Retroprospective Study of Discard Rate in Department of Transfusion Medicine of a University Medical College of North India
Received: 31-Aug-2022 / Manuscript No. JCEP-22-73363 / Editor assigned: 05-Sep-2022 / PreQC No. JCEP-22-73363 (PQ) / Reviewed: 26-Sep-2022 / QC No. JCEP-22-73363 / Revised: 05-Oct-2022 / Manuscript No. JCEP-22-73363 (R) / Published Date: 19-Oct-2022 DOI: 10.4172/2161-0681-22.12.418.
Abstract
Background: This study was conducted in the blood centre at MMDU, Mullana. The aim of study was to calculate the discard rate during the study period and finding out the reasons responsible for them in order to provide suggestions for further improvisation in blood transfusion techniques.
Design: Study was carried out over a period of 6 months i.e. August, 2019 to January, 2020. The conducted study was retroprospective. Data for study period was collected from the blood centre records. The testing protocol was followed in the blood centre in accordance to NABH guidelines.
Result: During the study period of 6 months, a total of 4311 units were collected, which were later subjected to component preparation. Out of the components prepared, 4114 units were issued and 643 were discarded due to various reasons, resulting in discard rate of 15.62%. Outdating was the leading cause of wastage, followed by seropositivity. Platelet concentrates and PRBC’s were the most discarded components, respectively.
Conclusion: A closer look on the handling and usage of blood and its components would aid in focusing the various causes of blood wastage. Additionally, it would help in planning reformative measures to minimize blood wastage in future, as well as spreading awareness of the same. Simple and economical methods of improvement such as staff education, improved handling and transportation of blood units can have a tremendous influence in reduction of blood wastage as it always was, and for the foreseeable future, will be an issue for blood centres.
Keywords: Blood; Blood components; Transfusion medicine, Discard rate; Quality indicator
Introduction
Blood Transfusion Services (BTS) play an indispensable role in patient’s health care services. The high quality of blood and blood products, in addition to their injudicious use may additionally have an effect on the health care facility [1]. Safe and sufficient supply of blood and its components should be the aim of BTS. More and more provisions for safe blood are demanded by advances made in medical sciences for the welfare of patients [2]. Increase in the means essential for the collection and management of blood and its components can improve the efficiency of BTS. This can also be achieved by using existing resources more cautiously in order to subjugate the supply and demand difference. Therefore, every blood unit is indispensable and must be utilized with caution to reduce wastage [3]. The supply of blood in numerous countries fall short of the demand for blood. The data from World Health Organization (WHO) points out that less than half of the required collection is made by 87.5% of developing countries to meet the transfusion demands [4]. This demand-supply gap can either be filled by providing more resources into collection or by utilizing the present resources judiciously. Reduction of discard rate is an example of using the resources judiciously [5]. It is notable that only a few countries today have improvised upon necessary structures required for the betterment of BTS. Utilization of economic and material resources, preparation and implementation of a practical plan of action based on actual descriptions, analysis of current status of particular country, blood supply, standard and proper storage conditions, appropriate clinical conditions in treatment involving use of blood products and following the guidelines of blood and its product’s prescriptions are keystones of success [6]. Processes and manuals should be profoundly centered around creating quality blood components that are increasingly effective and safe. The essential segment in the quality control framework is blood donation, which is collected from prospective donors of different ages with different socioeconomics, wellbeing profiles and this blood collection in most parts of the world relies upon manual procedures which may have technical variations. In this way, these donations will be screened, stored and shipped under a variation of ecological circumstances [7]. An efficient and coherent BTS would improve patient care and further promote the progress of medical sciences in the country [8]. Therefore, it is necessary for any blood centre to encourage high standards of quality in all regards of blood transfusion managements. Internal Quality Control (IQC) is the foundation of quality administration program in the blood centre [9]. In the modern times, quality control of blood and its components guarantee the auspicious accessibility of a blood unit of high quality yield with the most extreme adequacy and insignificant hazard to potential recipients [10]. Blood products with short shelf life are bound to have a certain level of wastage, which is both inevitable and necessary to ensure safety and good quality of blood products [11]. The efficiency of BTS can be monitored by considering discard rate as a quality indicator. High wastage rate leads to decrease in efficiency and increase in the cost of production of blood and its components [12]. Because blood utilization practices vary widely, information is needed to determine areas of blood management that can be reformed to reduce wastage of blood in developing countries.
