Case Report Open Access
Restoring Smiles for the Young: Aesthetic and Functional Rehabilitation of 3 Year Old Children with Early Childhood Caries: Case Reports
Saini Sheeba1*, Sharma Deepak1 and Chopra Sumit21Department of Pediatric Dentistry, M. M. College of Dental Sciences and Research, Mullana, (Ambala), India
2Department of Oral and Maxillofacial Surgery M. M. College of Dental Sciences and Research, Mullana, (Ambala), India
- Corresponding Author:
- Dr. Sheeba Saini
Reader Pedodontics and Preventive dentistry
Himachal Institute of Dental Sciences and Research
Ponta Sahib, Himachal Pradesh, India
Tel: +91-9458960045
E-mail: sheeba888@gmail.com
Received date September 16, 2014; Accepted date October 13, 2014; Published date October 17, 2014
Citation: Sheeba S, Deepak S, Sumit C (2014) Restoring Smiles for the Young: Aesthetic and Functional Rehabilitation of 3 Year Old Children with Early Childhood Caries: Case Reports. J Interdiscipl Med Dent Sci 2:155. doi: 10.4172/2376-032X.1000155
Copyright: © 2014 Sheeba S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Early childhood caries results in early pulp involvement and gross destruction of the anterior and posterior teeth. This leads to decreased masticatory efficiency, difficulty in speech, compromised esthetics, development of abnormal tongue habits and subsequent malocclusion and psychological problems. The restoration of severely decayed deciduous teeth especially anteriors presents a special challenge to dentists, particularly in uncooperative children. The following case reports document the restoration of severely mutilated deciduous teeth in two emotionally immature patients resulting in an improvement in not only their oral and general health but also helping them gain self-confidence.
Keywords
Childhood caries; Abnormal tongue habits; Malocclusion; Deciduous teeth
Introduction
Early childhood caries (ECC) is a disease that involves development of one or more carious lesions, with or without cavitation, by the age of 71 months [1]. Epidemiological studies have indicated that ECC has a strong social element [2-4]. Indeed, higher prevalence in nondeveloped countries [5,6] and in socioeconomically disadvantaged groups living in low, middle [2-4] and high-income countries [7,8] have been documented.
In general, the prevalence of caries in preschool children is declining or has reached a plateau in most of the developed countries [9,10], but the same may be increasing in some developed and several developing countries [11,12]. In Asia, in the Far East region, the prevalence in threeyear- olds ranges from 36 to 85% [13-18] while in India a prevalence of 44% has been reported for caries in 8- to 48-month-old children [19].
The etiology of the disease is multifactorial. In developed countries the primary risk factor is considered to be the use of a nap time bottle that contains a fermentable carbohydrate such as milk with sugar, sweetened milk formula, fruit juice, or other sweetened solutions [20], whereas in developing countries along with the above stated other factors such as linear enamel hypoplasia of primary teeth associated with malnutrition may also contribute to the prevalence of this condition [21]. Complex interaction between the use of sweetened pacifiers, nursing on demand, neglected oral hygiene, Streptococcus mutans, maternal education and dental knowledge, family structure and social status make its etiology complex.
ECC is associated with significant adverse physical, functional, and behavioral consequences. The disease implications are high risk of new caries defects in both permanent and deciduous dentitions, insufficient physical development, hospitalization and emergency room visits, loss of school days and increased days of restricted activity, increased treatment costs and time, diminished ability to learn, and diminished oral health-related quality of life [22]. Due to the aggressive pattern of the disease, treatment should be specific for each individual patient, and should be given by a specialist who can manage the young child and the process of the disease [22]. Treatment options are: 1. Conservative approach which includes recalls and topical fluoride 2. Aggressive restorative approach. In both one should first stop the carious process and encourage prevention. To choose the type of treatment, one should consider the severity of the lesions, child's age, caries risk, child's behavior, and parents' cooperation and socioeconomic status [22].
