheral predominance was all common features. Pleural effusion was seen in 4%.
Conclusion: This study corroborates imaging findings from earlier studies in the prevalence of radiographic/CT features. There was no significant difference in symptoms between males and females however there was a significant difference in the number of abnormal imaging between the groups.
Background
Coronavirus disease 2019 (COVID-19) is caused by SARS-CoV-2, a beta coronavirus closely linked to the SARS virus. The virus was first identified in the city of Wuhan, China, in December 2019 [1]. Transmission mainly occurs from contact with respiratory droplets, by direct contact with infected persons, or by contact with contaminated objects or surfaces [2]. The incubation period for COVID-19 (the time from initial exposure to symptom onset) is, on average, 5–6 days, but can be up to 14 days [1]. Most people with COVID-19 develop only mild (40%) or moderate (40%) disease with common symptoms including fever, dry cough, tiredness, loss of taste or smell, sore throat, aches and pains and diarrhoea [3]. However around 15% will develop severe disease that requires oxygen support, and 5% will develop critical disease with complications such as respiratory failure, acute respiratory distress syndrome (ARDS), sepsis and septic shock, thromboembolism, and/or multiorgan failure, including acute kidney injury and cardiac injury [4].
There have been several studies into the radiological manifestations of the disease. Chest radiographs have been shown to have limited sensitivity to COVID-19 (around 68.1%) [5]. Findings include patchy or diffuse reticulonodular opacities and consolidation, with basal, peripheral and bilateral predominance5. Computed Tomography (CT), has a much higher sensitivity (97–98%), but a very low specificity in detecting typical features [6-8]. Documented manifestations include bilateral, sub-pleural, ground-glass opacities with air bronchograms, ill-defined margins, and a slight predominance in the right lower lobe [9]. Abnormal lung CT findings can be present even in asymptomatic patients, and lesions can rapidly evolve into a diffuse ground-glass opacity predominance or consolidation pattern within 1–3 weeks after onset of symptoms, peaking at around 2 weeks after onset. Age and gender have previously been identified as potential risk factors and although this hasn’t been confirmed epidemiological studies have found an increase in attack rates amongst the elderly [10].
Despite British Society of Thoracic Imaging (BSTI) guidelines identifying features such as pleural effusion as being atypical for COVID-19, these have been found to be prevalent in as much as 26% of cases in the literature [11]. Moreover it is our experience that atypical appearances have been frequently identified on both chest radiograph and CT imaging in practice.
The aim of this study was to gain a better understanding of the common radiographic features of COVID-19 pneumonia, by describing the main chest X-ray and CT findings in a selected cohort of patients. By also examining the demographics (age and gender) and symptoms at presentation we also aimed to identify the most common symptoms, correlate with the national guidance and determine whether there is any statistically significant difference in imaging presentation between demographics.
Without an accurate understanding of the key radiological manifestations of the disease we cannot hope to achieve efficient diagnosis and isolation of the infected individuals. We hope that by comparing this with current BSTI guidelines for radiographic reporting of COVID-19 patients [11]. We can potentially identify whether any features currently classed as ‘atypical’ actually occur more frequently thus should not be used as exclusion criteria for the disease.
Methods
A retrospective study was performed during the first wave of COVID-19, between the months of March and May 2019. Eligibility criteria included those presenting with a positive COVID-19 test result that also underwent a chest x ray, CT chest or CT pulmonary angiography between 01/03/2020 to 31/05/2021. A total of 332 patients met the criteria, aged from 16 to 98.4 and compromising men and women (mean age of 70.5 years).
As part of the study, all included imaging studies, patients’ demographics and symptoms were examined by a consultant radiographer and 3 radiologists using electronic clinical software ‘Medi Tech and ‘Sepia’. The local PACS software was accessed to visualise the imaging reports and the radiographic features. Each reviewer was blind to the others’ review to prevent bias in interpretation. Results were recorded in tabular format using Excel software.
IRAS and local research and development department approval was obtained prior to commencement of this study. Any patient identifiable information was stored electronically and password protected.
