Research Article Open Access
Repeated Suicide Attempts in Emergency Room Psychiatric Referrals
Gramaglia C1, Bert F2*, Gattoni E1, Delicato C1, Di Marco S1, Coppola I1, Venesia A1, Marangon D3, Castello LM4, Avanzi GC4, Siliquini R2, Torre E1, Zeppegno P1,3
1Institute of Psychiatry, Department of Translational Medicine, Università del Piemonte Orientale, Via Solaroli n° 17, 28100, Novara, Italy
2Department of Public Health and Paediatric Sciences, Università degli Studi di Torino, Italy
3SC Psichiatria, AOU Maggiore della Carità, Corso Mazzini n° 18, 28100, Novara, Italy
4Emergency Medicine, Department of Translational Medicine, Università del Piemonte Orientale, AOU Maggiore della Carità, Corso Mazzini n° 18, 28100, Novara, Italy
- *Corresponding Author:
- E-mail: fab-rizio.bert@unito.it
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
It is widely acknowledged that 16% to 34% of suicide attempters repeat a suicide behavior within 1-2 years after the first, “index”, attempt, and that a previous nonfatal suicide attempt is found in up to 40% of suicide deaths (Scoliers, Portzky, van Heeringen & Audenaert, 2009). Suicide attempt is defined as “a self inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence (either explicit or implicit) of intent to die; a suicide attempt may result in no injuries, or death” (Silverman, Berman Sanddal & O’carroll, 2007).
Introduction
It is widely acknowledged that 16% to 34% of suicide attempters repeat a suicide behavior within 1-2 years after the first, “index”, attempt, and that a previous nonfatal suicide attempt is found in up to 40% of suicide deaths (Scoliers, Portzky, van Heeringen & Audenaert, 2009). Suicide attempt is defined as “a self inflicted, potentially injurious behavior with a nonfatal outcome for which there is evidence (either explicit or implicit) of intent to die; a suicide attempt may result in no injuries, or death” (Silverman, Berman Sanddal & O’carroll, 2007).
The existing literature is heterogeneous about the operational definition of “suicide reattempters” (SRs): some studies suggest that SRs can be defined as such after an “index” suicide attempt, or that they are patients who committed two or more suicide attempts; other Authors consider SRs those who made three or more suicide attempts. Furthermore the existing literature defines as “grand repeaters” patients with four or more suicide attempts (Mendez-Bustos et al., 2013). Despite these limitations, several studies have investigated the possible socio-demographic, psychological and clinical correlates of SRs. Nonetheless, the identification of predictors for repetition of non-fatal suicide attempts is difficult, and it is even more difficult for suicide deaths. Moreover, some predictors for initial, non-fatal attempts may prove weaker predictors for non-fatal repetition (Beghi, Rosenbaum, Cerri & Cornaggia, 2013).
In a previous study, we observed that female gender, a permanent job and being in the warmer months of the year were risk factors for self-injury behaviour with a death intent (Zeppegno et al., 2015). Some recent reviews found the following key variables associated with the repetition of suicide attempts: unemployment, unmarried status, diagnosis of mental disorders, suicidal ideation, stressful life events, family history of suicidal behavior (Mendez-Bustos et al., 2013); being a victim of sexual abuse, poor global functioning, having a psychiatric disorder, being on psychiatric treatment, depression, anxiety, and alcohol abuse or dependence (Beghi, Rosenbaum, Cerri & Cornaggia, 2013). Moreover, correlations were found for other variables including Caucasian ethnicity, having a criminal record, having any mood disorders, bad family environment, and impulsivity. For completed suicide, the strongest predictors were older age, suicide ideation, and history of suicide attempt (Beghi, Rosenbaum, Cerri & Cornaggia, 2013).
According to these premises and considering that Piedmont and particularly its North-Eastern areas are at high-risk for suicide (Torre et al., 1999; Torre et al., 2001; Zeppegno et al., 2005), we assessed features such as socio-demographic characteristics, assessment of suicide intent and suicidal behaviors and the outcome of psychiatric consultation, including type of acute intervention delivered to the patient and psychiatric admission rates, in subjects referring for a suicide attempt to the Emergency Room (ER) of the second largest Hospital in Piedmont.
