Case Report Open Access
Renal Cell Carcinoma Invading Duodenum: Management by Pancreaticoduodenectomy and Discussion of Treatments
Juan Chipollini1 and Gaetano Ciancio1,2*
1Department of Urology, University of Miami Miller School of Medicine, Miami, Florida, USA
2Department of Surgery, Division of Transplantation, Miami Transplant Institute, University of Miami Miller School of Medicine, Jackson Memorial Hospital, Miami, Florida, USA
- Corresponding Author:
- Gaetano Ciancio, M.D
University of Miami Miller School of Medicine
Department of Surgery and Urology
University of Miami Miller School of Medicine
Jackson Memorial Hospital, Miami Fl
Miami Transplant Institute, P.O. Box 012440
Miami, Fl 33101, USA
Tel: (305) 355-5460
Fax: (305) 355-5797
E-mail: gciancio@med.miami.edu
Received Date: February 9, 2016 Accepted Date: February 29 2016 Published Date: March 06, 2016
Citation:Chipollini J, Ciancio G (2016) Renal Cell Carcinoma Invading Duodenum: Management by Ancreaticoduodenectomy and Discussion of Treatments. J Gastrointest Dig Syst 6:394. doi:10.4172/2161-069X.1000394
Copyright: © 2016 Chipollini J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
At present, complete surgical resection remains the standard for curative intervention in cases of locally advanced renal cell carcinoma (RCC) although the role of surgery in cases of adjacent visceral invasion remains controversial. We report a case of a right sided RCC involving the duodenum and head of pancreas in which en-bloc resection was achieved by radical nephrectomy and concomitant pancreaticoduodenectomy. For those patients with good performance status, aggressive interventions should be thoroughly discussed along with the role of targeted systemic therapies in the adjuvant setting.
Keywords
Pancreaticoduodenectomy; Duodenum
Introduction
In 2015, an estimated 61,560 new kidney and renal pelvis cancers were diagnosed in the United States, and approximately 14,080 died of this disease [1]. Renal cell carcinoma (RCC) is anadenocarcinoma of the renal parenchyma, and accounts for more than 80% of kidney cancer in adults [2]. With the widespread use of computer tomography (CT), the classic triad of flank pain, hematuria, and flank mass is rarely seen today and only a third of RCC cases present with locoregional or widespread metastatic disease [1].
While surgical extirpation has been the mainstay for smaller lesions, the role and timing of surgery in cases of aggressive disease with adjacent invasion into surrounding viscera remains controversial [3]. It is known that complete resection of RCC provides the best chance for long term survival, though this has been mostly proven in the setting of oligometastatic disease [4,5]. The current literature is scarce when it comes to nephrectomy and concomitant resection of intra-abdominal organs. We present a case of a patient with right sided RCC invading into duodenum and pancreas as well as subsequent treatment.
Case Report
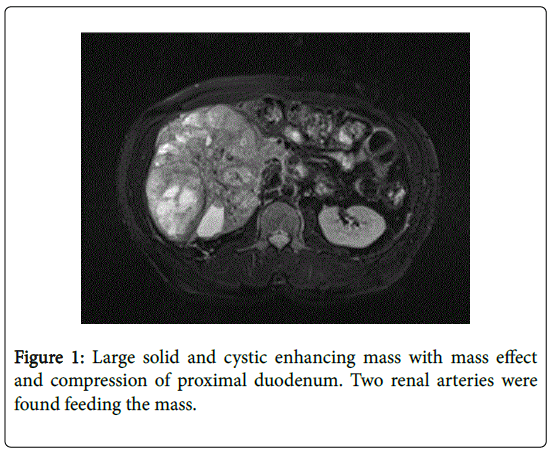
A 50 year-old male with past medical history for hypertension presented with weakness, fatigue and hematuria. He denied any abdominal pain, nausea or vomiting. His physical exam demonstrated a clearly palpable abdominal mass noted from the right subcostal region to almost the level of the umbilicus. A CT of the abdomen and pelvis ordered by his primary care physician revealed a large solid and cystic enhancing mass replacing the right renal parenchyma measuring 17 cm in craniocaudal dimension, 16.4 cm in anterior-posterior diameter, and 11.2 cm in transverse diameter (Figure 1). There was also associated mild gastric distension, due to the mass effect on the proximal duodenum. Rest of metastatic workup revealed multiple bilateral pulmonary nodules as well a 1 cm lytic lesion in the right third rib. Magnetic resonance imaging showed lack of soft tissue planes between the mass and inferior vena cava (IVC) but no gross invasion noted. His initial creatinine was 1.10 mg/dL and hemoglobin and hematocrit 7.8 g/dL and 26.7 g/dL, respectively. The case was discussed at multidisciplinary tumor board conference and consensus was to attempt complete resection given the patient’s intractable hematuria and acceptable performance status. The patient was presented the options and he agreed to proceed with open radical nephrectomy and indicated procedures.
