Renal Primitive Neuroectodermal Tumor in a Child with Brain Metastasis: A Case Report
Received: 15-May-2018 / Accepted Date: 14-Jun-2018 / Published Date: 19-Jun-2018 DOI: 10.4172/2476-2024.1000143
Abstract
Primitive neuroectodermal tumor (PNET) is a malignant small round cell tumor that typically arises from bone or soft tissue in adolescents and young adults. Renal PNET is extraordinarily rare and exhibits highly aggressive biological behavior with poor prognosis. It generally occurs in young adults and only a few pediatric cases have been reported.
Here, we present a case of renal PNET in an 11-month-old boy which developed brain metastasis after two years, despite combined modality treatment.
Keywords: PNET; Kidney; Brain metastasis; Children
Introduction
Primitive neuroectodermal tumor (PNET) is a malignant small round cell tumor, typically arises from bone and soft tissue in the trunk and axial skeleton, in adolescent and young adults [1]. Localization of PNET in genitourinary tract such as kidney, bladder and prostate and its occurrence in children less than 5 years of age is rare [2]. Owing to high aggressiveness and strong tendency of local recurrence and remote metastasis of renal PNETs, the overall prognosis of tumor is poor [3].
Here we report a rare case of renal PNET which developed brain metastasis and underwent two times craniotomy for his metastasis.
Case Report
An 11-month-old boy was referred to our hospital because of left flank mass, persistent for 3 months duration. His past medical history and lab data were unremarkable. Clinical examination was revealed only a palpable renal mass which was firm, fixed and non-tender. No ascites or peripheral edema was detected. Chest X-ray, lab tests and other evaluations showed no evidence of metastatic disease. Ultrasound revealed a heterogeneous mass, measuring 129*68*66 mm in middle and lower pole or left kidney.
The CT-scan of the abdomen was demonstrated a heterogeneous mass lesion measuring 130*66 mm arising from left kidney involving mid and lower pole, the most probable diagnosis was Wilms tumor.
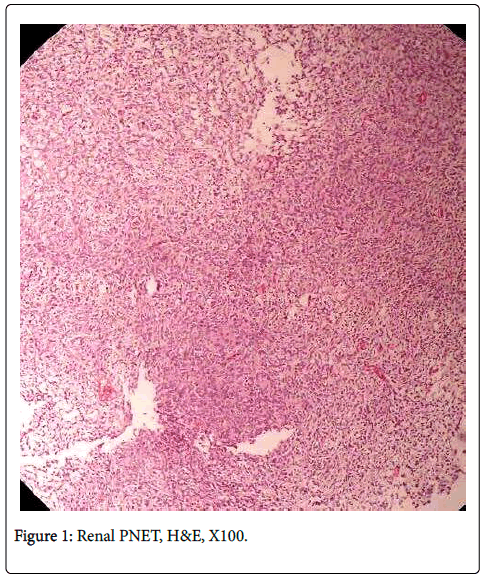
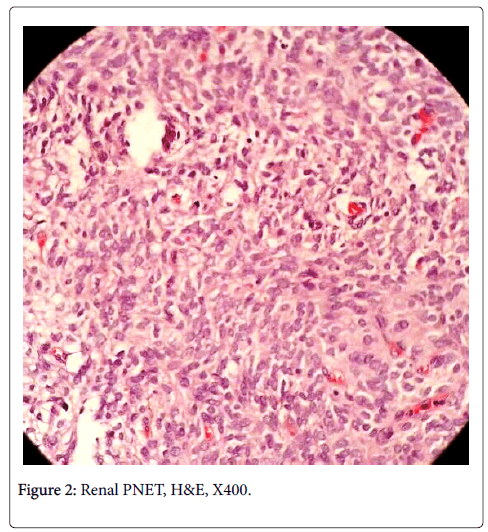
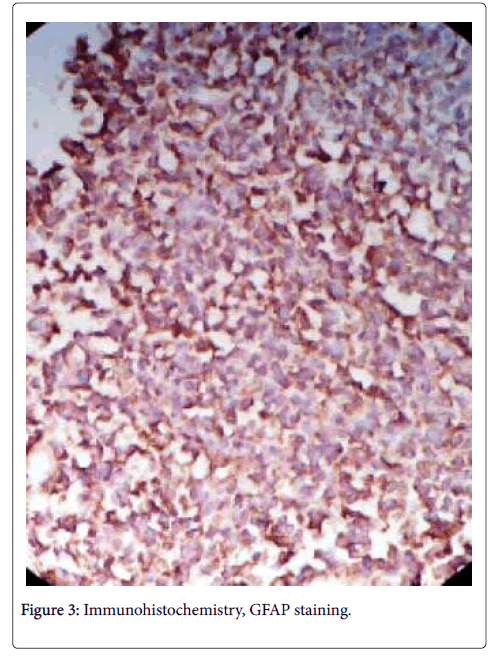
The patient underwent laparotomy and mass biopsy. Microscopically tumor consisted of small-sized round oval shaped cells with irregular nuclei and ill-defined cytoplasmic border and poorly formed rosette like structures (Figures 1 and 2). We carried out an immunohistochemistry (IHC) study using the avidin-biotin peroxidase method. IHC stains revealed positivity for vimentin, strong membranous positivity for CD99 (Figure 3) and negativity for GFAP, cytokeratin, LCA, desmin, WT1 and synaptophysin. Based upon the microscopic appearance and IHC features, the diagnosis of renal PNET was established.