The paediatrics and gynecology departments make most requests for blood in most hospitals [13]. These variations may compromise the basic control guides which are planned towards the improvisation of the nature of the blood products. A great deal of medical and surgical specialties relies upon the constant blood supply. The main task for a newly set up blood centre is to administer quality management system in all levels of collection, processing and storage of blood [14]. Various reasons of discard of blood and its components are Transfusion Transmitted Infection (TTI) reactivity, expiration, insufficient volume, leakage, clot formation, haemolysed and return back unused after issue. Platelets have the highest incidence of discard because of their short shelf life, followed by Packed Red Blood Cell (PRBC) and Fresh Frozen Plasma (FFP) [15]. Preferably, expiration of blood and its components should be avoided. Nonetheless, due to imminent requirement to have stock available at all times and frequent uncertain emergencies allow the acceptance of low expiration rates imminently [16]. Units requested by wards, that are neither transfused, nor returned to blood bank (within defined time period and temperature as per the component issued) and units that have exceeded their shelf life are the two prime reasons behind wastage of blood in hospitals. The units (that are issued, but not transfused) kept between a temperature range of 1°C-6°C, can be accepted in compliance with one of the criteria’s of U.S. Food and Drug Administration and AABB guidelines. The “30-minute” rule is still applicable in some blood centres, according to which RBC units can be accepted back by blood centres, if they are kept in temperature controlled containers since the time of issue to the time unit is returned and the unit is received back to blood centre inventory within 30 minutes. National Accreditation Board for Hospitals and Health care providers list wastage/discard rate 3rd among the 10 quality indicators. Regular transfusion audits should be carried out in the blood centre to know the utilization trends. Unnecessary transfusions may contribute to shortage of blood products and each indication for requisition of blood products should be justified. Blood centres should carry out routine audits in order to be up to date with blood usage trends [17]. Finding out the reasons for wastage of blood and its products, so that the preparation and use of blood and its components can be optimized through staff education and training was the objective of this study. This aids in developing guidelines for donor screening, preparation of components and their storage [18]. Study of discard rate and its aspects is an under-valued point in regards to the improvement of BTS and concerning literature is sparse.
Aim and objective
1. To evaluate the overall discard/wastage rate of blood and its components in blood centre of a deemed to be University teaching and tertiary care hospital of North India
2. To compare the result with other similar studies done in India and Abroad
3. To understand the different factors that lead to blood wastage, and use the knowledge gained from this to :
• Observe the future trend of blood discard
• Take remedy actions necessary to prevent excessive blood wastage
Materials and Methods
Study area
Department of transfusion medicine in tertiary care hospital of Northern India
Study population
This study is a hospital based study; it was conducted in hospital
Study design
Observational retro prospective study
Study duration
Study was carried out over a period of 6 months i.e. 1 Aug, 2019 to 31 Jan, 2020
Study analysed
Various reasons of discarded blood and blood components bags
Inclusion criteria
Blood bags donated by donors, fulfilling NACO criteria for donor selection, discarded for different reasons were included in this study after checking medical history and brief clinical examination by the medical officer. The donors were either voluntary or replacement. Replacement donors were either relatives or friends of the patients.
The whole blood was collected in single, double, triple and quadruple bags and components were prepared as per Drugs & Cosmetic Act, 1940 and Rules 1945. Citrate Phosphate Dextrose Adenine anticoagulant blood bags were used for WB collection and Saline Adenine Glucose Mannitol additive solution as preservative for PRBC. The components were prepared by Platelet rich plasma method. The quality of WB and blood components was evaluated as per the National Accreditation Board for Hospitals and Healthcare Providers (NABH) Guidelines [14]. All the blood units were subjected to Enzyme Linked Immune Sorbent Assay (ELISA) for TTI testing. Only seronegative products meeting the quality parameters were issued and the rest were discarded. 1% of individual blood bags (WB, PRBC, PC, FFP) were subjected for QC [19].
Data analysis
Data was collected after obtaining ethical clearance before the study from authorities concerned. It was collected from the blood bank data record. The present study includes blood units discarded for different reasons, which include Transfusion Transmitted Infection (TTI) reactivity, expired, insufficient volume, leakage, clotted, hemolysis and return back unused after issue. Blood components (Packed RBC (PRBC), Platelet Concentrate (PC), and (FFP) Fresh Frozen Plasma) were prepared from 350/450 ml blood bags under aseptic conditions according to Drug and Cosmetic Act guidelines as per demand and staff available in the blood centre [20].