Full mouth rehabilitation including the esthetic restoration of severely mutilated primary anterior teeth has always been a challenge for the dentist for a long time, not only because of the limitations of the available materials and techniques but also because the children who require such restorations are usually among the youngest and least manageable group of patients. Most clinicians prefer to treat the emotionally immature children under general anesthesia. Treatment under general anesthesia has its own risks and limitations. The treatment is expensive and out of reach for most of the middle and low socioeconomic status children. It is also associated with a huge range of risks and difficulties [23]. It is unpleasant for the child as well as for the parents.
The following case reports describe the challenging task of treating two 3 year-old patients suffering from early childhood caries presenting with multiple mutilated teeth. Both the children had a Frankel behavior rating of definitely negative (Table 1) [24,25], but were managed using only voice control and other non-pharmacological behavior management techniques. The children were dealt with an extra ordinary amount of patience and hence required multiple sittings. At the end of treatment they walked out of the operatory not only with their oral problems solved but also as stronger and more confident individuals with a positive attitude towards dental treatment developed for life.
Case I
| Rating | Description |
|---|---|
| Definitely Negative | Refusal of treatment, crying forcefully, fearful, or any other overt evidence of extreme negativism |
| Negative | Reluctant to accept treatment, uncooperative, some evidence of negative attitude but not pronounced, sullen, withdrawn |
| Positive | Acceptance of treatment, at times cautious, willingness to comply with the dentist, at times with reservation but patient follows the dentist's directions cooperatively |
| Definitely Positive | Good rapport with the dentist, interested in the dental procedures, laughing and enjoying the situation |
Table 1: Frankle 4-Point Behaviour Rating Index
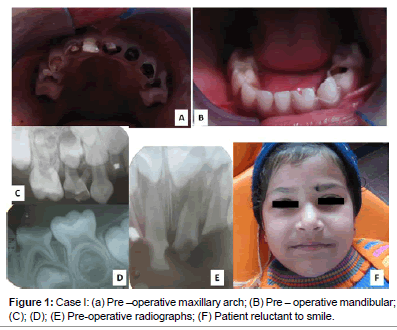
A 3-year-old female patient reported to the Dept. of Pediatric Dentistry, MM College of Dental Sciences and Research, with a complaint of severely decayed teeth. The child was emotionally immature and highly uncooperative. Intraoral examination revealed multiple carious lesions, with 54,53,52,51, 61, 62, 63, 64, and 74 showing pulp involvement. Crown portions of maxillary incisors were grossly destructed (Figures 1-6).
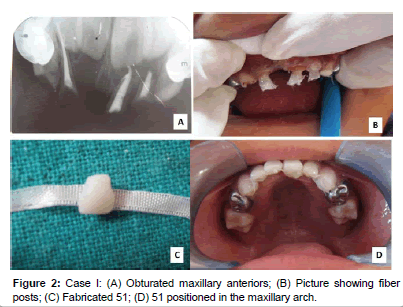
It was decided to extract 51 and pulpectomize 54,53,52,61, 62, 63 and 64.74 were posted for pulpotomy. Post and core and strip crown was planned for 52, 61and 62. The posterior teeth (54, 64 and 74) were restored with stainless steel crowns. For the 51space an esthetic fixed functional space maintainer was planned.
Treatment was carried out in multiple sittings as per the standard norms. Pulpectomy followed by composite restoration (strip crown) and custom-made posts were performed. For core build up in deciduous anterior teeth, about 4 mm of cement was removed from the coronal end of the root canal, and 1 mm of glass ionomer cement was placed. A fiber reinforced composite post was fabricated and cemented with composite in 52,61,62. The incisal end of the post projected 2-3 mm above the remaining tooth structure. The composite was light cured for 40 seconds. A strip crown was used to reconstruct the crown.