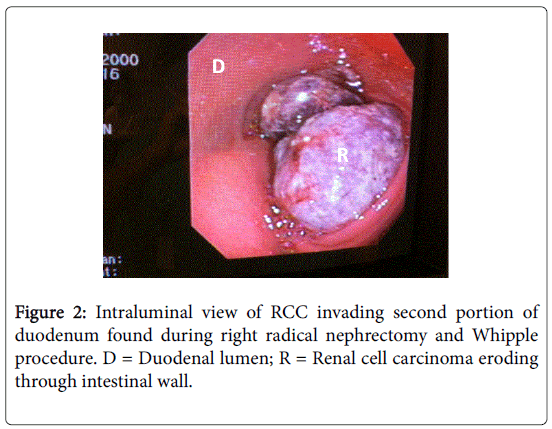
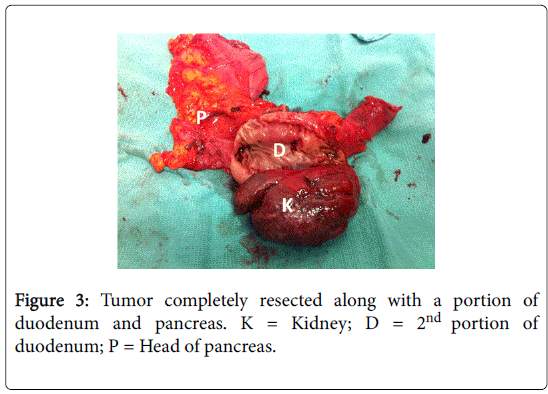
A Chevron incision was made three fingers’ breadth below the costal margin and a Rochard retractor system used to optimize exposure of the upper abdomen. Incision on the peritoneal lining over the line of Toldt allowed for reflection of the colon medially. Early intraoperative ligation of the renal artery was pursued by mobilizing the kidney medially until the renal artery can be identified and ligated [6]. Early arterial ligation results in decompression of collateral circulation and decreased blood loss. Liver mobilization was then performed using our “piggyback” technique [7,8] in order to gain further exposure of the right upper retroperitoneum as well as the retrohepatic IVC. Once the IVC was carefully dissected from the mass, the renal vein was encountered and ligated with no tumor thrombus found. At this point, attention was paid to the duodenum which appeared adherent to the mass with some fullness noted in its lumen. At this point, the gastroenterology service was called to perform an intraoperative esophagogastroduodenoscopy which revealed intraluminal growth of the mass into the second portion of the duodenum (Figure 2). The head of the pancreas also seemed adherent to the mass and after discussion with another onsultant, a pancreaticoduodenectomy seemed the best option for complete resection. A classic Whipple procedure was then performed and the specimen was able to be removed en-bloc for pathologic evaluation (Figure 3). The patient tolerated the procedure well with no major intraoperative complications.
Post-operatively, the patient developed an infected pleural effusion which required pigtail catheter drainage, but was able to be discharged home on post-operative day 10. Histopathological examination revealed clear cell RCC, 13.6 cm in greatest dimension, Fuhrman nuclear grade IV of IV, and tumor extending into pericaliceal system. The duodenal mass and pancreatectomy specimen was confirmed to be RCC with negative resection margins and 0 out of 2 lymph nodes negative for disease for an American Joint Committee on Cancer (AJCC) classification (7th edition) of pT4N0. Surveillance imaging 3 months later showed numerous enhancing metastatic lesions within the liver which were biopsy-proven metastatic RCC (mRCC). Patient was initiated on tyrosine kinase inhibitor (TKI) therapy with Sunitib 50 mg per day, but 2 months later developed lytic lesions along his thoracic spine and the patient opted for second line treatment with mammalian target of Rapamycin (mTOR) inhibitor Everolimus 10 mg daily before deciding on end-of-life care due to the terminal nature of his disease.