Method of discarding blood
Bags to be discarded due to any reason mentioned above are autoclaved at temperature of 121° C for 20 minute. Autoclaved bags are directly handed over to biomedical waste staff (Table 1).
| Months | Total unit collection |
|---|---|
| August,19 | 693 |
| September,19 | 746 |
| October,19 | 1035 |
| November,19 | 652 |
| December,19 | 480 |
| January,20 | 705 |
| Total | 4311 |
Table 1: Total No. of blood/components collected.
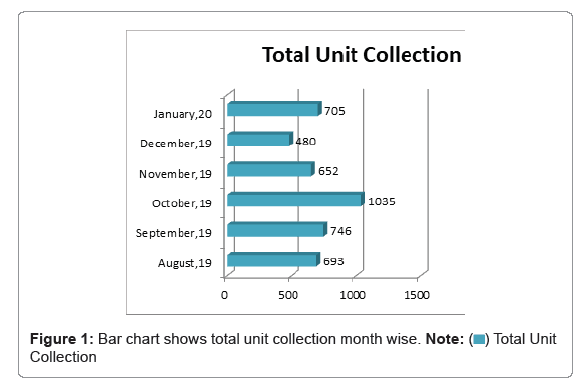
In the above table, total collection of blood units during the study period of 6 months from August, 19 to January, 20 is recorded 4311 units. Maximum units were collected in the month of October, 19 i.e. 1035 units while December, 19 recorded the lowest collection of 480 units. Number of blood units collected in the months of August, 19, September, 19, November, 19 and January, 20 were 693, 746, 652 and 705, respectively (Figure 1).
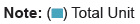
Total number of units issued from August, 19 to January, 20 are 4114, as shown in this table. The highest number of units were issued in the month of October, 19, i.e. 780 while November, 19 recorded the least number of issued units, i.e. 603 [21-25]. Units issued in the months of August, September, December and January are 733, 636, 666 and 696, respectively (Figure 2 and Tables 2,3).
| Months | Total issued units |
|---|---|
| August,19 | 733 |
| September,19 | 636 |
| October,19 | 780 |
| November,19 | 603 |
| December,19 | 666 |
| January,20 | 696 |
| Total | 4114 |
Table 2: Total No. of blood/components issued.
| Months | Total discarded units |
|---|---|
| August,19 | 87 |
| September,19 | 72 |
| October,19 | 135 |
| November,19 | 157 |
| December,19 | 79 |
| January,20 | 113 |
| Total | 643 |
Table 3: Total No.of blood/components discarded.
The above table shows the number of discarded blood units in the months of August, 19 to January, 20. The total units discarded in 6 months are 643 (includes both Whole Blood and Components). November, 19 recorded the highest no of discarded unit’s i.e.157 units, followed by 135 units in October, 19 and 113 units in January, 20. August, September and December of 2019 recorded comparatively lesser number of discarded units than the months mentioned above. The numbers of units discarded in these months are 87, 72 and 79, respectively (Figure 3 and Table 4).
| Months | Total WB’s discarded | Total PRBC’s discarded | Total FFP’s discarded | Total platelets discarded |
|---|---|---|---|---|
| August,19 | 10 | 6 | 2 | 74 |
| September,19 | 17 | 13 | 11 | 53 |
| October,19 | 3 | 129 | 26 | 29 |
| November,19 | 3 | 143 | 15 | 27 |
| December,19 | 8 | 9 | 4 | 67 |
| January,20 | 4 | 7 | 7 | 109 |
| Total | 45 | 307 | 65 | 359 |
Table 4: Total No. units of discarded blood/component wise.
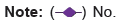
This table provides information about the type of blood component (WB, PRBC, FFP AND PL) discarded during the study period in each month [26-31]. Platelets contributed the most to the discard rate in blood bank, followed by PRBC’S and FFP’s, while Whole Blood units contributed the least (Figures 4,5 and Table 5).
| Type of blood unit /component | No. of units | Discard rate |
|---|---|---|
| WB | 45 | 1.09% |
| PRBC | 307 | 7.46% |
| FFP | 65 | 1.57% |
| Platelets | 359 | 8.72% |
Table 5: Discard rate component wise.
