Research Article Open Access
Retention of Implant-supported Fixed Restorations Using Different Provisional Luting Agents
Mohamed Abdelmageed Awad1* and Tarek Rashad Abdelrehim2
1Associate Professor, Crowns and Bridges Department, Faculty of Dentistry, Tanta University, Egypt and King Abdulaziz University, Jeddah, KSA, Saudi Arabia
2Associate Professor, Conservative Dentistry Department, Faculty of Dentistry, Mansoura University, Egypt
- *Corresponding Author:
- Dr. Mohamed Abdelmageed Awad
Faculty of Dentistry
King Abdulaziz University, KSA
Tel: +966507680301
E-mail: mohamed_awad61@yahoo.com
Received Date: August 20, 2013; Accepted Date: August 30, 2013; Published Date: September 03, 2013
Citation: Awad MA, Abdelrehim TR (2013) Retention of Implant-supported Fixed Restorations Using Different Provisional Luting Agents. J Oral Hyg Health 1:112. doi: 10.4172/2332-0702.1000112
Copyright: © 2013 Awad MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Retrievability of cemented implant-supported fixed prosthesis is desirable. Objectives: Compare retentive force of several provisional luting agents when used with cemented superstructures and one implant system. Methods: Five ITI solid screw implant fixtures and solid conical abutments with 6º taper were used. Five metal ceramic crowns were fabricated and cemented with five different provisional luting agents named Tem Bond, Temp Bond NE, Fynal, TNE, and ImProv. Tensile retentive force necessary to debond each casting was measured 30 minutes after cementation in a dry condition (n=10) and after storing and thermocycling for 72 hours (5-55ºC) in artificial saliva (n=10). Mean and standard deviation of retentive force was calculated for all cements. Data were statistically analyzed using two way analysis of variance at 5% level of significance. Tukey’s post hoc test was performed. Statistical software (SPSS, v.16) was used for data analysis. Results: This study provided a rank order of different provisional luting cements according to their ability to retain crowns. Storing and thermocycling of specimens in artificial saliva for 72 hours caused significant reduction in the retentive values of all provisional luting agents investigated. Conclusion: The results may help the clinicians for selecting luting agent, retentive enough
Keywords
Implant-supported prosthesis; Provisional luting agents; Retentive forces
Introduction
Both high success rate and reduced cost of implants are from the main reasons that have increased the number of patients being treated with implant supported prosthesis now a day. The success of these restorations depends not only on the sound osseointegration of their implant fixtures but also on the integrity of the connection of the prosthetic superstructure to these fixtures. In screw-retained designs, loosening or breakage of the screws may lead to failure or replacement of the whole implant. However, for cement-retained designs, dissolution of luting agent may lead to loss of bond between the final prosthesis and implant abutment which should be recemented again [1].
Although the use of cemented superstructures greatly limits the retrievability of the prosthesis, it has been advocated as a successful method for simplifying the restorative phase of treatment. An advantage of cemented superstructures is that conventional prosthodontic procedures may be used during the clinical and laboratory phases of restorative treatment. Moreover, the luting agent-metal interface allows small discrepancies which are not acceptable in a screw-retained fixture and may even act as a shock absorber [2]. One more advantage of cemented superstructure is that minor divergences of implants can be easily corrected during abutment preparation which makes it even easier to accomplish aesthetic restorations as the abutment bulk can be more favorably managed [3].
On the other hand, one major disadvantage here is that, permanent cementation of such prostheses should only be considered when future retrievability of the prosthesis for repair or modification is not desired or when surgical correction of peri-implant tissue problems is not anticipated [4]. Moreover, permanent cementation of implantsupported restorations may become a great disadvantage in case of loosening of the abutment screw, porcelain fracture or even if framework fracture occurred [5,6].
Sometimes, conventional cast fixed prostheses are recommended to be provisionally cemented to abutment teeth in order to evaluate occlusion and tissue reactions. Indeed, provisional cementation of such restorations for up to two months has been advocated [7]. This implies also for implant-supported and implant-tooth-supported prostheses which are sometimes provisionally cemented to evaluate occlusion and occlusal loading of the implant fixture. Provisional luting agents may also be used as final luting agents in cases of implant supported restorations [2].
The type of provisional luting agents selected for a given clinical situation controls the amount of retention obtained [2,8,9]. However, provisional cementation is unpredictable to some extent, due to the many different factors that influence the retentiveness of a restoration and can result in difficult retrieval or premature loosening [10,11].
