Response Preparedness to Viral Hemorrhagic Fever in Nigeria: Risk Perception, Attitude towards Lassa Fever
Received: 04-Aug-2015 / Accepted Date: 10-Sep-2015 / Published Date: 18-Sep-2015 DOI: 10.4172/2161-1165.1000199
Abstract
Objectives: The objective of the study was to determine the knowledge, attitude, and practices towards Lassa fever of tertiary health workers.
Setting: Two Federal Teaching Hospitals in Nigeria.
Participants: Doctors, nurses, laboratory scientists, health educator, environmental health officers, mortuary attendants, cleaners, pharmacists, physiotherapists, and health technicians.
Primary and secondary outcome measures: A cross-sectional study was conducted using a standardized, self-administered questionnaire, which enquired about the risk perception, knowledge, attitude, and health-seeking behavior towards Lassa fever.
Results: Risk perception among participants was fairly good, while compliance with universal precautions amongst these highly exposed populations should be improved.
Conclusions: Training on Lassa fever should be paired with appropriate and corresponding training on personal protective equipment.
Trial Registration: Not applicable.
Keywords: Lassa fever; KAP; Health workers; Nigeria
163805Introduction
Lassa fever (LF) is an acute viral illness endemic to several countries in West Africa. Lassa virus (LASV) is a zoonotic, rodent-borne, single-stranded ribonucleic acid (RNA) virus from the Arenaviridae virus family. The natural reservoir of the Lassa virus, a ‘multimammate rat’, Mastomys natalensis [1]. Mastomys spp. produce large numbers of offspring, and are abundant in the savannah and forests of West, Central and East Africa. They readily colonize human homes, thus increasing the risk of LASV spread from infected rats to humans. Although LASV was first isolated in 1969 from a missionary nurse working in Lassa town of Borno State in North-Eastern Nigeria, LF seems to have been described as early as the 1950’s in Guinea, West Africa [2,3]. LF is also highly endemic in other West African countries including Sierra Leone, Liberia, and Guinea [4,5] As such, the prevalence of LASV antibodies in the general population is 8-52% in Sierra Leone, [6] 4-55% in Guinea, [6] and 21% in Nigeria [7]. In the early phases of the disease, LF symptoms are similar to those of many other common febrile illnesses such as flu, malaria or typhoid; as such, misdiagnosis is a common problem in the early stages of an outbreak. While LF is mild or has no observable symptoms in about 80% of people infected with the virus, the remaining 20% develop a severe multisystem disease [7,8]. During LF outbreaks, the case-fatality rate can reach as high as 50% [8-11]. LF has an overall fatality rate of 1-2%; much lower than the fatality rate of 9.3% to 18% seen among all hospital admissions [11]. LF continues to be major public health concern in Nigeria, Liberia, Sierra Leone and Guinea, as it is among the largest burden of viral hemorrhagic fevers in West Africa after Yellow Fever and the 2014 Ebola Viral Disease outbreak [9,10]. The populations at risk in Sierra Leone, Guinea, and Nigeria may be as high as 59 million, with an annual incidence of illness of 3 million, and mortality as high as 67,000 [1,11]. LASV has been associated with nosocomial outbreaks with high mortality, [12] and LF cases have been “exported” into the United States of America and Europe by viremic travelers from endemic areas [13]. The increasing LF incidence outside endemic regions, due in part to the increased frequency of international travel, necessitates that health care providers, who are at the highest risk for infection because of their frequent contact with infected patients and their blood or bodily fluids, have comprehensive information on LASV infection.