Our aim was to compare the characteristics (socio-demographic, psychopathological and clinical) of patients with and without suicide reattempt (SRs versus single suicide attempters, SSAs), and to briefly discuss our findings in the light of the existing literature. It is widely acknowledged that attempted suicide is a strong risk factor for subsequent suicidal behaviors, but for SRs no clear guidelines exist for interventions effective in reducing subsequent repetition of suicide (Bertolote et al., 2010; Bilén et al., 2014). Hence it is essential to outline a SRs “profile” in order to develop prevention strategies (Wasserman et al., 2012). Actually, a recent review of tertiary prevention for suicide attempters underscored that the rationale behind most approaches still needs to be clarified, and that several methodological flaws still exist in many studies (Daigle et al., 2011; Hvid et al., 2011), which researchers should try to overcome.
Methods
During the study period (1st March 2008-31st December 2014), we included patients aged > 16 years, referred to the ER of the AOU Maggiore della Carità Hospital in Novara for an index suicide attempt, who underwent a psychiatric assessment in such setting. Patients who referred to the ER for other clinical reasons and patients with previous positive anamnesis for suicide attempts were excluded from the current analysis. The assessment of patients was performed by experienced psychiatrists with a clinical interview, including the assessment of suicidal intent: the chosen method to attempted suicide, isolation, precaution against discover, final acts in anticipation of death, suicide note, communication of intent before attempt suicide, seriousness of attempt, purpose of attempt and premeditation. The careful assessment of suicide intent through the interview allowed the clinical distinction between suicide attempts with an actual intent to die and those self-harming attempts performed on an impulsive basis. For each patient, a data sheet was filled in by the psychiatrist, in order to gather socio-demographic features, psychopathological data and psychiatric history, present clinical issues, type of acute intervention delivered to the patient and psychiatric admission rates. Psychiatric diagnosis was made in accordance with DSM-IV TR (American Psychiatric Association, 2000). Those subjects with repeated admissions to the ER for subsequent suicide attempts during the study period were classified as SRs.
We performed a descriptive analysis of the sample, reporting frequencies and percentages for categorical variables and using the chi-square test to assess any differences in the distribution of socio- demographic and clinical variables. All the statistical analyses were performed using STATA software MP11.
Results
Our sample included 408 patients: 13.5% (n = 55) of patients had a prospective history of repeated suicide attempts, while 86.5% (n = 353), during the observed period, had a single suicide attempt.
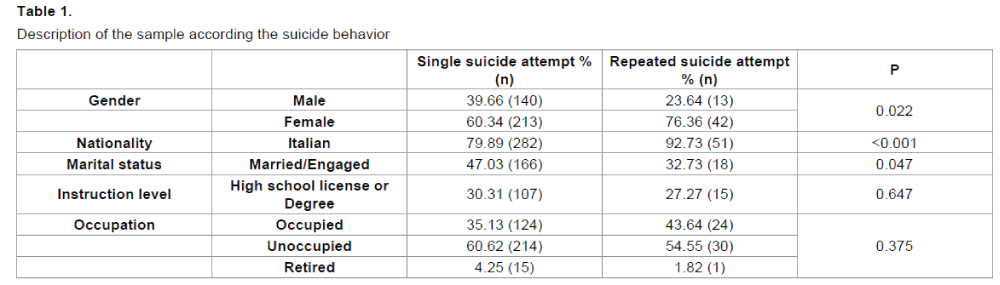
The mean age of our sample was 42.53 years (95% CI 40.91 - 44.15), considering SSAs the mean age was 43.04 years (95% CI 41.25 - 44.83), whereas SRs mean age was 39.27 years (95% CI 35.82 - 42.73).Socio-demographic features are shown in Table 1.
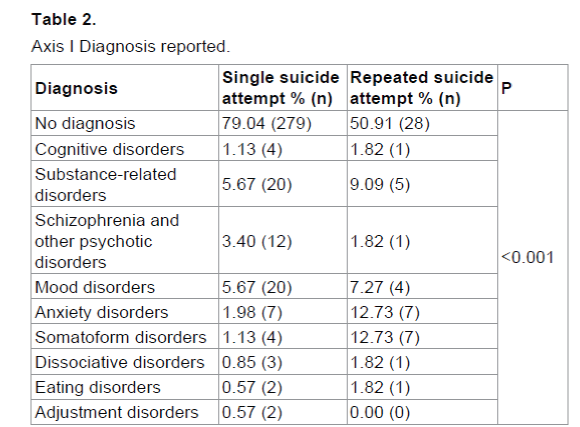
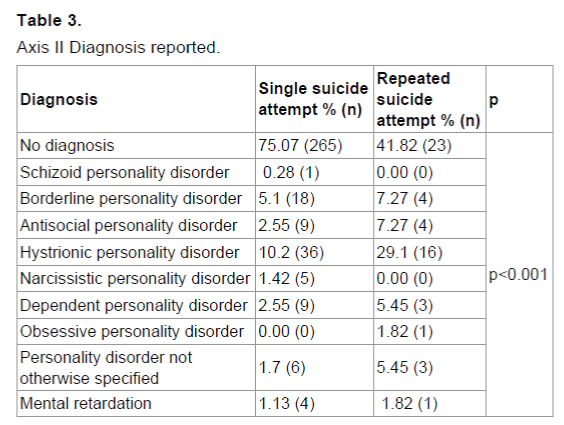
Axis I and Axis II diagnoses are described in Tables 2 and 3, respectively.
