Research Article Open Access
Removing the User Fees for the Under-Fives' Simple Malaria Treatment in Cameroon: Effect on the Health Services Utilization
Isidore Sieleunou*, Emmanuel Betsi, Jean Christian Kouontchou, Alain Takeu Nguela and Habakkuk Azinyui YumoSchool of Public Health, University of Montreal, Canada
- *Corresponding Author:
- Isidore Sieleunou
School of Public Health
University of Montreal, Canada
Tel: 15142199771
E-mail: i.sieleunou@yahoo.com
Received date: November 14, 2015 Accepted date: November 26, 2015 Published date: December 03, 2015
Citation: Sieleunou I, Kouontchou JC, Nguela AT, Yumo HA (2015) Removing the User Fees for the Under-Fives' Simple Malaria Treatment in Cameroon: Effect on the Health Services Utilization. J Community Med Health Educ 5:383. doi: 10.4172/2161-0711.1000383
Copyright: © 2015 Sieleunou I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Access to free diagnoses and treatments has been shown to be a major determinant in malaria control. The Cameroonian government launched in February 2011 the exemption of the under-fives' simple malaria treatment policy. This study aimed at assessing the main effect of the policy on services utilization. Methods: A concurrent mixed-method research using time series data collected in July 2011 and April 2012, and qualitative data collected in April 2012 was conducted. Content analysis was used for the qualitative data. For the quantitative data, a proxy was used to measure living standards by calculating a composite index using principal component analysis. Results: General outpatients consultations and of the under-five (U5) increased to about 10% during the year 2011 compared to the year 2010 (before the policy). The average number of consultations for simple malaria cases in children U5 increased in the months following the launch of the policy then started declining from September 2011. The proportion of U5 who was exempted from payment of drugs increased from 19.6% to 32.9% at 4 and 12 months after the implementation of the policy. In contrast there was no effect in reducing inequalities among socioeconomic groups: the rural and lowest socio-economic households benefit less from the exemption measure (RR respectively 2.7, 1.6). Two thirds of U5 who used health services for uncomplicated malaria paid on average 2940 FCFA (6 $USA) for the treatment. The major part of this cost was made on the acquisition of artemisinin combination therapy (1680 FCFA/3.5 $USA).
Keywords
User fees; Malaria; Exemption policy; Inequality; Mixedmethods; Evaluation; Under five; Cameroon
Context
Malaria is a major cause of morbidity and mortality in children less than 05 years (U5) in sub-Saharan Africa. WHO estimates that in 2008, malaria caused an estimated one million deaths among children in the world [1]. In the African continent, a child dies of malaria every second and this scourge is responsible for 20% of all children deaths [1].
In Cameroon, malaria remains the leading cause of morbidity in U5 with an incidence of about 187 new cases per 1000 [2] and the leading cause of death in this age group with 22% of deaths [3]. This problem contributes significantly to the high child mortality in Cameroon situated at 127 per 1000 live births [4].
The disease is endemic in the country with three epidemiological strata: (i) the stratum of a stable and continuous transmission throughout the year in the southern part of the country, (ii) the stratum of an unstable and long transmission in Adamawa region and (iii) the stratum of a short transmission length in the North and Far North regions.
In the Adamawa region, the incidence of malaria is 217 new cases per 1000, representing one of the most affected regions in the country [2]. The total number of actual cases of malaria in U5 in 2011 at national level (687,289) and in the Adamawa region (42,216) [2] are underestimated, since a large number of treated cases at home or at the community level are not registered at health facilities.
In the Adamawa region, 66.67% of U5 are hospitalized for clinically diagnosed malaria (PNLP, 2012). With an incidence rate of 217.17‰, the Adamawa region is one of the hardest hit by the disease, after the East (292.46‰), North (241.24‰) and West (217.93‰) regions. U5 children pay the brunt of malaria in the Adamawa region and represent 71% of all malaria deaths [2].
Since April 2001, WHO recommends the use of artemisinin-based therapies (ACTs) in countries with high resistance to antimalarial drugs such as chloroquine, sulfadoxine-pyrimethamine and amodiaquine [5]. Given the high resistance to chloroquine in Cameroon, the government introduced ACTs in the malaria treatment policy in mid-2006 [6].