For implant systems in which the abutments are cemented to the fixtures, the provisional luting agent must be strong enough to resist functional forces, but weak enough to allow easy removal of the superstructure when necessary without harm to the abutment and implant fixture [2,12,13].
The purpose of this study is to compare and rank the retentive strength of several provisional luting agents when used with implant supported prostheses using ITI implant system, both after 30 minutes and after storing and thermo-cycling for 5000 cycles (5-55°C) in artificial saliva for 72 hours.
The null hypotheses indicate that there is no difference between all the provisional luting agents investigated either after 30 minutes or after 72 hours.
Materials and Methods
Five ITI solid screw titanium implant fixtures (TPS-surface) (4.1×1.0 mm and 5.5 mm solid conical abutments with 6 degrees taper (Straumann AG, Switzerland) were used in this study. Five cementretained metal cast crowns were fabricated on these abutments and cemented with different luting agents.
An autopolymerizing acrylic resin custom tray with a 2 mm. wax relief was used to make impression of the abutment with a polyvinylsiloxane impression (Reprosil medium viscosity, Caulk/Dentsply, Milford, Delaware). Improved dental stone (Silky Ro, Whip Mix, USA) was used to form stone die from the impression. One coat of die spacer (μ- spacer Major, Italy) was applied to the occlusal and axial surfaces of the die. A wax pattern coping was formed for each die by the use of blue inlay wax (Whip mix, Louisville, Kentucky, USA). A wax loop was formed on the occlusal portion of each coping for the attachment with the Universal testing machine. The patterns were sprued, invested and casted, in a high palladium casting alloy (Spartan Plus, Willams Gold Co., Buffalo, NY) following the manufacturer’s instructions. After divesting and sprue removal, the metal castings were sandblasted with aluminum oxide 110 μm. (Korox 110, BEGO Goldschlagerei Wilh. Herbst GmbH & Co., Germany). Adaptation of the metal castings to their abutments was evaluated with the use of disclosing medium (Fit-checker, Japan). All internal casting nodules were removed with no. 1/2 round bur. Metal castings were steam cleaned for 5 seconds and allowed to dry in air. Porcelain build-up was followed in the usual manner to simulate the process of producing crown as in clinical case.
Five different provisional luting agents were used to cement crowns to their implant abutments (Table 1). The luting agents were mixed according to the manufacturer’s instructions. A stiff brush was used to coat the inner surface of each crown with an even thickness of luting agent, and the crown was seated on the abutment with finger pressure for 10 seconds. A static constant load of 6 kg was applied for 10 minutes. Excess luting agent was removed from each specimen with a plastic instrument. The previous steps were repeated twenty times given that each crown was cemented to its corresponding abutment using the same luting agent every time to eliminate the possibility of abutments surface contamination or luting materials’ residues interaction. The retentive strength necessary to debond each crown was measured after exposure to two conditions. One, was after being stored at room temperature in a dry condition for 30 minutes (n=10), and the other was after being stored in artificial saliva for 72 hours where thermocycling for 5000 cycles (5-55°C) was done (n=10).
| Materials investigated | Code | Manufacturer | Composition |
| Tem Bond | TB | Kerr Mfg Co., Romulus, Michigan | Type I zinc oxide eugenol |
| Temp Bond NE | TBNE | Kerr Mfg Co., Romulus, Michigan | noneugenol zinc oxide |
| Fynal | FYN | Caulk, Dentsply, Milford, DE | polymer modified zinc oxide eugenol |
| TNE | TNE | Temrex, Freeport, NY | Diurethane dimethacrylate |
| ImProv | IMP | Steri-Oss, CA | polyurethane luting agent |
Table 1: Materials investigated in this study, their manufacturers and compositions.
The composition of artificial saliva is: Magnesium chloride (0.20 mM), calcium chloride dehydrate (1.0 mM), potassium dihydrogen orthophosphate (4.0 mM), HEPES (20.0 mM), potassium chloride (16.0 mM), ammonium chloride (4.5 mM). The pH was adjusted to 7.0 using potassium hydroxide (1.0 M).