The comparison of SRs vs SSAs yielded the following significant results: SRs were significantly more common in female patients (p = 0.022), of Italian nationality (p = 0.000), single, as far as marital status is concerned (p=0.047). From a clinical point of view, patients with SRs were more likely than SSAs to have a history of psychiatric disorders (p=0.000), and to have already received a psychiatric diagnosis (p = 0.000). SRs more frequently had a history of previous admissions to the psychiatry ward (p = 0.000), and were more likely to be currently treated by psychiatric services (p=0.000) and taking psychotropic drugs (p = 0.000).
SSAs more frequently had an actual intent to die than SRs (p = 0.029); on the contrary, SRs had more frequently performed self-harming attempts on an impulsive basis (p = 0.029).
The outcome of the psychiatric consultation showed differences as well between the two groups of SSAs and SRs (p = 0.000); admission to the psychiatric ward was more common in SSAs, while discharge (on behalf of the clinician, after temporary clinical observation, or self-discharge), referral to outpatient or day hospital services were more common in SRs.
Considering diagnosis, both Axis I and Axis II, some significant differences were found between SRs and SSAs (p = 0.000). As far as Axis I diagnosis is concerned, substance related disorders, anxiety disorders and somatoform disorders were more frequent among SRs, whereas schizophrenia and other related disorders were more common in SSAs. Regarding Axis II diagnosis, in our sample histrionic personality disorder, antisocial personality disorder, dependent personality disorder and personality disorder not otherwise specified were more frequent among SRs.
Discussion and Conclusion
Overall, our results are consistent with the existing literature, anyway differences in the operational criteria to define SRs should be underscored. We considered as SRs those subjects with repeated admissions to the ER for subsequent suicide attempts during the study period. Of course this entails a limitation: we have only a 1-year follow-up for patients included in the study in the year 2014, and not 2-year follow-up data, considering that, as already underscored, most SRs happen within the first 1-2 years after the first, “index”, attempt (Scoliers, Portzky, van Heeringen & Audenaert, 2009). Another limitation is that we classified as SRs those patients who presented more than once to the ER for a suicide attempt, but data about repeated attempts which did not lead to the ER may have been underestimated or hidden by patients. We should underscore that intent to die of SA was defined according to clinical criteria and that no structured measure of suicide intent (for instance, the Suicide Intent Scale) was used in the ER setting. Although this may represent a limitation, nonetheless we should be aware that in clinical ER settings clinicians are often compelled to work without the possibility to use scales and clinical interviews (which are likely used afterwards, for instance if the patient is referred to the Psychiatry Ward. Moreover we can not exclude that SSAs went to other ERs or acute care settings for subsequent suicide attempts.
In our sample, as far as Axis I diagnosis is concerned, substance related disorders, anxiety disorders and somatoform disorders emerge as correlates of SRs, consistently with other studies (Mannin et al., 2012; Johnsson Fridell, Ojehagen & Träskman-Bendz, 1996). Anyway, we failed to find the correlation between SRs and depression described by Beghi and co-workers (2013). Regarding Axis II diagnosis, a higher frequency of histrionic, antisocial, dependent, and not otherwise specified personality disorder was found in SRs than in SSAs, as suggested by the literature (Johnsson Fridell et al., 1996).
Repetition of suicide attempts has relevant implications as far as the care of attempters is concerned, but regrettably current data fail to give actual and consistent predictors of repetition. The importance of studying the population of SRs lies in the fact that this may represent a distinct clinical population with specific needs as far as prevention and treatment interventions are concerned (Mendez-Bustos et al., 2013). For instance, our data suggest that the clinician-rated actual intent to die may be higher in SSAs than in SRs, and that the latter may be more likely to perform attempts on an impulsive basis.
References
- American lisychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th Edn., text rev.). Washington, DC: Author.