Results
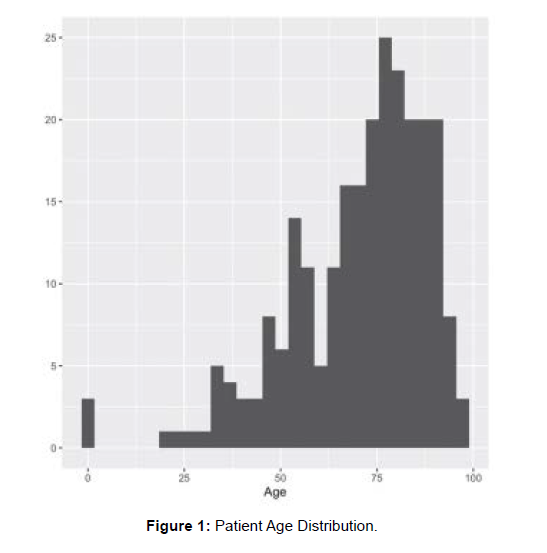
The data consisted of 332 patients, 154 (46%) were female and 178 (54%) were male. The majority (313) of patients were Caucasian (94%), Table 1 show the sex and ethnicity percentages. (Table 1 and Figure 1)
| Demographics (n=332) | ||||
|---|---|---|---|---|
| Female | Male | |||
| % Sex | 46 | 54 | ||
| Asian | Caucasian | N/A | Black | |
| % Ethnicity | 2 | 94 | 3 | 0 |
Table 1: Gender and ethnicity frequency.
Figure 1 shows the distribution of patient age. The range of patient ages was 0.1 to 98.4 years with a mean of 70.5 and a standard deviation of 18.22. Excluding patients with a recorded age under 16 years, the mean age was of 71.2 years (standard deviation 17.02).
Table 2 shows that 17% of patients had a normal chest X-ray (normal.CXR=Y). For those patients that had an abnormal chest X-ray the percentage of each abnormality is given. Similarly, the percentage of patients who had a normal CT scan (normal.CT=Y) are presented. For those patients that had an abnormal CT scan the percentage of abnormalities are given. (Table 2)
| Y | N | N/A | |
|---|---|---|---|
| % Normal CXR (n=332) | 17 | 80 | 2 |
| % Abnormal CXR (n=266) | |||
| % Reticulonodular (RN) Opacities | 2 | 98 | 0 |
| % Consolidation | 89 | 11 | 0 |
| % Basal | 77 | 22 | 0 |
| %Peripheral | 53 | 46 | 1 |
| % Bilateral | 76 | 24 | 0 |
| % Normal CT (n=332) | 1 | 15 | 84 |
| Abnormal CT scan: Classic Signs (n=50) | |||
| %Ground Glass Opacity (GGO) | 90 | 10 | 0 |
| %Crazy paving | 46 | 54 | 0 |
| % Air Bronchograms | 30 | 70 | 0 |
| % Subpleural | 86 | 14 | 0 |
| % Bilateral | 58 | 36 | 6 |
| Abnormal CT scan: Intermediate (n=50) | |||
| % Central | 30 | 64 | 6 |
| % Unilateral | 8 | 86 | 6 |
| % Lymphadenopathy | 14 | 80 | 6 |
| Abnormal CT scan: Atypical (n=50) | |||
| % Cavitation | 8 | 92 | 0 |
| % Calcification | 8 | 92 | 0 |
| % Pneumothorax | 8 | 92 | 0 |
| % Pleural effusion | 20 | 72 | 8 |
Table 2: Frequency of imaging freatures.
Tables 3 to 5 give the percentage of patients with other symptoms. Table 3 shows general other symptoms, Table 4 shows chest X-ray related other symptoms and Table 5 shows CT scan related other symptoms. (Table 3-5).
| Other Symptoms Value | Frequency | Percentage |
|---|---|---|
| Vomiting | 17 | 5 |
| Wheeze | 12 | 4 |
| Productive Cough/Sputum | 30 | 9 |
| Falls | 16 | 5 |
| Haemoptysis | 4 | 1 |
Table 3: Frequency of symptoms.
| CXR Other Value | Frequency | Percentage |
|---|---|---|
| Pleural Effusion | 12 | 4 |
| Atelectasis | 3 | 1 |
| Bronchiectasis | 1 | 0 |
Table 4: Frequency of “Atypical” Imaging Features on Chest X-Ray.
| CT Other value | Frequency | Percentage |
|---|---|---|
| 224 | 73 | |
| Atelectasis | 1 | 0 |
| Bronchiectasis | 1 | 0 |
| Cardiomegaly, pulmonary oedema | 1 | 0 |
| Pulmonary Fibrosis | 1 | 0 |
| N/A | 83 | 25 |
Table 5: Frequency of “Atypical” Imaging Features on Chest CT.