The crowns were pulled from their abutments by means of a 500 kg load cell at a crosshead speed of 5 mm/minute on an Instron Universal testing machine (Model 1193, Instron Limited, UK). After tensile testing, the crowns and their abutments were placed in an ultrasonic cleanser containing cement removal solution (Removalon I, Primer Dental products Co., Norristown, Pa.) for 5 minutes. All crowns were allowed to dry in air and were inspected visually under magnification to ensure complete removal of luting agent residues. The use of bur or sandblasting was avoided to prevent changing of abutments’ and internal crowns surfaces. The force at which bond failure occurred was recorded. Mean and standard deviation of tensile force was calculated for all cements. Data were statistically analyzed using two-way Analysis Of Variance (ANOVA) at 5% level of significance. Tukey’s post hoc test was conducted within each condition to compare cements and within each cement to compare conditions. Statistical software (SPSS, v.16, SPSS Inc., Chicago, IL) was used for data analysis.
Results
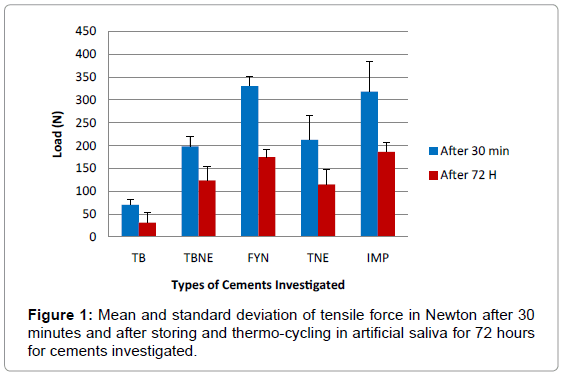
Mean and standard deviation of tensile forces required to pull cemented crowns from their implant abutments either after storing 30 minutes in dry condition or after storing and thermo-cycling for 72 hours to all cements are presented in (Table 2 and Figure 1).
| Materials | TB | TBNE | FYN | TNE | IMP |
| 30 minutes | 70.3 ± 12.4 | 198.5 ± 21.8 | 330.5 ± 20.7 | 212.7 ± 52.9 | 318.4 ± 64.8 |
| 72 hours | 31.5 ± 21.7 | 123.8 ± 31.4 | 174.6 ± 15.8 | 115.3 ± 31.6 | 186.6 ± 19.3 |
Table 2: Mean ± standard deviations of tensile force in Newton’s for all cements investigated after 30 minutes and after storing and thermo-cycling in artificial saliva for 72 hours (n=10).
Results showed that Temp Bond luting agent (Type I zinc oxide eugenol) exhibited the lowest mean tensile force after storing in dry condition for 30 minutes (70.3 N) and after storing and thermo-cycling in artificial saliva for 72 hours (31.5 N), while Fynal and ImProv luting agents showed the highest mean tensile bond strength in dry condition (330.5 N) and after storing and thermo-cycling in artificial saliva for 72 hours (186.6 N), respectively.
Statistical analysis (Table 3) showed that there is significant difference between mean force of all cements investigated either after 30 minutes or after 72 hours of cementation. Storing and thermocycling of specimens in artificial saliva solution for 72 hours caused a significant reduction in the retentive force values.
| Cement | Sum of Squares | df | Mean Square | F value | P value |
| Model | 845770.56 | 9 | 93974.507 | 84.359 | 0.000 |
| Cement | 554528.86 | 4 | 138632.215 | 124.447 | 0.000 |
| Storage | 248601.96 | 1 | 248601.960 | 223.165 | 0.000 |
| Cement × Storage | 42639.74 | 4 | 10659.935 | 9.569 | 0.000 |
| Error | 100258.6 | 90 | 1113.984 | ||
| Total | 4051378.0 | 100 | |||
| Corrected Total | 94629.16 | 99 |
Table 3: P values of two-way ANOVA for tensile force in Newton of cements investigated after 30 minutes and after storing and thermo-cycling in artificial saliva for 72 hours.
For Temp Bond luting agent 3 specimens were deboned after thermo-cycling and the load were recorded for them as zero. This may explain high standard deviation of the load of that cement.
The nature of the retentive failures was adhesive in all luting agents investigated. It was consistently found at the abutment-cement interface with the cement remnants attached to the casting.