Malaria control policy in Cameroon relies heavily on the objectives of the Global Partnership "Roll Back Malaria" (RBM) [7]. Thus, the fight against malaria in Cameroon has three main areas: (i) prevention, (ii) management of cases and (iii) communication for behavior change. Alongside, there are associated support areas: monitoring and evaluation, training and operational research, managerial process and governance [7].
One of the major barriers to improving accessibility to health facilities in sub-Saharan Africa has been the presence of user fees, especially for the poorest households [8]. Evidence that user fees impede access to health care, particularly for poor and vulnerable population groups have been documented by many scholars [9]. So too is the case related to the positive impact of user fee abolition in increasing health service utilization [8].
Access to free diagnoses and treatments have been shown to be a major determinant in malaria control [10] and despite some evidence, many countries still rely on user fees for financing healthcare [11]. More specific evidence on the sound effects of user fee elimination is still needed [12,13].
In Cameroon, three quarters of sick people do not consult a health facility and the financial barrier is the reason given by half of them [14]. Thus, in a setting of extreme poverty, direct payments are an obstacle to the use of health services, and may be an important contributing factor to the poor health outcome, especially that of vulnerable groups such as children. It is in this context that the Cameroonian government launched in February 2011 the exemption of the under-fives' simple malaria treatment policy.
User fees removal of the under-fives’ simple malaria treatment in Cameroon:
User fees removal apply on consultations and treatment kits. The treatment kit includes artesunate-amodiaquine (25+67.5 mg and 50+135 mg) and paracetamol 100 mg.
Treatment is due after diagnosis of uncomplicated malaria after free consultation done by qualified health personnel.
When conditions are favorable, malaria diagnosis could be confirmed by a thick blood or a rapid biological test.
The dispensation is made on the basis of a drug prescription duly completed and signed by qualified health personnel in the child medical record.
Source: Extract of the decision No: 0032/MINSANTE/CAB/, January 24, 2011
This study aimed at assessing the main effect of the exemption policy on services utilization fifteen months after its implementation.
Methods
Study design
A concurrent mixed-method research [15,16] using time series data collected in July 2011 and April 2012, and qualitative data collected in April 2012 was conducted.
The study was restricted to the Adamawa region since this region is located in the unstable and long transmission stratum, halfway between the Sahelian zone and the large southern part of the country. It is therefore a diagonal figure of the malaria transmission of the two large southern and northern Cameroon.
In light with the study objective, we targeted:
(1) Health facilities regardless of their status (public, private) and their level of service (integrated health center, medicalized health center, district hospital) on the supply-side; and
(2) The beneficiaries met in the community and out of health facilities on the demand side.
Sampling
Sampling of health facilities used the list provided by the Regional Delegation of Public Health of the Adamawa region and consists of all functional health facilities (HF) in the region. A one degree stratified random sampling was used taking sector (private or public) as strata and crossing it by the level of care (District Hospital, Medicalized Health Center and Integrated Health Center).To assure sampling representativeness, the research team agreed to include at least 2/5 of the total of health facilities. Ultimately, out of the 91 health facilities, 39 were visited in July 2011 and 43 in April 2012.
For each phase, an average of 04 beneficiaries were conveniently selected and interviewed in each selected HF as follows: one U5, one pregnant woman, one woman of childbearing age (aged 15-49 years) and one man, came for medical consultation. In the community, 20 households in each randomly selected village in a health area with at least one selected HF were visited using the WHO's cluster survey method [17]. A total of 851 individuals were interviewed in July 2011 and 852 in April 2012.
Sampling for in-depth interviews was purposive and informants were selected according to criteria that allowed a maximum sampling variation. A total of 113 in-depth interviews with policy makers and service providers involved in the formulation and/or implementation of the policy, and beneficiaries (traditional and religious leaders, heads of associations, COSADI, parents of children) were conducted (Table 1).