Discussion
Approximately one third of RCC cases make their debut in advanced stages of the disease [9,10]. The pancreas and duodenum are rare sites for RCC involvement, likely due to the protective nature of the anterior and posterior renal fasciae [11]. The route by which RCC spreads to the pancreas is unclear, with both hematagenous and lymphotagenous theories proposed [12]. RCC involving the duodenum has only been described in a number of case reports, and can present with upper GI bleeding [13-16]. As such, metastatic lesions to the upper gastrointestinal tract are sometimes diagnosed on endoscopy [17].
Resection for locally advanced RCC has increasingly been performed with acceptable morbidity and mortality rates in the last few years [18,19], and there are some series describing such an aggressive approach with modest survival benefit in this group of patients [20,21]. Furthermore, clinical and pathological stage discrepancy is common in surgically treated patients which can have significant impact on clinical outcome [22]. Thus, surgical extirpation has been the mainstay of treatment for patients who present with stage I-III RCC. For those who present late with advanced and metastatic disease (stage IV), the overall clinical course of RCC varies; approximately 50% of patients survive less than 1 year and 10% survive for more than 5 years [23].
Fortunately, a better understanding of RCC tumorigenesis has led to the emergence of targeted molecular therapies as equally effective alternatives to cytokines, and have shown a survival benefit when combined with surgery in mRCC [24]. Clinical trials have proven the effectiveness of targeted therapies for advanced RCC and a growing body of work is underway to provide molecular biomarkers for response of these new therapies which act primarily against the vascular endothelial growth factor (VEGF) or mammalian target of Rapamycin (mTOR) pathways. There are currently 8 US Food and Drug Administration (FDA) approved agents available for the treatment of mRCC [25]. Five of these agents target VEGF or its receptors, two inhibit activity of mTOR, and one is a recombinant form of the endogenous cytokine IL-2. Each of these agents provides clinical benefit to a subset of patients, and the overall outlook for patients with advanced RCC is better today than it was 10 years ago [26].
We present a case in which nephrectomy and pancreaticoduodenectomy was performed for locally advanced RCC. The patient was able to live an additional 6 months before succumbing to his disease. It is unclear if starting systemic therapy earlier in the adjuvant setting could have extended his overall survival, although ongoing prospective phase III trials are currently ongoing that will answer this question soon. For those patients with good performance status presenting with locally advanced RCC with invasion to neighboring viscera, surgical resection is a viable option that should be comprehensively discussed. Further studies to evaluate survival benefit in combination with targeted therapies are anticipated.
Conclusion
Complete surgical extirpation is possible in cases of RCC invading other organs such as pancreas and duodenum. A contemporary, multiinstitutional cohort is needed to determine which patients may benefit from such aggressive surgical interventions while the role of systemic therapies continues to evolve in the management of these locally invasive tumors.
References
- Siegel RL, Miller KD, Jemal A (2015) Cancer statistics, 2015 .CA Cancer J Clin 65: 5-29.
- King SC, Pollack LA, Li J, King JB, Master VA (2014) Continued increase in incidence of renal cell carcinoma, especially in young patients and high grade disease: United States 2001 to 2010.J Urol 191: 1665-1670.
- Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, et al. (2015) EAU guidelines on renal cell carcinoma: 2014 update.Eur Urol 67: 913-924.
- Bhat S (2010) Role of surgery in advanced/metastatic renal cell carcinoma.Indian J Urol 26: 167-176.
- Russo P, Synder M, Vickers A, Kondagunta V, Motzer R (2007) Cytoreductive nephrectomy and nephrectomy/complete metastasectomy for metastatic renal cancer.ScientificWorldJournal 7: 768-778.
- Ciancio G, Vaidya A, Soloway M (2003) Early ligation of the renal artery using the posterior approach: a basic surgical concept reinforced during resection of large hypervascular renal cell carcinoma with or without inferior vena cava thrombus. BJU Int 92: 488-489.