This table shows the discard rate of individual components in our study period. Platelets contributed 8.72%, most to the total discard rate, followed by 7.46% PRBC’s, 1.57% FFP’s and 1.09% WB units (Figures 6,7 and Table 6).
| Months | Total expired units discarded | Total TTI positive units discarded | Total units discarded due to leakage | Total units discarded due to haemolysis |
|---|---|---|---|---|
| August,19 | 81 | 4 | 0 | 3 |
| September,19 | 58 | 14 | 0 | 1 |
| October,19 | 106 | 26 | 0 | 3 |
| November,19 | 140 | 16 | 0 | 2 |
| December,19 | 71 | 5 | 1 | 2 |
| January,20 | 103 | 9 | 0 | 1 |
| Total | 558 | 73 | 1 | 12 |
Table 6: Various reasons for discard month-wise.
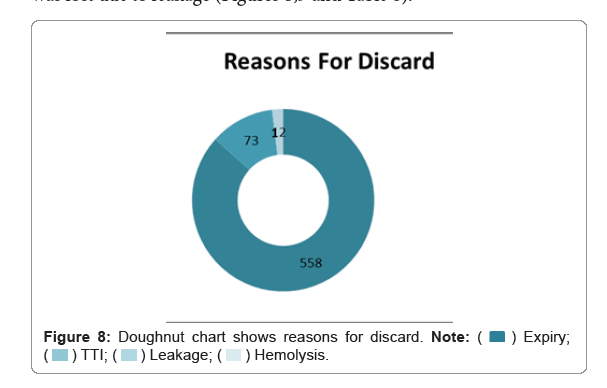
This table provides an insight into various major reasons for blood wastage. In our study, expiry and TTI positivity of blood units turned out to be the 2 leading causes of blood discard. Most expiration of blood happened in the months of October and November of 2019. 12 units were discarded due to hemolysis while one unit was discarded due to leakage (Table 7).
| Reasons for discarding | No. of units | Discard rate |
|---|---|---|
| Expiry | 558 | 13.56% |
| TTI | 73 | 1.77% |
| Leakage | 1 | 0.02% |
| Hemolysis | 12 | 0.29% |
Table 7: Various reasons of discard in total.
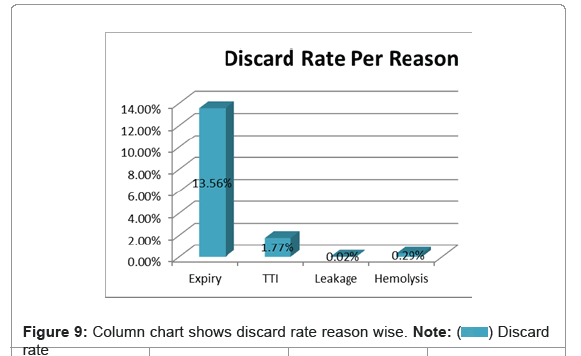
This table shows the various reasons responsible for the wastage of blood. Expiration, without doubt, is the leading cause because of the short shelf life of platelets [32-34]. A total of 558 units were wasted due to expiration. TTI is the second leading cause of wastage in our study, contributing 73 units. Hemolysis accounted for 12 units and one unit was lost due to leakage (Figures 8,9 and Table 8).
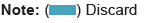
| Discard rate per month | |||
|---|---|---|---|
| Months | Total discarded units | Total issued units | Discard rate |
| August,19 | 87 | 733 | 11.86% |
| September,19 | 72 | 636 | 11.32% |
| October,19 | 135 | 780 | 17.30% |
| November,19 | 157 | 603 | 26.03% |
| December,19 | 79 | 666 | 11.86% |
| January,20 | 113 | 696 | 16.23% |
| Total | 643 | 4114 | 15.62% |
Table 8: Total discard rate during study period.
This table marks the number of discarded units in each month and in totality of 6 months. November was the highest contributor to the wastage rate with 157 units and 26.03%. October, 19 was a close second in terms of number of units as 135 of its units were discarded, marking the month for 17.30% wastage rate? Wastage of 113, 87 and 79 units in the months of January, August and December, marked the months for 16.23%, 11.86% and 11.86%, respectively. September was the month with least number of units discarded in terms of number, as well as percentage, as 72 of its units with a monthly wastage rate of 11.32% were discarded.