| Sampling | 1st survey phase (July 2011) | 2nd survey phase (April 2012) | |
|---|---|---|---|
| Quantitative data | Health facilities | 39 (04 MHC, 11 private HC, 21 public HC, 02 DH, 01 private hospital) | 43 (04 MHC, 15 private HC, 21 public HC, 02 HD, 01 private hospital) |
| Health personnel | 76 | 85 | |
| Beneficiaries | 851 (150 exit interview, 701 household interview) | 852 (172 exit interview, 680 household interview) | |
| Qualitative data | In-depth interview | 113: SG MINSANTE, PNLS, CAPR, DRSP Adamaoua, head HF, community leaders (religious, traditional, administrative etc.), community agent relay,… etc. | |
Table 1: Summary of the study sampling
| Drugs received | ||||||
| All drugs (%) | No drug (%) | RR (no drug) | IC95% | |||
| Jul. 2011 | Ap. 2012 | Jul. 2011 | Ap. 2012 | |||
| Residence | ||||||
| Urban | 27.8 | 60 | 61.1 | 10 | - | |
| Rural | 17.6 | 28.6 | 45.9 | 20.6 | 2.7 | [1.5-3.7] |
| Well being | ||||||
| Poor | 14.3 | 24 | 62.7 | 32 | 1.6 | [1.1-2.2] |
| Mean | 20.6 | 38.1 | 44.1 | 14.3 | 1 | [0.7-1.4] |
| High | 26.1 | 37 | 34.8 | 11.1 | - | |
| Total | 19.6 | 32.9 | 48.9 | 19.2 | ||
Table 2: Distribution of beneficiaries of drugs among U5 treated for uncomplicated malaria, Adamawa region, Cameroon. April 2012.
| Socio -demographic Characteristics | Beneficiaries informed of the exemption policy (%) | Respondents (n) |
|---|---|---|
| Residence | ||
| Urban | 29.1 | 227 |
| Rural | 35.5 | 623 |
| Educational level of the family head | ||
| None | 23.7 | 312 |
| Primary | 32.6 | 325 |
| Secondary | 50 | 180 |
| Tertiary | 51.5 | 33 |
| Well-being | ||
| Poor | 23.9 | 284 |
| Mean | 35.7 | 283 |
| High | 41.3 | 283 |
| Total | 33.7 | 850 |
Table 3: Distribution of beneficiaries informed of the exemption policy for U5 uncomplicated malaria treatment, Adamawa region, Cameroon. April 2012.
| Socio-demographic Characteristics | Average cost (FCFA) | Direct cost (FCFA) | Total direct cost (FCFA) | |||||
|---|---|---|---|---|---|---|---|---|
| Medical booklet | Consultation | Laboratory | ACT | medical | non medical | |||
| Residence | ||||||||
| Urban | 209 | 482 | 582 | 1834 | 3106 | 323 | 3429 | |
| Rural | 335 | 580 | 340 | 1642 | 2896 | 851 | 3748 | |
| Welfare | ||||||||
| Poor | 336 | 516 | 280 | 1721 | 2852 | 1050 | 3902 | |
| Mean | 250 | 560 | 300 | 925 | 2035 | 710 | 2745 | |
| high | 308 | 605 | 560 | 2019 | 3491 | 413 | 4011 | |
| Total | 309 | 559 | 391 | 1682 | 2941 | 739 | 3680 | |
Table 4: Distribution of beneficiaries informed of the exemption policy for U5 uncomplicated malaria treatment, Adamawa region, Cameroon. April 2012.
Data collection, processing and analysis
A training session for interviewers including a pilot test phase questionnaires were organized before each collection phase in July 2011 and April 2012.
The qualitative data collected were transcribed, entered in MSWORD RTF and imported into the Atlas Ti.6 software coding and analysis. The analysis process was iterative and flexible. The concepts, categories and their properties and dimensions were identified by induction. Dissonant elements of the main findings were retained or rejected after an internal discussion within the research team.
Quantitative data were obtained using specific questionnaires for each target. Data on the health facilities were collected over twelve months before and thirteen months after the implementation of the exemption policy. Data on morbidity were collected the last four weeks preceding the survey.
After data collection, the questionnaires were coded, entered by trained staffs under CsPro software in a single control approach in the first phase and double in the second to minimize data entry errors. The resulting databases were cleared and analyses were performed in Stata 10.0 (College Station, Texas 77845 USA) and SPSS 17.0 (South Wacker Drive, Chicago, IL 60606-6412). Risk ratio (RR) and student test were used to estimate the intervention effects.
Households were categorized into three groups of economic welfare, (i) low, (ii) medium and (iii) high, following the approach proposed by Owen O'Donnell [18]. In the absence of data on income or consumption expenditure of households, a proxy was used to measure living standards by calculating a composite index using principal component analysis [19].
Ethical consideration
The research protocol was jointly developed between the Operational Research Unit of the Ministry of Public Health, the National Institute of Statistics and the UNICEF office in Cameroon. The data collected did not involve any biological sample. The principle of anonymity was explained to respondents and consent was required before any data collection.