- Ciancio G (2011) Liver transplantation techniques for the surgical management of renal cell carcinoma with tumor thrombus in the inferior vena cava: step-by-step description. Eur Urol 59: 401-406.
- Ciancio G, Livingstone AS, Soloway M (2007) Surgical management of renal cell carcinoma with tumor thrombus in the renal and inferior vena cava: the University of Miami experience in using liver transplantation techniques. Eur Urol 51: 988-995.
- Frank I, Blute ML, Cheville JC, Lohse CM, Weaver AL, et al. (2002) An outcome prediction model for patients with clear cell renal cell carcinoma treated with radical nephrectomy based on tumor stage, size, grade and necrosis: the SSIGN score.J Urol 168: 2395-2400.
- Lam JS, Belldegrun AS, Pantuck AJ (2006) Long-term outcomes of the surgical management of renal cell carcinoma.World J Urol 24: 255-266.
- Raptopoulos V, Lei QF, Touliopoulos P, Vrachliotis TG, Marks SC Jr (1995) Why perirenal disease does not extend into the pelvis: the importance of closure of the cone of the renal fasciae.AJR Am J Roentgenol 164: 1179-1184.
- Kassabian A, Stein J, Jabbour N, Parsa K, Skinner D, et al. (2000) Renal cell carcinoma metastatic to the pancreas: a single-institution series and review of the literature.Urology 56: 211-215.
- Haidong W, Jianwei W, Guizhong L, Ning L, Feng H, et al. (2014) Ampullary tumor caused by metastatic renal cell carcinoma and literature review.Urol J 11: 1504-1507.
- Street R, Brady J, Slobodav G (2013) Renal cell carcinoma presenting with Melena from direct invasion into the duodenum: a case report and a review of literature.J Okla State Med Assoc 106: 477-479.
- Schlussel AT, Fowler AB, Chinn HK, Wong LL (2013) Management of locally advanced renal cell carcinoma with invasion of the duodenum.Case Rep Surg 2013: 596362.
- Bhatia A, Das A, Kumar Y, Kochhar R (2006) Renal cell carcinoma metastasizing to duodenum: a rare occurrence.Diagn Pathol 1: 29.
- Hsu CC, Chen JJ, Changchien CS (1996) Endoscopic features of metastatic tumors in the upper gastrointestinal tract.Endoscopy 28: 249-253.
- Sperti C, Moletta L, Patanè G (2014) Metastatic tumors to the pancreas: The role of surgery.World J Gastrointest Oncol 6: 381-392.
- Santoni M, Conti A, Partelli S, Porta C, Sternberg CN, et al. (2015) Surgical resection does not improve survival in patients with renal metastases to the pancreas in the era of tyrosine kinase inhibitors.Ann Surg Oncol 22: 2094-2100.
- Margulis V (2007) Renal cell carcinoma clinically involving adjacent organs: experience with aggressive surgical management. Cancer 109: 2025-2030.
- Karellas ME, Jang TL, Kagiwada MA, Kinnaman MD, Jarnagin WR, et al. (2009) Advanced-stage renal cell carcinoma treated by radical nephrectomy and adjacent organ or structure resection.BJU Int 103: 160-164.
- Svatek RS, Lotan Y, Herman MP, Duchene DA, Sagalowsky AI, et al. (2006) The influence of clinical and pathological stage discrepancy on cancer specific survival in patients treated for renal cell carcinoma.J Urol 176: 1321-1325.
- Yuen JS (2009) Molecular targeted therapy in advanced renal cell carcinoma: A review of its recent past and a glimpse into the near future.Indian J Urol 25: 427-436.
- Flanigan RC, Salmon SE, Blumenstein BA, Bearman SI, Roy V, et al. (2001) Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer.N Engl J Med 345: 1655-1659.
- Bex A, Gore M, Mulders P, Sternberg CN (2012) Recent advances in the treatment of advanced renal cell carcinoma: towards multidisciplinary personalized care.BJU Int 110: 1289-1300.
- Vaishampayan U (2014) The effect of targeted therapy on overall survival in advanced renal cancer: a study of the
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12157
- [From(publication date):
April-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 11226
- PDF downloads : 931