Discussion
Implant supported fixed partial dentures may be cemented to abutments with a provisional luting agent to enable removal of the restorations. The tensile bond strength of the luting agent must be great enough to resist lateral and vertical forces during function. The taper, surface area and texture of preparations affect the retention of the casting [14]. In this study, these factors were the same for all specimens investigated. Repeated cementation of dental castings has been shown that it did not significantly affect the tensile bond strength of luting agents [15] Breeding et al. [2] compared tensile bond strengths of three dental luting agents after cementing casted restorations to both human teeth and machined titanium implant abutments and reported no significant differences between retentive values for the natural abutments and the machined metal implant abutments for any of the luting agents tested.
With regard to potential retrievability of cement-retained implant restorations, the retentive strength of the luting agents is critical. Nejatidanesh et al. [11] evaluated the retention values of implant-supported metal copings using different luting agents. They concluded that the resin modified glass ionomer; zinc phosphate, zinc polycarboxylate, and Panavia F had statistically the same retentive quality and are recommended for definitive cementation of single implant-supported restorations. The provisional cements and glass ionomer may allow retrievability of these restorations.
In an in vivo study, Singer and Serfaty [1] reported success when implant-supported cast restorations were retained with provisional luting agents. Retrievability of the cast restoration is desirable if intervention therapy is required and for the maintenance of the supporting tissues and implants. The use of either a provisional luting agent or screw should allow retrievability; however, a provisional luting agent should eliminate problems noted with screw-retained prostheses. When a cemented superstructure is used, conventional prosthodontic procedures may be completed in both the laboratory and clinical phases of restorative treatment. Tensile bond strength of permanent dental luting agents, such as zinc phosphate and glass ionomer, has been reported with both natural abutments and implant abutments. However, published bond strength data for provisional luring agents used with cast restorations cemented to implant abutments are limited. The tensile strength of the luting agent should allow retrievability when required, yet be sufficient to retain the prostheses during function.
In the present study results showed that Fynal (polymer modified zinc oxide eugenol) and ImProv (polyurethane) luting agents showed the highest retentive values in the 30 minute group without significant difference between them. Their relative high retentive values may be related to their higher compressive strength.
Our results showed that thermo-cycling caused a significant reduction in the retentive values of all provisional luting agents investigated. This is in agreements with the results obtained by Michalakis et al. [16] and Kokubo et al. [17]. Michalakis et al. [16] concluded that thermal cycling had a detrimental effect on the retentive properties of all cements investigated. Also Kokubo et al. [17] stated that the retentive force of TempBond NE decreased significantly after thermal cycling. They concluded that TempBond NE may not be appropriate for the retention of single-tooth zirconia abutments and coping restorations. This is in agreement of our results as TempBond and TempBond NE had the lowest retentive load. Also Ramp et al. [18] found that Tem Bond and Provilink luting agents exhibited the lowest mean tensile bond strengths, while Neo Temp luting agent exhibited tensile bond strength more than three times that of Temp Bond luting agent.
Analysis of results demonstrated that variances of retentive loads between the different luting agents investigated. This may be due to the high standard deviations in some groups. The high standard deviation of Temp Bond luting agent after thermocycling was due to failure of three specimens and load was recorded for them as 0 loads. Some previous studies concerning cement retention have showed similar high standard deviations [2,19,20].
Nejatidanesh et al. [21] evaluated the retention value of implantsupported zirconium oxide ceramic copings using different luting agents. They concluded that the retention of zircona ceramic restorations, over ITI solid abutments may be influenced by the type of cement. Michalakis et al. [22] evaluated the failure loads of four provisional luting agents used for the cementation of FPDs supported by 2 implants or 4 implants. Nogenol luting agent exhibited the lowest retentive values in both types of FPD while ImProv was the most retentive cement of all cements tested. This is in agreement with our results. They found also that Temp Bond NE and Temp Bond presented significantly different values (P<.05) for the 2-implant prostheses but not for the 4-implant model [22].
Our paper rank the tensile bond of provisional luting agents investigated just after cementation and also after storing and thermocycling in artificial saliva resembling the conditions in vivo. This enables clinicians to select the suitable type of cement according to what they need.
Conclusions
Under the limitation of our study, it was concluded that:
1. There is significant difference between means of retentive forces of provisional cements investigated.
2. Temp Bond luting agent exhibited the lowest mean tensile bond strength.
3. Final and ImProv luting agents showed the highest mean tensile bond strength.
4. Storing and thermo-cycling of the specimens in artificial saliva for 72 hours caused a significant reduction in the retentive values of most provisional luting agents used.
5. Our results provide a ranking order of the different luting cement according to their ability to retain implant restorations.