A total of 643 units were discarded in the span of 6 months from August, 19 to January, 20 and 4114 units were issued during this period. So, from the formula of calculating wastage rate, total discard rate of 6 months turned out to be 15.62% (Figures 10 and 11).
| Sr. No. | Year | Study | Discard rate |
|---|---|---|---|
| 1 | 2014 | Study of rate and causes of blood components discard among Ahwaz's hospital [24] | 12% |
| 2 | 2015 | Blood Wastage Rate in a Sub-Saharan African Hospital Based Blood Bank[13] | 11.73% |
| 3 | 2016 | Blood discard rate in a blood center in Curitiba – Brazil. Ten years of study[27] | 10.20% |
| 4 | 2016 | Analysis of discard of whole blood and its components with suggested possible strategies to reduce it[2] | 22.45% |
| 5 | 2017 | Study of Utilization of Blood and Blood Components in a Tertiary Care Hospital[31] | 6.20% |
| 6 | 2017 | Analysis on Discard of Blood and Its Products with Suggested Possible Strategies to Reduce Its Occurrence in a Blood Bank of Tertiary Care Hospital[30] | 6.95% |
| 7 | 2018 | Discard of Blood and blood Components With Study of Causes – A Good Manufacture Practice[32] | 1.60% |
| 8 | 2019 | Reasons and Recommendations to Reduce Wastage Pattern of the Blood Components in the Newly Started Tertiary Care Hospital Based Blood Center in East India[37] | 22.80% |
| 9 | 2019 | Pattern of Utilization of Blood and Blood Products[34] | 17.90% |
| 10 | 2020 | Retro prospective Study of Discard Rate in Department of Transfusion Medicine of a University Medical College of North India | 15.62% |
Table 9: Comparison of overall discard rate among various studies in last few years.
Discussion
In recent years, most countries have emphasized towards implementing various strategies in order to further a step towards reduction in discard rate at their blood centres. With new and better treatment techniques developing every day, precise and improved diagnosis of disorders requiring transfusions are being made possible. Efficient and thoughtful management at blood centres is the first step towards reducing wastage of blood, which can save countless lives. Recent Patient Blood Management is the key to reduce discard of blood.
A balance is required between supply and demand in order to provide sufficient supply of blood. At current rate, the supply of blood doesn’t catch up with the demand for blood. The best way to keep a check on this balance in blood centres is to conduct self-audits to find out reasons for discard of blood and its components over a defined time period and assess if the reasons are avoidable. It helps in formulating different strategies to reduce the blood wastage [3].
The aim of this study was to evaluate the discard rate and its various causes in the blood centre of a University Medical College in North India. This retroprospective study was done for a period of 6 months i.e. Aug, 19 to Jan, 20. There are different perspectives when it comes to comparison of different studies with this one. Overall wastage rate, most common reasons of discard and contribution of TTI to the total wastage are the primary comparative aspects to this study [35-37]. Overall discard rate in this study was 15.62%, which is comparatively lower than studies no [27,32,37], while it was higher than studies numbered [2,13,24,30,31,34], as shown in Table 9.
Outdating was the leading cause of wastage in this study, followed by seropositivity, hemolysis and leakage. Platelet concentrate were the most expired units, followed by PRBC’s. Constant and proportional production of PC is necessary because of their short shelf life, which often leads to expiry. Maximum discard of PRBC’s was in the months of October and November of 2019. These months are attributed to the admission of dengue cases, when PC are prepared in advance and in comparatively higher quantities to fulfil the needs of patients. PRBC’s are prepared in order to obtain RDP, but not used to that extent, which leads to their expiration, causing high discard rate of PRBC’s in these particular months. Studies, in which expiration was the leading cause of discard, were compared with this study. Expiration rate in this study was higher than studies numbered [6,23,26], while it was almost same to study numbered [24]. Studies in which seropositivity played the most prominent role were compared to this study. This comparison shows that seropositivity contributed much lesser to the total wastage rate in this study, as compared to other studies [12,18,19,28]. Hemolysis and leakage as leading causes of discard were not seen in any other studies.
Conclusion
A closer look on the handling and usage of blood and its components would aid in focusing the various causes of blood wastage. Additionally, it would help in planning reformative measures to minimize blood wastage in future, as well as spreading awareness of the same. Simple and economical methods of improvement such as staff education, improved handling and transportation of blood units can have a tremendous influence in reduction of blood wastage as it always was, and for the foreseeable future, will be an issue for blood centres. There is no liberty for technical or administrative leniency when handling an invaluable commodity like blood. Availability of more resources or improved efficiency of present ones can overcome the shortage of blood.