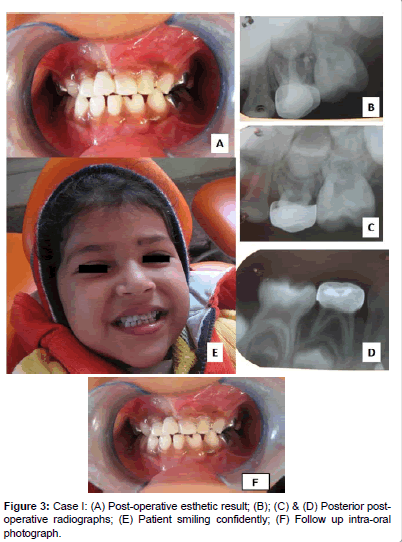
This provided good mechanical retention and support for the restorative material. Coronal tooth structure of 51 was fabricated using composite resin and fixed in place to the adjacent 52, 61, 62 and 63 using composite resin and fiber splint. The occlusion was checked and final finishing and polishing of the restoration was performed using soflex tips. The pulp treated posterior teeth were followed by a stainless steel crown. After completion of the procedure, post-operative photographs and radiographs were taken. Home care instructions, including oral hygiene measures and diet counseling, were given to the parents. Recall checkup was scheduled after every 6 months to assess the maintenance.
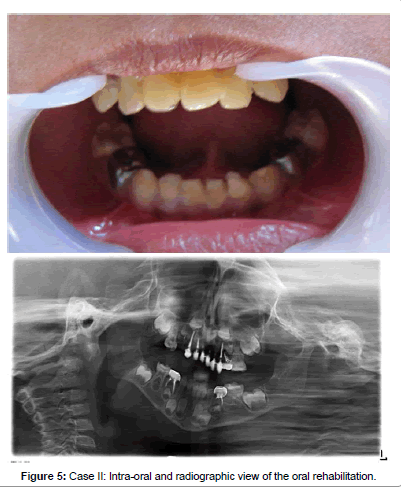
Case II
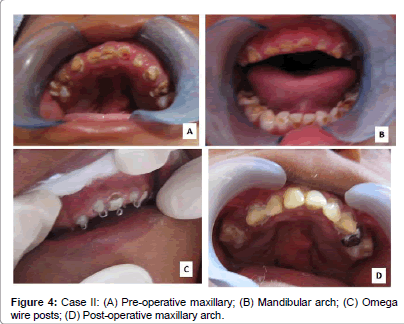
A 3-year-old male patient reported to the Department of Pediatric Dentistry, complaining of pain in severely decayed teeth. The highly uncooperative child had a subnormal IQ was and underweight because of long term inability to eat as most of the teeth were grossly destructed and painful. History revealed that the patient was on blood transfusions for treatment of severe anemia.
Intraoral examination revealed a cleft palate and multiple carious lesions, with pulpal involvement in 54, 53, 52, 51, 61, 62, 63, 64, 74, 84. Crowns of the carious maxillary teeth were grossly destructed. It was decided to do pulpectomy in 54, 53, 52, 51, 61, 62, 63, 64, 74, 84 followed by post and core and strip crown in 53, 52, 51, 61, 62 and 63. 64, 74 and 84 were planned to be restored with stainless steel crowns. 54 could not be crowned as the crown structure was insufficient. It was decided to retain the obturated root stumps of 54 to serve as a passive space maintainer. The other carious teeth with no pulpal involvement were planned to be restored with resin reinforced glass ionomer cement.
Pulpectomy followed by composite restoration (strip crown) using custom-made posts, were performed in the maxillary anteriors along with the other required treatments. For building core in the deciduous anterior teeth, about 4 mm of cement was removed from the coronal end of the root canal, and 1 mm of glass ionomer cement was placed. A 0.7-mm stainless steel orthodontic wire was bent using no. 130 orthodontic pliers into an omega loop so as to allow the ends to be engaged at the entrance of the root canal. The incisal end of the loop of the wire projected 2-3 mm above the remaining structure. The loop was inserted into the canal with composite. The composite was light cured for 40 seconds. A strip crown was used to reconstruct the crown.
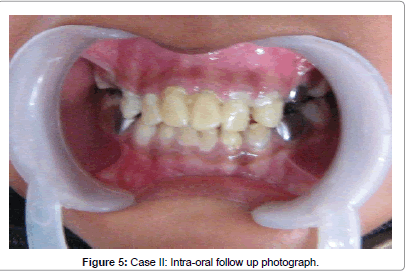
The occlusion was checked, and after the removal of interferences, final finishing and polishing of the restoration was performed using soflex tips. After completion of the procedure, post-operative photographs and Orthopantomogram were shot. Home care instructions and diet counseling, were given to the parents. Recall checkups were performed every 6 months.