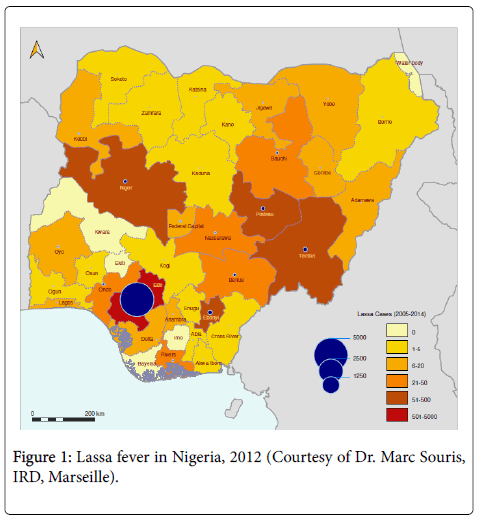
The large population at risk in West Africa and the limited surveillance and laboratory support for rapid diagnostics has prompted this study. The objective of the study was to determine the risk perception, knowledge, attitude and health-seeking behavior among tertiary health workers towards Lassa fever in the main hospitals situated in the LF endemic area, including the Federal Teaching Hospital Abakaliki, Ebonyi State and, Institute of Lassa Fever Diagnostic Centre and Research laboratory, Irrua Specialist Teaching Hospital, Edo State. LF is endemic in Edo, Nasarawa, Ebonyi and Plateau States. As of October 2012, LF has been reported in 23 of the 36 states including Federal Capital Territory (FCT), and 42 Local Government Areas (LGAs) reported LF cases across the country. Health workers are a high-risk population for exposure when working with LF patients or samples.
Nigeria witnessed an outbreak of Lassa fever in the year 2012 with 1,723 cases, 112 deaths, 201 laboratory-confirmed cases, and a case-fatality rate of 6.50. During the outbreak, six Nigerian tertiary health workers (three doctors and three nurses) lost their lives while managing LASV infected patients.
This study seeks to build upon the existing body of knowledge, attitudes, and practices toward Lassa fever in Nigeria. A previous study compared knowledge, attitudes, and practices between two hospitals within a single State [14]; this study makes the comparison between two hospitals that are from different States, but are within the epidemic zone of LF.
Study Population, Sites and Methods
Population and site
Cases have been previously and still are, reported in Ebonyi and Edo states, thus prompting the present study in these endemic states and among health workers (the most exposed population) of the two major teaching hospitals, which are referring for LF at the national level. The study population consisted of health workers, with ages ranging from 15 to 50 years old. The study was conducted from May to July 2013 at Federal University Teaching Hospital of Abakaliki, Ebonyi State and at Irrua Specialist Teaching Hospital of Irrua, Edo State (Figure 1).
Methods
The study was a descriptive cross-sectional study on the risk perception, knowledge, attitude and health seeking behavior of tertiary health workers towards LF in order to: assess the tertiary health workers’ knowledge of the causes, symptoms and signs and mode of transmission of LF; determine the health workers’ level of knowledge on the prevention of LF in the hospital; assess the attitude of health workers to LF and potentially infected patients; verify the risk perception as shown by the health seeking behavior of health workers who may be exposed.
Data collection and analysis
A cross-sectional study was performed, and a total of 326 questionnaires were administered. The survey included questions on the demographics for the survey participants, knowledge of Lassa fever, and occupational-specific knowledge on the treatment and prevention of Lassa fever infections. The sampling frame was comprised from the list of 23 tertiary institutions within the LF at-risk states. Two tertiary health facilities were judgmentally selected, from which 324 persons were selected, 162 from each. These samples were selected using population-weighted ratio of each of the two localities. A stratified sampling method was applied to select departments in those two health facilities from which the samples were taken. The various departments of the health institutions formed the strata, and the sample of 162 was allocated across the strata proportionally. A semi-structured questionnaire with both open/close-ended questions was used.
Ethics
Ethical approval for the study was obtained from the Ethics Committee of the University of Nigeria Enugu Campus, Abakaliki Federal University Teaching Hospital, Ebonyi State and Irrua Specialist Teaching Hospital, Irrua Edo State. Informed consent was obtained from each participant before enrolling him/her into the study. Investigators conducted the interviews in English, Hausa, Yoruba, and Igbo languages, as applicable to each respondent. Interviews were conducted in the work place of the respondents. Confidentiality assurance was given, and the questionnaire was anonymous. The interview was self-administered.
Data analysis
The questionnaires were collated, and data fed into the computer and analyzed using Statistical Programme for Social Sciences (SPSS Version 17).