Recommendations
• Education and counselling of donors can help with self- deferral among donors that can lead to a decline in no. of seropositive cases.
• Stock management and other records in blood centres should be maintained on computers through specific software that can help in detection of units before their expiration for efficient use.
• Daily checks through the stock of blood must be administered to ensure the detection of units that are about to expire, so that they can be issued before other units.
• Regular training of staff and audits should be conducted in blood centres to keep the staff prepared for any possible scenarios.
• More Plasma fractionation centres should be setup so that excess plasma can be sent for plasma separation.
• Wards requesting blood units must be aware of their need of blood, and fill requisitions more cautiously, as issued but not transfused blood is a very prominent reason for discard in most blood centres.
• Patient Blood Management should be implemented in clinical wards
References
- Varshney L,Gupta S (2017) Quality indicators- performance tools of blood transfusion services. J Evol Med Dent Sci 6(90):6348-6352.
- Patil P, Bhake A, Hiwale K (2016) Analysis of discard of whole blood and its components with suggested possible strategies to reduce it. J Res Med Sci 4(2): 477-481
- Goel N, Sudhakar D (2019) An analysis on blood product usage and wastage in a rural tertiary care hospital, Konkan belt of Maharashtra, India. Int J Pathol 9(3):144-149.
- Kurup R, Anderson A, Boston C, Burns L, George M, et al. (2016) A study on blood product usage and wastage at the public hospital, Guyana. BMC Res Notes 9(1).
- (2015) Transfusion Update. Jaypee Publishers.
- Far R, Rad F, Abdolazimi Z, Kohan M (2014) Determination of rate and causes of wastage of blood and blood products in iranian hospitals. Turk J Hematol 31(2):161-167.
[Cross Ref][Google Scholar](all versions)
- Liumbruno G, D'Amici G, Grazzini G, Zolla L (2008) Transfusion medicine in the era of proteomics. J Proteome Res 71(1):34-45.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Roy A, Pal A (2015) Evaluation of ‘Wastage Rate’ of blood and components-An important quality indicator in blood banks. Br J Med Med Res 2015;8(4):348-352.
[Cross Ref][Google Scholar](all versions)
- Sultan S, Zaheer H, Waheed U, Baig M, Rehan A, et al. (2018) Internal quality control of blood products: An experience from a tertiary care hospital blood bank from Southern Pakistan. J Lab Physicians 10(1):64.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Franchini M, Capuzzo E, Turdo R, Glingani C (2014) Quality of transfusion products in blood banking. Semin Thromb Hemost, 40(02): 227-231.
[Cross Ref][Google Scholar](all versions)[PubMed]
- National blood and blood product wastage reduction strategy 2013-2017. National Blood Authority, Austrailia.
- Cobain TJ (2004) Fresh blood product manufacture, issue, and use: A chain of diminishing returns? Transfus Med Rev. 2004;18(4): 279-292.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Atinuke F, Adebola S, Rachael K (2016) Blood wastage rate in a sub-saharan african hospital based blood bank. Int blood res rev 4(4):1-6.
- (2013) National Accreditation Board For Hospitals and Healthcare Providers(NABH). Accreditation standards on Blood banks/ Blood centers and Transfusion Services. 72-75.
- Morish M, Ayob Y, Naim N, Muhamad N, Salman H, et al. (2012) Quality indicators for discarding blood in the National Blood Center, Kuala Lumpur. Asian J Transfus Sci 6(1):19.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Collins R, Wisniewski M, Waters J, Triulzi D, Yazer M (2015) Effectiveness of multiple initiatives to reduce blood component wastage. Am J Clin Pathol 143(3): 329-335.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Kafi-Abad SA, Omidkhoda A, Pourfatollah A (2019) Analysis of hospital blood components wastage in Iran (2005-2015). Transfus Apher Sci 58(1):34-38.
[Cross Ref][Google Scholar](all versions)[PubMed]
- Sreedhar BK, Suresh B, Arun R, Chandramouli P, Jothibai D (2015) Reasons for discarding whole blood and its components in a tertiary care teaching hospital blood bank in South India. J Clin Sci 4(3):213.