On follow-up visits it was observed that apart from the dental benefits the child also became more confident socially. As no general anesthesia was used the child got over his dental fear and learnt to accept dental treatment. The general health of the child improved as indicated by an improvement in the hemoglobin level and a gain in body weight.
Discussion
Dental treatment of immature uncooperative children has always been a challenge. General anesthesia is used for such children, but is an expensive alternative. It is also associated with adverse events and unpleasant side effects. An important consideration for children who are unable to cooperate due to fear, anxiety or young age is their subsequent acceptance of care using other methods with low risk and low impact as general anesthesia does not shape the behavior of a child [26]. Therefore in the presented cases an effort was made by the authors to manage the children without anesthesia or sedation.
In the presented cases, custom-made posts were used in anterior teeth; other available options such as nickel-chromium cast posts, preformed and cast metal posts were not considered they are expensive and require additional lab work. The use of metal posts needs the use of an opaque resin to mask the unaesthetic post and also poses additional problems during the course of natural exfoliation [27].
An esthetic option for such cases is a biologic post. The disadvantage of this technique is acceptance and stringent infection control policies.
Available literature shows that intra-canal retention in primary teeth can be obtained by directly building resin composite posts or preparing an "inverted mushroom-shaped" undercut in the root canal prior to the buildup of the resin [28]. However, resin composite posts have low strength of loading. Previous studies concluded that fiber reinforced composite resin posts show higher strength, retention and marginal adaptation [29], this led the authors to use the said material in case I. However the high cost of glass fiber reinforced composite resin post limits its use. In the second case considering the socioeconomic status of the patient a custom-made post using an orthodontic wire followed by strip crowns was used. Literature reveals that this achieves satisfactory results in a child patient [30,31]. However, it is technique sensitive and requires parent's cooperation. Also there is a chance of loss of restoration due to trauma or biting on hard food, so the parents were instructed to teach the child to avoid hard food.
Both the children were very happy and satisfied with the functional and esthetic results, viz., mastication, speech, cosmetic function, etc. Restorations were found to be serving well at the 1 year recall appointment.
In this study, authors take the view that full-mouth rehabilitation without GA can enable children to cope with future dental care and leave them in a position where they may be more amenable to dental care. A child benefits from oral rehabilitation in more than one way. Apart from the dental benefits, oral rehabilitation also contributes towards improvement of general and psychological well-being as was seen in case II.
References
- AAPD: Definition of Early Childhood Caries (ECC) Classifications, consequences, and preventive strategies. Pediatr Dent 2004, 25: 31-32.
- Hallett KB, O'Rourke PK (2006) Pattern and severity of early childhood caries.Community Dent Oral Epidemiol 34: 25-35.
- Livny A, Assali R, Sgan-Cohen HD (2007) Early Childhood Caries among a Bedouin community residing in the eastern outskirts of Jerusalem.BMC Public Health 7: 167.
- Mohebbi SZ, Virtanen JI, Vahid-Golpayegani M, Vehkalahti MM (2008) Feeding habits as determinants of early childhood caries in a population where prolonged breastfeeding is the norm.Community Dent Oral Epidemiol 36: 363-369.
- Reisine S, Douglass JM (1998) Psychosocial and behavioral issues in early childhood caries.Community Dent Oral Epidemiol 26: 32-44.
- Prakash P, Subramaniam P, Durgesh BH, Konde S (2012) Prevalence of early childhood caries and associated risk factors in preschool children of urban Bangalore, India: A cross-sectional study.Eur J Dent 6: 141-152.
- Stecksén-Blicks C, Borssén E (1999) Dental caries, sugar-eating habits and toothbrushing in groups of 4-year-old children 1967-1997 in the city of Umeå, Sweden.Caries Res 33: 409-414.
- Tomar SL, Reeves AF (2009) Changes in the oral health of US children and adolescents and dental public health infrastructure since the release of the Healthy People 2010 Objectives.AcadPediatr 9: 388-395.
- Nordblad A, Souminen-Taipale L, Rasilainen J, Karhunen T,Suunterveydenhuoltoaterveyskeskuksissa 1970-luvulta vuoteen 2000 (Oral Health Care at Health Centers from the 1970s to the year 2000), Report 278, National Research and Development Center for Welfare and Health (STAKES),Helsinki, Finland.