Results
Almost all of the health workers surveyed (98.8%) were aware of LF as a infectious disease. Many of the surveyed respondents (89.8%) knew the correct definition of LF. 81.8% (265/324) of health workers surveyed got their information about LF from the community. Most of the survey respondents knew at least one of the major signs or symptoms of LF and identified Ribavirin as the most frequently used treatment for LF (Table 1).
| Knowledge (n=324) | Frequency (%) | |
|---|---|---|
| Awareness of Lassa fever | 320 (98.8) | |
| Correct definition of Lassa fever | 291 (89.8) | |
| Source(s) of knowledge | Community | 265 (81.8) |
| School | 220 (67.9) | |
| Media* | 134 (41.4) | |
| Hospital/MoH | 53 (16.4) | |
| Common signs and symptoms | Fever | 310 (95.7) |
| Headache | 296 (91.4) | |
| Weakness | 273 (84.3) | |
| Bleeding | 256 (79.0) | |
| Vomiting | 252 (77.8) | |
| Malaise | 241 (74.4) | |
| Abdominal pain | 228 (70.4) | |
| Sore throat | 222 (68.5) | |
| Nausea | 214 (66.0) | |
| Dizziness | 211 (65.1) | |
| Chest pain | 191 (59.0) | |
| Diarrhea | 180 (55.6) | |
| Cough | 178 (54.9) | |
| Myalgia | 144 (44.4) | |
| Ribavirin treatment | 292 (90.1) | |
| *(Radio, TV or newspaper) | ||
Table 1: Knowledge of definition, clinical presentation and treatment of Lassa fever among the study population of health workers of the two Teaching Hospitals of Ebonyi and Irrua States, Nigeria (2013) (Note: survey participants were allowed to select multiple answers for some questions).
Most of the surveyed respondents (96.9%) knew that LASV could be transmitted from one person to another, while 98.8% of surveyed respondents knew that a species of rat was the animal that transmits LASV. Most of the surveyed respondents (97.5%) equally knew that LASV could also be transmitted through the urine of the rat. Most of the surveyed respondents (96.9%) knew that LASV could be transmitted from animal to man through food contaminated with the virus. 74.0% of the surveyed respondents falsely believed raw food products could be preferentially contaminated with the virus (Table 2).
| Knowledge of LASV transmission (n=324) | Frequency | |
|---|---|---|
| From one person to another | 314 (96.9) | |
| By rat to man | 320 (98.8) | |
| By urine of rat to man | 316 (97.5) | |
| From animal to man through | Food contaminated | 314 (96.9) |
| Animal bite | 75 (23.1) | |
| Cuts | 68 (21.0) | |
| Contact with soil | 37 (11.4) | |
| Type of food items that can be contaminated with the virus: | Raw food products | 240 (74.0) |
| Food products spread by the road side | 235 (72.5) | |
| Canned or bottled food | 94 (29.0) |
Table 2: Knowledge of transmission of LASV among the study population of health workers of the Teaching Hospitals of Ebonyi and Irrua States, Nigeria (2013) (Note: survey participants were allowed to select multiple answers for some questions).
Majority of the surveyed health workers (90.7%) had a positive attitude toward food in relation to LF. Also 86.1% of surveyed respondents knew that LF could kill if not reported to the health facility in good time. Only 4.0% of surveyed respondents had negative attitude to LF in relation to food (Table 3).
| Attitude (n=324) | Frequency (%) |
|---|---|
| Positive | |
| Raw and cooked food should be kept in closed containers | 294 (90.7) |
| Lassa fever can kill if not reported in good time | 270 (83.3) |
| Canned drinks should be washed before consumption | 179 (55.2) |
| Negative | |
| Food should be kept open | 17 (5.2) |
| Cassava and yam should be dried along the road | 13 (4.0) |
Table 3: Attitudes to food in relation to Lassa fever of Health workers of the Teaching Hospitals of Ebonyi and Irrua States, Nigeria (2013).
The study indicated that 97.5% of the health workers surveyed acknowledged that LF could be transmitted via contact with the urine of the Natal Multimammate mouse (Mastomys natalensis). 90.7% of surveyed respondents knew that raw and cooked food should be kept in closed containers.