[Cross Ref][Google Scholar](all versions)
- Vimal M (2019) Pattern of Utilization of Blood and Blood Products in a Tertiary Care Hospital. Adv Pathol Lab Med 05(02):14-17.
- (1940) Drug and Cosmetic Act.
- Thakare MM, Dixit JV, Goel NK (2011) Reasons for discarding blood from blood bank of government medical college, Aurangabad. Asian J Transfus Sci 2011;5:59-60.
[Cross Ref][Google Scholar](all versions)
- Kora SA, Kulkarni K (2011) An analysis Of donor blood wastage in a blood bank in rural Karnataka. J Clin Diagn Res 5:1393-1396.
[Google Scholar](all versions)
- Gauravi D, Agravat A, Krupal MP (2012). Seroprevalance of HIV, HBV, HCV and syphilis in blood donors Saurashtra region of Gujarat: Declining trends over a period of 31/2 years. Online J Health Allied Sci 11:5.
- Singhal M, Patel M, Kapoor D, Mittal D (2013). A research analysis on blood component usage and wastage in blood bank and blood component center. J Physiol Pathophysiol 4(2): 23-28.
[Cross Ref][Google Scholar](all versions)
- Kumar A, Sharma S, Ingole N, Gangane N (2014). Analysis of reasons for discarding blood and blood components in a blood bank of tertiary care hospital in central India: A prospective study. Int J Community Med Public Health 4(1):72.
[Cross Ref][Google Scholar](all versions)
- Arora I, Singh S, Singh S (2018) Donor blood wastage: A study from blood bank Chamba (H.P). Int J Community Med Public Health 5(7): 3016.
[Cross Ref][Google Scholar](all versions)
- Ghaflez BM, Omeir HK, Far MJ, Saki N, Maatoghi JT, et al. (2014) Study of rate and causes of blood components discard among Ahwaz's hospital. Sci J Iran Blood Transfus Organ 11(3):197-206.
- Neetika S, Kaushik S, Kumar R, Azad S, Acharya S, et al. (2014) Causes of wastage of blood and blood components: A retrospective analysis. J Dent Med Sci 13:59-61.
[CrossRef]
- Bobde V, Parate S, Kumbhalkar D (2015). Analysis of discard of whole blood and blood components in government hospital blood bank in central india. J Evid Based Med Healthc 2(9):1215-1220.
- Monich A, Dantas T, Fávero K, Almeida P, Maluf E, et al. (2017) Blood discard rate in a blood center in Curitiba-Brazil. Ten years of study. Transfus Apher Sci 56(2): 130-134.
[CrossRef][Google Scholar](all versions)
- Punee K, Rupinder K, Victor M, Aikaj J (2016) Incidence and causes of wastage of blood & blood components in a blood bank of tertiary care hospital: A retrospective study. J Med Dent Sci 15(09):108-110.
- Shahshahani J, Taghvai N (2017) Blood wastage management in a regional blood transfusion centre. Transfus Med 27(5): 348-353.
[CrossRef][Google Scholar](all versions)
- Kanani A, Vachhani J, Dholakiya S, Upadhyay S (2017) Analysis on discard of blood and its products with suggested possible strategies to reduce its occurrence in a blood bank of tertiary care hospital in Western India. Glob J Transfus Med 2(2):130.
[CrossRef][Google Scholar](all versions)
- Giriyan SS, Chethana HD, Sindhushree N, Agarwal A, Nirala NK, et al. (2017) Study of utilization of blood and blood components in a tertiary care hospital. J Blood Lymph 7(2): 169.
- Mahapatra S, Ray G, Panigrahi R, Mishra D, Sahoo B, et al. (2016) Platelet audit: To weigh the rationality between requirement and uses in blood transfusion. Int J Res Med Sci Technol 4548-4551.
- Mukherjee G, Ghosh S, Halder S, Mondal S (2018) Study of “Discard Rate” of Whole Human Blood: Useful Blood Center Quality Indicator. J Sci Soc 45(3):116.
- Kumari N, Maheshwari A, Kumar N, Rabab S (2019) Reasons and Recommendations to Reduce Wastage Pattern of the Blood Component in the Newly Started Tertiary Care Center Blood Bank in East India. Int J Contemp Med 6(5).
Citation: Singh R, Kaur J, Singh AK, Singh M (2022) Retroprospective Study of Discard Rate in Department of Transfusion Medicine at University Medical College in North India. J Clin Exp Pathol 12: 418. DOI: 10.4172/2161-0681-22.12.418.