Table 6 includes the numbers and percentages of males and females who had ‘Yes’ for each of the CXR and CT variables. The Fisher’s exact test was carried out, where possible, to test whether there was a statistically significant difference between the number of males and females for each symptom. The test p-values are given, where p<0.05 is considered a significant result.
| Female | Male | Total | p-value | |
|---|---|---|---|---|
| Normal CXR | 36 (23.4%) | 22 (12.4%) | 58 (17.5%) | 0.0086 |
| Abnormal CXR (n=266) | - | - | - | - |
| RN Opacities | 3 (2.7%) | 2 (1.3%) | 5 (1.9%) | 0.6534 |
| Consolidation | 97 (85.8%) | 139 (90.8%) | 236 (88.7%) | 0.2406 |
| Basal | 88 (77.9%) | 118 (77.1%) | 206 (77.4%) | 0.8814 |
| Peripheral | 62 (54.9%) | 79 (51.6%) | 141 (53.0%) | 0.6168 |
| Bilateral | 82 (72.6%) | 119 (77.8%) | 201 (75.6%) | 0.4678 |
| Normal CT (n=332) | 0 (0.0%) | 2 (1.1%) | 2 (0.6%) | 0.5385 |
| Abnormal CT scan: Classic Signs (n=50) | - | - | - | - |
| GGO | 16 (88.9%) | 29 (90.6%) | 45 (90.0%) | 1 |
| Crazy paving | 10 (55.6%) | 13 (40.6%) | 23 (46.0%) | 0.3817 |
| Air Bronchograms | 6 (33.3%) | 9 (28.1%) | 15 (30.0%) | 0.7544 |
| Sub pleural | 17 (94.4%) | 26 (81.2%) | 43 (86.0%) | 0.3978 |
| Bilateral | 17 (94.4%) | 28 (87.5%) | 45 (90.0%) | 0.6418 |
| Abnormal CT scan: Intermediate (n=50) | - | - | - | - |
| Central | 6 (33.3%) | 9 (28.1%) | 15 (30.0%) | 0.7526 |
| Unilateral | 1 (5.6%) | 3 (9.4%) | 4 (8.0%) | 1 |
| Lymphadenopathy | 1 (5.6%) | 6 (18.8%) | 7 (14.0%) | 0.3955 |
| Abnormal CT scan: Atypical (n=50) | - | - | - | - |
| Cavitation | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | * |
| Calcification | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | * |
| Pneumothorax | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | * |
| Pleural effusion | 3 916.7%) | 7 (21.9%) | 10 (20.0%) | 1 |
Table 6: Male and Female Imaging Features.
Overall, the difference in the number of abnormal chest X-rays (CXR) between males and females was significant (p= 0.0086) but within those abnormal X-rays there were no individual symptoms showing significant differences between the sexes. Only 52 patients underwent a CT scan and no significant difference was found between males and females for the number of abnormal CT scans, or for any of the symptoms in the abnormal CT scan group. (Table 6)
Discussion
SARS-CoV-2 is a newly discovered and named single strand, positive-sense RNA coronavirus1. This is a retrospective study which investigates the epidemiology and clinical features of swab positive (RT-PCR test) Covid-19 patients in relation to their imaging findings. It was done during the first wave of Covid-19 in the region between March 2020 and April 2020. The study reveals useful information about the clinical presentation, the most common clinical features observed in this infection and the commonly observed imaging manifestations of this infection in swab positive cases. It addition it also highlights some unusual clinical manifestations observed and less common imaging findings noted in a small percentage of cases.
The study included patients with positive RT-PCR test for Covid-19, who also had Chest radiograph, CT scan of the chest or CT Pulmonary angiogram study in this period between April 2020 to May 2020. Out of the total number of 332 cases [4, 10]. 46% were female and 54% male. The maximum number of cases was between the age group of 55 and 85 years, mean age being 71 years. 94% of the patients in our study were Caucasian.
Dry cough, fever were the most common clinical symptoms observed in our study, which is consistent with recent literature published [10, 12]. Studies have shown that fever, cough, dyspnoea are the most common symptoms of Covid-19 infection. Less common manifestations noted in our study like haemoptysis were seen in 1% of the cases, while 5% patients had vomiting, falls. These are not the usual signs of Covid-19 infection.
Out of the patients who had Chest radiograph, 17% were normal. Among the abnormal chest X ray results, the most commonly observed findings were consolidation with bilateral, basal and peripheral predominance. 2% of the cases had reticulonodular opacities. 4% cases had pleural effusion on Chest radiograph, whereas 1% had collapse/ atelectasis. 52 patients had CT scan of the Chest. No significant difference was observed with the sex ratio distribution regarding abnormal CT findings in our study. Among the patients who had CT Chest/CTPA, the most common finding observed was ground glass opacification in predominant basal, bilateral, sub pleural distribution. Less common findings or atypical features on CT included atelectasis, bronchial dilatation, pulmonary oedema and mild pericardial effusion. These findings are in concordance with studies showing predominant pattern of abnormality of GGO, with bilateral, peripheral distribution [6, 9]. Most of the Chest CT findings observed are consistent with recent literature.
Combining assessment of imaging features with clinical findings could hence facilitate diagnosis of Covid -19 infection in patients with clinical symptoms highly suspicious for Covid-19 infection. Diagnosis should also be based in addition on RT-PCR result in patients with high clinical suspicion.