Only 66.7% of surveyed respondents indicated that they always used personal protective equipment (PPE) when it was appropriate. The type of PPE used varied among survey participants: only 43.2% of them used coveralls (providing protection from splashes of blood, specimen, and other forms of contaminations), which is a major form of protection for health workers against infection by patients with highly infectious pathogens. Moreover, only 5.2% of surveyed participants indicated that they did not use the most commonly used PPE (gloves, face masks, aprons, boots, goggles, coveralls), which is a serious indication of exposure. Almost all surveyed respondents (92.3%) reported to health authorities for a proper medical check-up when exposed to a suspected case of LF (Table 4).
| Practice (n=324) | Frequency (%) |
|---|---|
| Use of personal protective equipment always | 216 (66.7) |
| Type of personal protective equipment used | |
| Gloves | 291 (89.8) |
| Face mask | 241 (74.3) |
| Apron | 205 (63.3) |
| Boots | 153 (47.2) |
| Goggle | 150 (46.3) |
| Coverall | 140 (43.2) |
| All of above | 108 (33.3) |
| None of above | 17 (5.2) |
| Action in case of exposure to suspected case of Lassa fever | |
| Report to health authority for medical check-up | 299 (92.2) |
| Self-medication | 11 (3.4) |
| Report to church/mosque/herbalist | 4 (1.2) |
| None of the above | 3 (0.9) |
Table 4: Practices of Lassa fever among the study population of health workers of the Teaching Hospitals of Ebonyi and Irrua States, Nigeria (2013) (Note: survey participants were allowed to select multiple answers for some questions).
Discussion
Only two health institutions from the six administrative zones were investigated, and thus may not be fully representative of the knowledge, attitudes, and practices of all health workers in Nigeria. However, these two institutions are located within the endemic zone for Lassa fever, so these results are circumstantial and pertinent to disease prevention and preparedness. Results were not weighted to adjust for biases inherent to proportionalities between larger and smaller departments within these hospitals. Results were not stratified by hospital, so comparisons between the two institutions were not performed. Analyses were restricted to bivariate comparisons; a more comprehensive, stratified understanding of how descriptive variables influence KAPs can be performed in future research, perhaps using multivariate regression.
A very high level of awareness (98.8%) towards LF was recorded among the surveyed health workers. This observation appears to be contrary to a previous finding of a similar 2005 study in Lagos that recorded a low level of awareness (21%) among study subjects [15]. Although the study population had a good knowledge of Lassa fever, there is a general, limited adherence to the universal standard precautionary measures that need to be taken for Lassa fever infection to be avoided amongst health workers in their various health facilities.
Most of the surveyed respondents had knowledge of the common signs and symptoms of LF; these results mirror those from other studies involving health workers [2,16-18]. Almost all (90.1%) of the surveyed respondents knew that Ribavirin is used to treat LF; this is significant because Ribaviran is currently the only treatment available.
The results showing that nearly all of the surveyed respondents (98.8%) knew that Lassa fever could be transmitted by a rat are similar to those in a previous study by Guinean researchers that emphasized the health workers’ belief that LF can kill if not reported in good time [19].
Since the first reported outbreak in Nigeria in 1969, it is well documented that Lassa fever kills a disproportionate number of health workers involved in the management and care of patients in hospital settings. Several health workers have lost their lives to LF at Irrua Specialist Teaching Hospital, prior to the establishment of the Institute of Lassa Fever Diagnostic and Research Laboratory.
Conclusions
This study has highlighted the risk perception, knowledge and attitude of health workers from two tertiary health institutions in Nigeria within the endemic zone for Lassa fever. Based on the findings of the present study, and the importance of the survival of public health workers working with VHFs, we suggest the following: training on Lassa fever for health workers should be paired with appropriate and corresponding training on personal protective equipment.
Standard precautions for Lassa fever are designed to prevent contact between the health care worker and infectious materials. Indeed, the same precautions are used for other highly infectious VHFs, such as Ebola Virus Disease (EVD), and have been promoted outside of those historical VHF endemic areas, which have been transgressed by EVD in West Africa since March 2014.
Authors Contributions
AD: Actively worked on generating field data and processing data in a common data base, developed the concept, did the data analysis, produce the figures and wrote the manuscript; EAN, TV, JPG: developed the concept, did the data analysis, produce the figures and wrote the manuscript. Marc Souris (French Institute of Research for Development) created the map of Lassa fever incidence.