Copyright: © 2022 Singh R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2724
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 2327
- PDF downloads: 397

 Collection
Collection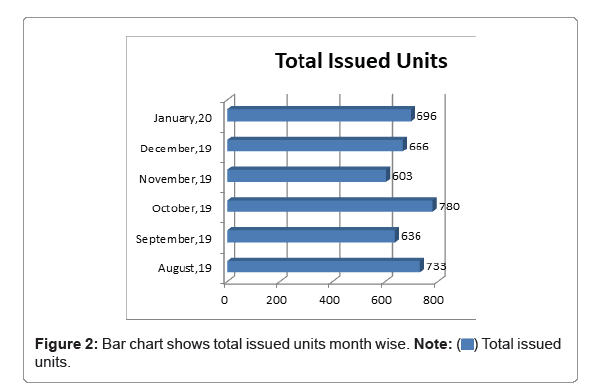
 units.
units.
 Total discarded units.
Total discarded units.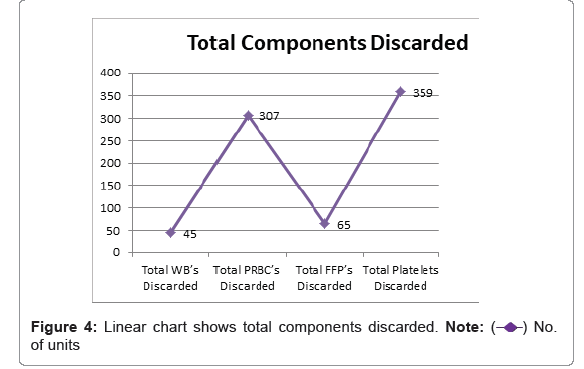
 of units
of units
 Total platelets discarded.
Total platelets discarded.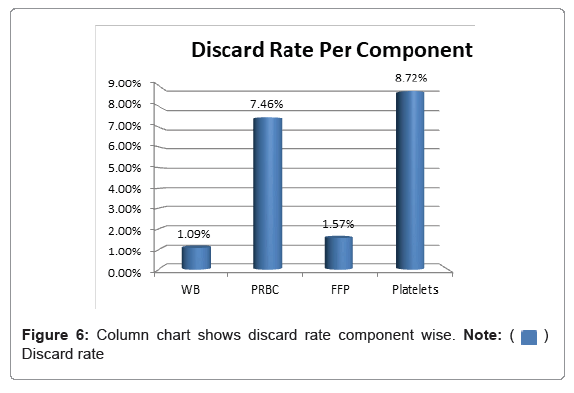
 Discard rate
Discard rate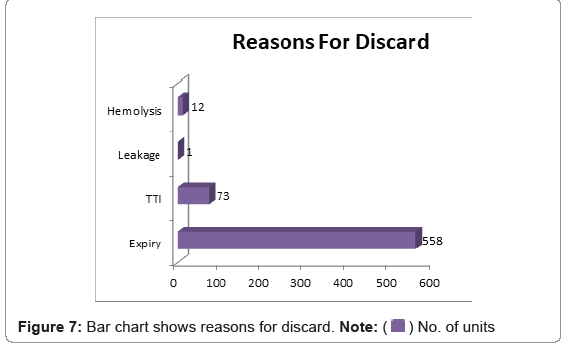



 rate
rate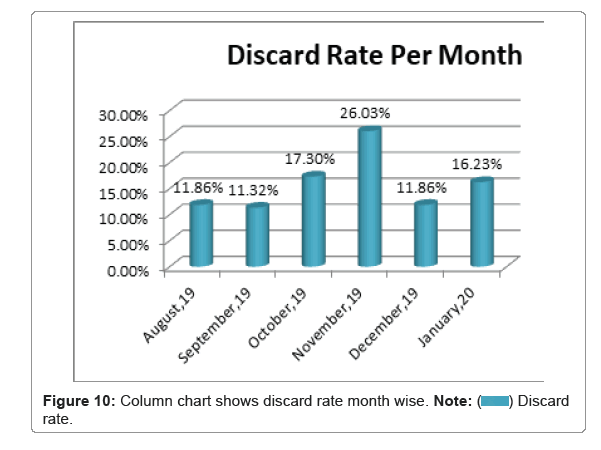
 rate.
rate.
 rate
rate