The patient was subsequently begun on systemic chemotherapy for 6 cycles. Afterwards the patient underwent a left radical nephrectomy with removal associated lymph nodes and ureter. Resected specimens were sent to pathologic department for macroscopic and microscopic evaluation. Gross examination of the resected kidney showed extensive replacement of the renal parenchyma by grayish-yellow 8*3*1 cm mass with focal cystic areas and massive irregular areas of necrosis. Microscopically, some sections of normal renal parenchyma were seen. Massive necrosis with foamy macrophages, and hemosiderin deposition were noted. A small focus of blue small round cells aggregation with local area of calcification and giant cell reaction were seen. Resection was complete. The patient received appropriate chemotherapy and other palliative treatments.
After two years he was admitted in our hospital because of convulsion and right hemiparesis. No infected disease was detected. In brain CT scan, well-defined hypodense mass lesion containing hemorrhage was seen (Figure 4). The mass involved left front parietal lobe associated with pressure to left ventricle and minimally midline shift. Radiologic differential diagnoses were cystic astrocytoma, ependymoma, and metastasis. Also in MRI study hemorrhagic tumor was diagnosed. Cystic brain mass was aspirated and sent to lab for cytological examination. No metastatic cell was identified in cytological evaluation. Finally the patient underwent craniotomy and mass biopsy. Microscopically sections showed neoplastic proliferation of mesenchymal tumoral cells in diffuse pattern.
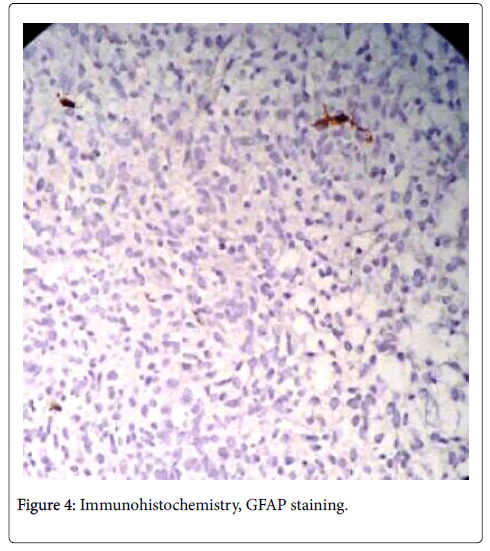
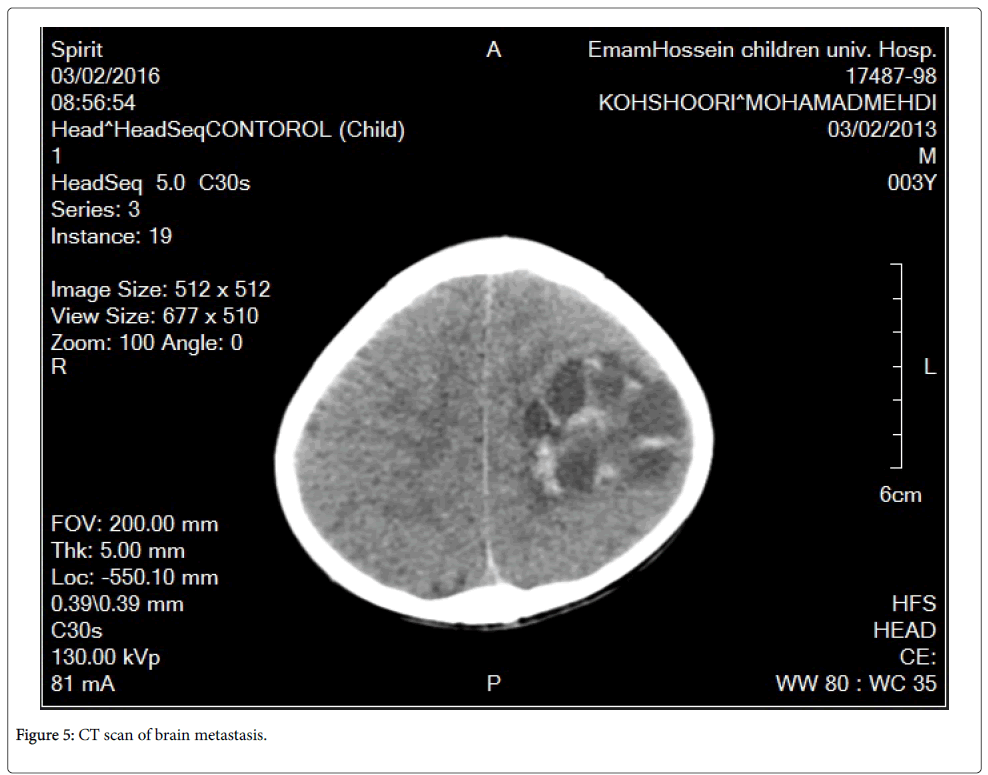
These cells had high N/C ratio with round to oval nuclei and pseudo rosette formation. Foci of hemorrhaged and necrosis were seen. Gliosis also was presented. IHC study confirmed metastasis from previous renal PNET of the patient (Figure 5).