Funding
Funding and consideration for this study was provided by the Nigerian Federal Ministry of Health.
References
- Kay RJ, Baglole DJ (2003) Lassa fever: epidemiology, clinical features, and social consequences. BMJ 29: 327:1271-5.
- Frame JD, Baldwin JM, Gocke DJ, Troup JM (1970) Lassa fever, a new virus disease of man from West Africa. 1. Clinical description and Pathological findings. Am J Trop Med Hyg 19: 670-676.
- Günther S, Emmerich P, Laue T, Kühle O, Asper M, et al. (2000) Imported lassa fever in Germany: molecular characterization of a new lassa virus strain. Emerg Infect Dis 6:466-76.
- Bowen MD, Rollin PE, Ksiazek TG,Hustad HL, Bausch DG, et al. (2000) Genetic diversity among Lassa virus strains. J Virol 74:6992-7004.
- Gonzalez JP, Emonet S, de LamballerieX, Charrel R (2007) Arenaviruses. Curr Top MicrobiolImmunol 315:253-88.
- Frame JD, Yalley-Ogunro JE, Hanson AP (1984) Endemic Lassa fever in Liberia. V. Distribution of Lassa virus activity in Liberia: Hospital staff surveys. Trans R Soc Trop Med Hyg 78:761-763.
- Ogbu O, Ajuluchukwu E, Uneke CJ (2007) Lassa fever in West African sub-region: an overview. J Vect Borne Dis44:1-11.
- Gershman MD, Staples JE (2015) Infectious Diseases Related to Travel: Yellow Fever. In: Brunette GW, edtn. CDC Health Information for International Travel. New York: Oxford: 78.
- Rainisch G, Shankar M, Wellman M, Merlin T, Meltzer MI (2015) Regional spread of Ebola virus, West Africa 2014. Emerg Infect Dis 21:444-7.
- Nadezhda EY, Walker DH (2012) Pathogenesis of Lassa Fever. Viruses 4:2031-2048.
- Fisher-Hoch SP, Tomori O, Nasidi A, Perez-Oronoz GI, Fakile Y, et al. (1995) Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practice. BMJ 311:857-9.
- Atkin S, Anaraki S, Gothard P, Walsh A, Brown D, et al. (2009) The first case of Lassa fever imported from Mali to the United Kingdom, February 2009. Euro Surveill 14(10).
- Tobin EA, Asogun DA, Isah EC, Ugege OG, Ebhodaghe P (2013) Assessment of knowledge and attitude towards Lassa fever among Primary care providers in an endemic suburban community community of Edo state: implications for control. J Med MedSci 4:311-318.
- Izegbu MC, Amole OO, Ajayi GO (2006) Attitudes, perception and practice of workers in laboratories in the two colleges of Medicine and their teaching hospitals in Lagos State, Nigeria as regards universal precaution measures. Biomedical Research 17: 49-54.
- Mertens PE, Patton R, Baum JJ, Monath TP (1973) Clinical presentation of Lassa fever cases during the hospital epidemic at Zorzor, Liberia, March-April 1972. Am J Trop Med Hyg 22:780-784.
- Fisher-Hoch S, McCormick JB, Sasso D, Carven RB (1988) Hematologic dysfunction in Lassa fever. J Med Virol 26:127-135.
- Monath TP, Maher M, Casals J, Kissling RE, Cacciapuoti (1974) Lassa fever in the Eastern Province of Sierra Leone, 1970-1972. II. Clinical observations and virological studies on selected hospital cases. Am J Trop Med Hyg 23:1140-1149.
- Fichet-Calvet E, Lecompte E, Koivogui L, Daffis s, terMeulen J (2008) Reproductive characteristics of Mastomysnatalensis and Lassa virus prevalence in Guinea, West Africa. Vector Borne Zoonotic Dis 8:41-8.
Citation: Adebayo D, Nwobi EA, Vincent T, Gonzalez JP (2015) Response Preparedness to Viral Hemorrhagic Fever in Nigeria: Risk Perception, Attitude towards Lassa fever. Epidemiology (sunnyvale) 5:199. DOI: 10.4172/2161-1165.1000199
Copyright: © 2015 Adebayo D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.