Results
Health services utilization
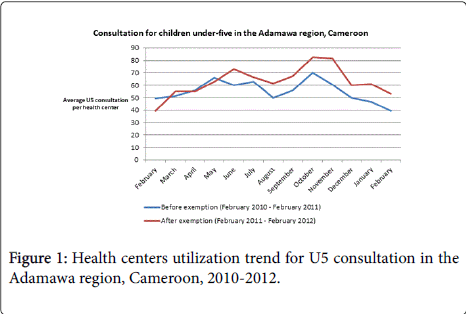
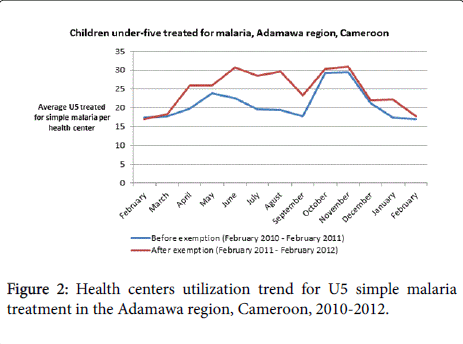
Consultations of the general population and overall consultations of the U5 (all causes) increased to about 10% during the year 2011 (after the exemption policy) compared to the year 2010 (before the exemption policy).
The average number of consultations for simple malaria cases in children U5 increased in the months following the launch of the policy then started declining from September 2011 to reach the level before the implementation of exemption.
According to various stakeholders, the increase in services utilization was due to the policy, as some of them quote:
“There are many changes since now huh, if the child now heated a little, he is directly brought to the hospital. We are expecting because it's free. Ehein. Ehein. That's it. So attendance increased.”
“It has really increased. I mentioned the case of poverty, people do not come. But when they learned that there is free, everyone comes. So if there is a child who has a little discomfort moms rush to the hospital.”
Source: in-depth interviews.
Benefits of the policy
The proportion of households who benefited free treatment for U5 uncomplicated malaria treatment twelve months after the policy significantly increased among all social categories of the population.
Between July 2011 and April 2012, the indicators related to total access to the exemption policy improved significantly. In fact, the proportion of U5 who was totally exempted from payment of drugs for uncomplicated malaria treatment increased from 19.6% to 32.9% at 4 and 12 months after the implementation of the policy.
In contrast there was no effect in reducing inequalities among social groups: the rural and lowest socio-economic well-being households were those who benefit the least from the exemption measure (RR respectively 2.7, 1.6).
There is a close correlation between the level of education of the population, their level of socio-economic well-being and their willingness or not to be aware of the policy. The higher the level of education or level of socio-economic well-being, the higher the probability of being informed (P-value=0.000 in each case).
Informed households significantly benefited more from this policy as compared to the uninformed, with an increasing inequality over time. Indeed, four months after the start of the implementation of the policy, as opposed to the uninformed household, the informed were about three times more likely to benefit from the policy (RR=2.7). Six months after, this chance was five times higher (RR=5.4).
Informal costs
Before the implementation of the exemption policy, the official cost to access the treatment of uncomplicated malaria for the U5 was 325 FCFA (0.67 $USA) at the level of the health center. The official cost with the introduction of the exemption policy was zero.
After the introduction of the policy, two thirds of U5 who used health services for uncomplicated malaria paid for the treatment. On average, these disbursements were 2940 FCFA (6 $USA) for direct costs. The major part of this cost was made on the acquisition of ACT (1680 FCFA/3.5 $USA).
"Not only must thank the president, but he must know that we still pay the drugs in the hospital. Whether children less than 5 years or more! "
"Well, I thought when the child was, upon consultation, it must be free and then after consultation, it must be given free medicines. But for me, when I went with my child, I’ve always been asked to pay. People ask me 4000, 5000 (8, 10 $USA), and that is only for the consultation"
Source: In-depth interview
Staffs coping strategies
Several coping mechanisms have been developed by care providers to address different shortfalls induced by the policy such as the sale of "free medicine", unsystematic patient registration, classification of cases of uncomplicated malaria as complicated cases or classification of children U5 in the over 05 years category.
Most providers admit to not be satisfied on the way in which the policy was designed, and advanced the loss of income generated by such a decision, but also the fact of not having been involved in its design and planning.