Limitations
This study has several limitations. One limitation is that the sample includes only those patients with positive Covid-19 swab test (RT-PCR) and those who had some form of imaging like Chest radiograph, CT Chest/CTPA. We thus lack data on patients with negative RT-PCR result with imaging findings typical of Covid -19 infection and those with positive RT-PCR test and did not have any imaging like Chest radiograph or CT scan of Chest. Another limitation is that this is a small scale analysis, and only sampled patients during the first major wave of covid-19. It is possible that there may be variance in patient presentation as new variants have emerged and clearly further studies are needed.
Although now there is extensive data published on imaging findings in Covid -19 cases, it still remains a challenge and limits specificity. The commonly observed CT finding of GGO is also found in some other viral pneumonia. Bilateral, sub pleural dominance is also a pattern in some other pneumonia [13]. Also the patients with Covid -19 may develop further lung complications like ARDS, thromboembolism which complicates the interpretation of CT imaging. Another consideration is selection bias, with the sickest patients most likely to undergo imaging. Limitations with regards to interpretation of the Chest radiograph/CT findings also affected with factors like days since the infection and underlying comorbidities.
Conclusion
The Coronavirus pandemic has had great impact on our society. The healthcare system in the UK and internationally has been stretched. Medical imaging has contributed greatly to the diagnosis and management of COVID-19 and its complications. In the first wave of the pandemic clinicians observed the varying presenting symptoms from typical symptoms of sore throat, fever, loss of smell and short of breath to abdominal pain or renal colic symptoms. The latter two would be subsequently diagnosed with COVID-19 pneumonia on CT imaging of the abdomen which routinely incorporates the lung bases. Due to this phenomenon, we altered our abdominal pain protocol to incorporate a CT pulmonary angiogram and a portal venous abdomen and pelvis.
For patient presenting with suspected COVID-19 pneumonia, a chest X-ray was one of the initial investigations but any patient deemed a candidate for invasive ventilation would be escalated to a CT pulmonary angiogram to seek out severity of the COVID-19 pneumonia and to exclude a pulmonary embolus (a recognised complication with COVID-19 pneumonia).
Typical imaging findings such as ground glass consolidation, crazy paving in a peripheral, basal and bilateral distribution were demonstrated on CT of the chest, which is consistent with many other studies. This study corroborates imaging findings from earlier studies.
References
- World Health Organisation (2020) Clinical management of COVID-19: Interim Guidance 27 May 2020. World Health Organisation.
- Liu Y, Yan LM, Wan L, Xiang TX, Le A et al (2020) Viral dynamics in mild and severe cases of COVID-19. The Lancet. Infectious Diseases 20:656-657.
- World Health organisation Coronavirus Symptoms (2020) found on the World Wide Web World Health organisation.
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team (2020) vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China. China CDC Weekly 2:113-122.
- Cozzi D, Albanesi M, Cavigli E, Moroni C, Bindi A et al (2020) Chest X‑ray in new Coronavirus Disease 2019 (COVID‑19) infection: findings and correlation with clinical outcome. La Radiologia Medica 125:730-737.
- Choi H, Qi X, Yoon SH, Park S J, Lee K H (2020) Extension of coronavirus disease 2019 (CVID-19) on chest CT and implications for chest radiograph interpretation. Radiology: cardiothoracic Imaging 2:e200107.
- Ai T, Yang Z, Hou HY, Zhan C, Chen C (2020) Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a repost of 1014 cases. Radiology 296:E32-E40.
- Fang Y, Zhang HQ, Xie J, Ying L, Pang P et al (2020) Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 296: E115-E117.
- Shi H, Han X, Jiang N, Cao Y, Alwalid O et al (2021) Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. The Lancet 20: 425-434.
- Bi Q, Wu Y, Mei S, Ye C, Zou X (2020) Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. The Lancet: infectious Diseases 2:911-919.
- British Society of Thoracic Imaging (2020) BSTI COVID-19 CXR Report Proforma. Available from British Society of Thoracic Imaging.
- Chen N, Zhou M, Dong X, Qu J, Gong F et al (2020). Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 395:507-513.
- Guan C S, Lv Z B, Yan S, Du YN, Chen H (2020) Imaging Features of Coronavirus disease 2019 (COVID-19): Evaluation on Thin-Section CT. Academic Radiology 27:609-613.
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Cross Ref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Indexedat Google Scholar Crossref
Citation: Barlow N, Ibrahim M, Shah M, Gavai B (2022) Retrospective analysis of the epidemiology and clinical features of COVID-19 swab positive patients in relation to their imaging characteristics. OMICS J Radiol 11: 360. DOI: 10.4172/2167-7964.1000363
Copyright: © 2022 Barlow N et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3993
- [From(publication date): 0-2022 - Nov 14, 2025]
- Breakdown by view type
- HTML page views: 3279
- PDF downloads: 714