In follow up, despite of treatment, the patient had another recurrence of brain metastasis after 7 months and underwent craniotomy again. At now he is alive and receives his treatment.
Discussion
PNET is a malignant small cell neoplasm of neural crest origin. It is a very rare tumor representing about 1% of all sarcoma [4]. Renal PNET was first reported by Mor and colleagues [4,5]. These are only a few reported cases of renal PNET. Renal PNET is highly aggressive malignant neoplasm and is more aggressive than PNET arising from other sites [6]. From this point the distinction from other primary malignancies of the kidney is crucial for prognosis. The clinical features of renal PNET are nonspecific and including vague pain, mass in the flank, irregular fever, weight loss and hematuria [7]. Radiographic features of renal PNET are nonspecific and are usually presented as a huge renal mass with or without calcification. The diagnosis of renal PNET is made usually post operatively based on histopathology and the panel of IHC stains [4].
Differential diagnosis includes Wilms tumor, neuroblastoma, lymphoma, rhabdomyosarcoma, and clear cell sarcoma. Histologically, PNET consists of sheets and nests of primitive small round blue cells and presence of the Homer-wright rosettes [4]. IHC staining is crucial in the diagnosis [8]. Renal PNET is positive for CD99 in more than 90%-95% of cases. Other helpful markers are neuron specific enolase, vimentin and synaptophysin. Furthermore cytogenetic studies showed that renal PNET is consistently associated with translocation of the long arm of chromosome 11 and 22, t(11,22) (q24.q12) in more than 90% of the tumors. It is also characteristic of PNET and Ewing sarcoma [4]. Unfortunately cytogenetic study was not performed in our case.
Renal PNET is a highly aggressive tumor and almost 50% of patient present with distant metastasis, most commonly to regional lymph nodes, lungs and liver, but brain metastasis is very rare. Survival rate is poor and most patients die within one year of the diagnosis.
Since PNET biologically behaves like Ewing’s sarcoma it should be treated with combination of radical nephrectomy and chemotherapy. In cases where there is an incomplete resection or positive margin or recurrence of the tumor, radiation is recommended.
Conclusions
Renal primitive neuroectodermal tumors are very rare and extremely aggressive and brain metastasis although is a rare event, but should be considered. In such cases the pathologist has a major role in establishing a final diagnosis through histological and IHC profile. IHC for CD99 is very helpful in the diagnosis of renal PNET.
References
- Gupta S, Billadello L, Casalino DD (2014) Renal primitive neuroectodermal tumor. J Urol 187: 2211-2212.
- Mohsin R, Hashmi A, Mubarak M (2011) Primitive neuroectodermal tumor/Ewing's sarcoma in adult uro-oncology: A case series from a developing country. Urol Ann 3: 103-107.
- Yang C, Xu H, Zhou J, Hao Z, Wang J, et al. (2015) Renal Primitive Neuroectodermal Tumor: A Case Report. Medicine (Baltimore). 94: e2304.
- Asiri M, Al-Sayyad A (2010) Renal primitive neuroectodermaltumour in childhood: Case report and review of literature. Can Urol Assoc J. 4: e158-160.
- Mor Y, Nass D, Raviv G, Neumann Y, Nativ O, et al. (1994) Malignant peripheral primitive neuroectodermal tumor (PNET) of the kidney. Med Pediatr Oncol 23: 437-440.
- Lam JS, Hensle TW, Debelenko L, Granowetter L, Tennenbaum SY (2003) Organ-confined primitive neuroectodermal tumor arising from the kidney. J Pediatr Surg 38: 619-621.
- Mandal PK, Mukherjee S, Roy S, Bhattacharyya NK (2012) PNET of kidney: Report of four cases. Indian J Med Paediatr Oncol 33: 130-133.
- Gupta NP, Singh BP, Raina V, Gupta SD (1995) Primitive neuroectodermal kidney tumor: 2 case reports and review of the literature. J Urol 153: 1890-1892.
Citation: Naimi A, Soltan M, Saberi E, Riahinezhad M (2018) Renal Primitive Neuroectodermal Tumor in a Child with Brain Metastasis: A Case Report. Diagn Pathol Open 3: 143. DOI: 10.4172/2476-2024.1000143
Copyright: © 2018 Naimi A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 5696
- [From(publication date): 0-2018 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 4848
- PDF downloads: 848