6. The results may help the clinician for selecting luting agent, retentive enough to withstand occlusal forces, yet weak enough to allow easy retrieval of cement-retained fixed restorations.
7. The nature of the retentive failures was adhesive in all luting agents which found at the abutment-cement interface with the cement remnants attached to the casting.
References
- Singer A, Serfaty V (1996) Cement-retained implant-supported fixed partial dentures: a 6-month to 3-year follow-up. Int J Oral Maxillofac Implants 11: 645-649.
- Breeding LC, Dixon DL, Bogacki MT, Tietge JD (1992) Use of luting agents with an implant system: Part I. J Prosthet Dent 68: 737-741.
- Block MS and Kent JN (1995) Endosseous implants for maxillofacial reconstruction. pp. (l97-200) W.B Saunders Comp Philadelphia.
- Chiche GJ, Pinault A (1991) Considerations for fabrication of implant-supported posterior restorations. Int J Prosthodont 4: 37-44.
- Ganor Y, Indig B, Gross M (1996) Retrievable cemented crown options on implant-supported angled abutments: a case report. Quintessence Int 27: 679-684.
- Hebel KS, Gajjar RC (1997) Cement-retained versus screw-retained implant restorations: achieving optimal occlusion and esthetics in implant dentistry. J Prosthet Dent 77: 28-35.
- Rosenberg MM, Kay HB, Keough BE, Holt RJ (1988) Periodontal management for advanced cases. Chicago, Quintessence, 401-405.
- Carter GM, Hunter KM, Herbison P (1997) Factors influencing the retention of cemented implant-supported crowns. N Z Dent J 93: 36-38.
- Schiessl C, Schaefer L, Winter C, Fuerst J, Rosentritt M, et al. (2013) Factors determining the retentiveness of luting agents used with metal- and ceramic-based implant components. Clin Oral Investig 17: 1179-1190.
- McGlumphy EA, Papazoglou E, Riley RL (1992) The combination implant crown: a cement- and screw-retained restoration. Compendium 13.
- Nejatidanesh F, Savabi O, Ebrahimi M, Savabi G (2012) Retentiveness of implant-supported metal copings using different luting agents. Dent Res J (Isfahan) 9: 13-18.
- Chee WW, Torbati A, Albouy JP (1998) Retrievable cemented implant restorations. J Prosthodont 7: 120-125.
- Lepe X, Bales DJ, Johnson GH (1999) Retention of provisional crowns fabricated from two materials with the use of four temporary cements. J Prosthet Dent 81: 469-475.
- Shillingburg HT, Sather DA, Wilson EL, Cain JR, Mitchell DL, et al. (2013) Fundamentals of fixed prosthodontics, Quintessence Pub Co (4th edn), Chicago.
- Felton DA, Kanoy BE, White JT (1987) Recementation of dental castings with zinc phosphate cement: effect on cement bond strength. J Prosthet Dent 58: 579-583.
- Michalakis K, Pissiotis AL, Kang K, Hirayama H, Garefis PD, et al. (2007) The effect of thermal cycling and air abrasion on cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants 22: 569-574.
- Kokubo Y, Kano T, Tsumita M, Sakurai S, Itayama A, et al. (2010) Retention of zirconia copings on zirconia implant abutments cemented with provisional luting agents. J Oral Rehabil 37: 48-53.
- Ramp MH, Dixon DL, Ramp LC, Breeding LC, Barber LL (1999) Tensile bond strengths of provisional luting agents used with an implant system. J Prosthet Dent 81: 510-514.
- Baldissara P, Comin G, Martone F, Scotti R (1998) Comparative study of the marginal microleakage of six cements in fixed provisional crowns. J Prosthet Dent 80: 417-422.
- Hunsaker KJ, Christensen GJ, Christensen RP, Cao D, Lewis RG (1993) Retentive characteristics of dental cementation materials. Gen Dent 41 Spec No: 464-467.
- Nejatidanesh F, Savabi O, Shahtoosi M (2013) Retention of implant-supported zirconium oxide ceramic restorations using different luting agents. Clin Oral Implants Res 24 Suppl A100: 20-24.
- Michalakis KX, Pissiotis AL, Hirayama H (2000) Cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures. Int J Oral Maxillofac Implants 15: 545-549.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 16901
- [From(publication date):
September-2013 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12084
- PDF downloads : 4817