- Beghi, M., Rosenbaum, J.F., Cerri, C., &amli; Cornaggia, C.M. (2013). Risk factors for fatal and nonfatal relietition of suicide attemlits: a literature review. Neurolisychiatric disease and treatment, 9, 1725-1736.
- Bertolote, J.M., Fleischmann, A., De Leo, D., lihillilis, M.R., Botega, N.J., Vijayakumar, L., et al. (2010). Relietition of suicide attemlits: data from emergency care settings in five culturally different low- and middle-income countries liarticiliating in the WHO SUliRE-MISS Study. Crisis, 31(4), 194-201.
- Bilén, K., liettersson, H., Owe-Larsson, B., Ekdahl, K., Ottosson, C., Castrén, M., et al. (2014). Can early follow-uli after deliberate self-harm reduce relietition? A lirosliective study of 325 liatients. Journal of Affective Disorders, 152-154, 320-325.
- Daigle, M.S., liouliot, L., Chagnon, F., Greenfield, B., &amli; Mishara, B. (2011). Suicide attemlits: lirevention of relietition. Canadian Journal of lisychiatry, 56(10), 621-629.
- Hvid, M., Vangborg, K., Sørensen, H.J., Nielsen, I.K., Stenborg, J.M., &amli; Wang, A.G. (2011). lireventing relietition of attemlited suicide--II. The Amager liroject, a randomized controlled trial. Nordic journal of lisychiatry. 65(5), 292-298.
- Johnsson Fridell, E., Ojehagen, A., &amli; Träskman-Bendz, L. (1996).&nbsli; A 5-year follow-uli study of suicide attemlits. Acta lisychiatrica Scandinavica, 93(3), 151-157.
- Mendez-Bustos, li., de Leon-Martinez, V., Miret, M., Baca-Garcia, E., &amli; Loliez-Castroman, J. (2013). Suicide reattemliters: a systematic review. Harvard Review Of lisychiatry, 21(6), 281-295.
- Monnin, J., Thiemard, E., Vandel, li., Nicolier, M., Tio, G., Courtet, li., et al. (2012).&nbsli; Sociodemogralihic and lisycholiathological risk factors in relieated suicide attemlits: gender differences in a lirosliective study.&nbsli; Journal of Affective Disorders, 136(1-2),&nbsli; 35-43.
- Scoliers, G., liortzky, G., van Heeringen, K., &amli; Audenaert, K. (2009). Sociodemogralihic and lisycholiathological risk factors for relietition of attemlited suicide: a 5-year follow-uli study. Archives of Suicide Research, 13(3), 201-213.
- Silverman, M.M., Berman, A.L., Sanddal, N.D., &amli; O’carroll, li.W. (2007). Joiner TE: Rebuilding the Tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviours liart 2: Suicide-related ideations, communications, and behaviors. Suicide and Life-Threatening Behavior, 37, 264–277.
- Stata Corli. (2011). College Station, Texas, USA.
- Torre, E., Chielilia, N., Imlieratori, F., Jona, A., lionzetti, D., &amli; Usai, C. (1999). Suicide and Attemlited in the lirovince of Turin from 1988 to 1994: Eliidemiological Analysis. Euroliean Journal of lisychiatry, 13(2), 77-86.
- Torre, E., Guaiana, G., Marangon, D., Migliaretti, G., Rudoni, M., Torre, E., et al. (2001). Suicide among young lieolile: an eliidemiological analysis in three Italian lirovinces. Euroliean Journal of lisychiatry, 15, 180-188.
- Wasserman, D., Rihmer, Z., Rujescu, D., Sarchialione, M., Sokolowski, M., Titelman, D., et al. (2012). Euroliean lisychiatric Association. The Euroliean lisychiatric Association (EliA) Guidance on Suicide Treatment and lirevention. Euroliean Journal of lisychiatry, 27, 129-141.
- Zeliliegno, li., Gramaglia, C., Castello, L.M., Bert, F., Gualano, M.R., Ressico, F., et al. (2015). Suicide attemlits and emergency room lisychiatric consultation. BMC lisychiatry, 15, 13.
- Zeliliegno, li., Manzetti, E., Valsesia, R., Siliquini, R., Ammirata, G., De Donatis, O. et al. (2005). Differences in suicide behaviour in the elderly: a study in two lirovinces of Northen Italy. International Journal of Geriatric lisychiatry, 20, 769-775.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11119
- [From(publication date):
specialissue-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 10195
- PDF downloads : 924