- Holm AK (1990) Caries in the preschool child: international trends.J Dent 18: 291-295.
- Oral health improving for most Americans, but tooth decay among preschool children on the rise (2007) Center for Disease Control (CDC). Centers for Disease Control and Prevention 2007-1698.
- Pitts NB, Palmer JD (1995)The dental caries experience of 5-year-old children in Great Britain. Surveys coordinated by the British Association for the Study of Community Dentistry in 1993/94. Community Dent Health 12:52-58
- Tsai AI, Chen CY, Li LA, Hsiang CL, Hsu KH (2006) Risk indicators for early childhood caries in Taiwan.Community Dent Oral Epidemiol 34: 437-445.
- Cariño KM, Shinada K, Kawaguchi Y (2003) Early childhood caries in northern Philippines.Community Dent Oral Epidemiol 31: 81-89.
- Jin BH, Ma DS, Moon HS, Paik DI, Hahn SH, et al. (2003) Early childhood caries: prevalence and risk factors in Seoul, Korea.J Public Health Dent 63: 183-188.
- Douglass JM, Wei Y, Zhang BX, Tinanoff N (1995) Caries prevalence and patterns in 3-6-year-old Beijing children.Community Dent Oral Epidemiol 23: 340-343.
- Mayanagi H, Saito T, Kamiyama K (1995) Cross-sectional comparisons of caries time trends in nursery school children in Sendai, Japan.Community Dent Oral Epidemiol 23: 344-349.
- Fujiwara T, Sasada E, Mima N, Ooshima T (1991) Caries prevalence and salivary mutans streptococci in 0-2-year-old children of Japan.Community Dent Oral Epidemiol 19: 151-154.
- Jose B1, King NM (2003) Early childhood caries lesions in preschool children in Kerala, India.Pediatr Dent 25: 594-600.
- Ribeiro NM, Ribeiro MA (2004) [Breastfeeding and early childhood caries: a critical review].J Pediatr (Rio J) 80: S199-210.
- Oliveira AF, Chaves AM, Rosenblatt A (2006) The influence of enamel defects on the development of early childhood caries in a population with low socioeconomic status: a longitudinal study.Caries Res 40: 296-302.
- Nissan S, Khoury-Absawi M (2009) [Early childhood caries].RefuatHapehVehashinayim 26: 29-38, 70.
- Cravero JP, Blike GT (2004) Review of pediatric sedation.AnesthAnalg 99: 1355-1364.
- McMillan S (1982) Behavior of children and adolescents. In: Pediatric Dentistry- Scientific foundations and clinical practice (1stedn) Stewart RE, Barber TK, Troutman KC and Wei SHY. Mosby, St. Louis, USA. p152.
- Wright GZ, Stigers JI (2011)Nonpharmacologic management of children's behaviors. In: McDonald and Avery Dentistry for the Child and Adolescence (9thedn) Mosby, St. Louis, USA. p27-40.
- Harrison MG, Roberts GJ (1998) Comprehensive dental treatment of healthy and chronically sick children under intubation general anaesthesia during a 5-year period.Br Dent J 184: 503-506.
- Mortada A, King NM (2004) A simplified technique for the restoration of severely mutilated primary anterior teeth.J ClinPediatr Dent 28: 187-192.
- Rifkin AJ (1983) Composite post-crowns in anterior primary teeth.J Dent Assoc S Afr 38: 225-227.
- Sharaf AA (2002) The application of fiber core posts in restoring badly destroyed primary incisors.J ClinPediatr Dent 26: 217-224.
- Usha M, Deepak V, Venkat S, Gargi M (2007) Treatment of severely mutilated incisors: a challenge to the pedodontist.J Indian SocPedodPrev Dent 25 Suppl: S34-36.
- Aminabadi NA, Farahani RM (2009) The efficacy of a modified omega wire extension for the treatment of severely damaged primary anterior teeth.J ClinPediatr Dent 33: 283-288.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 15814
- [From(publication date):
December-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11125
- PDF downloads : 4689