As some players below raised, the services offered by providers are directly related to the amount of interest saved or lost:
"You know it's not everyone who will agree with the decision of the President of the Republic. For some, it makes a kind of hollow in the pocket if they don’t sell drugs. Because you know that drug in the hospital is not sold at a single price."
"I told you earlier that there were some households, when they get there, they tell us that the presidential measures are not well implemented. People continue to pay and almost all malaria cases are now complicated cases."
Source: In-depth interview.
Discussion
The decision to exempt the uncomplicated malaria treatment for U5 in Cameroon resulted in an increase services utilization of general consultations and U5 consultations. In contrast, consultations of malaria (and uncomplicated malaria) for U5 increased only during the months following the launching of the policy.
The results obtained in other countries are somehow heterogeneous, as the experience of Burkina Faso where the change in utilization was very diverse depending on the district, or the experience of Niger where there was a smaller increase on the utilization of services for U5 in districts where attendance was already low [20].
The figure thus observed with our data shows that the increase in the health service utilization was indistinguishable with the announcement effect and has not really been sustained over time. In addition, rural households and those with low socio-economic wellbeing are those who benefit the least. A recent study found a persistence of inequity of access to health care between rural and urban households during implementation of public policies in Equatorial Guinea [21].
Exemption policies should not only increase the ability to access care, but should also ensure that the most vulnerable can actually benefit. It is essential to develop strategies to enable the most disadvantaged social groups (rural, low socio-economic well-being, less educated) to benefit from this policy.
In Uganda [22], Ghana [23] and South Africa [24], caregivers felt that user fees abolition mainly benefited the poor. In Ghana, the proportion of primary care delivered increased in each socioeconomic quintile, but the largest increases were observed in the two poorest [25]. In Uganda, the largest increases in the use of health services after abolition were among the poor [26,27].
By questioning the essence of the exemption policy in Cameroon, beneficiaries welcome and appreciate the opportunity, but when discussing the implementation phase, other vision more sententious, challenges and criticizes its effectiveness, citing reasons directly and mainly due to the behavior of providers and their ability to organize their service. This, far from encouraging the utilization of health facilities has reversely led to rejections and even frustrations, bringing some beneficiaries to move to other health facilities and pharmacies where these services were not free.
In countries that initiated free care, beneficiaries of health services were satisfied with the measures [28], and were annoyed when these policies were suspended or malfunctioned, creating tensions with health personnel [24,29,30].
The situation is different for the staff. Spontaneously interviewed, providers said they were satisfied with the policy. But pursuing a deeper discussion, the emerging trend is that preserving their interests was an element that weighed heavily in their behavior during the implementation of the policy. Most providers admit not to be satisfied on how the measure was designed and point out loss of revenues generated by such a decision, but also the fact of not having been involved in its design and planning.
Health professionals in Ghana appreciated the abolition of fees [23,30], however, the effects on job satisfaction vary considerably [23,30]. Studies in Uganda mention the demoralization of staff [22,28]. In South Africa, nurses interviewed were ambivalent [24]. When they felt they had done professionally their duty as free health care meant "to be able to help more patients," they also complained they had been neglected by policy makers.
The evidence from this research suggests that households still continue to pay to access, only third of households received free treatment and this policy had benefited mainly the least deprived.
In any case, due to the persistence: (a) direct cost not included in the exemption policy (laboratory tests and products not included in the kits), (b) indirect costs (transport, food), (c) illicit costs (billing undue, illegal drug sales or favors, etc.), some households remain excluded from care.
Similar results were reported in Burkina Faso [31] where exemption or subsidy have never really been free for the users, they continue to pay, but significantly less than before the policy.
Several coping strategies developed by the staff were identified. Staff continued to sell free drugs, sometimes registering uncomplicated malaria cases as complicated ones, or simply by not registering the patient. In fact, conscious that the number of malaria cases and ACT consumption have to be adequate and would be subject to suspicion during supervision if not the case, the staffs preferred to under notify the uncomplicated malaria cases in order to sell their own ACT, leaving stocks of provided drug to expire. In other cases, staff classified the U5 in the category of more than 5 years, allowing them to charge fearlessly consultation and supposed free medicines.
Similar practices are reported elsewhere. In Senegal, Niger and Mali, some health facilities restored payments for legally free services, while others increased the cost of paid services. Under the Sesame plan in Senegal, patients are prescribed drugs normally free but have to buy them in private pharmacies. We are witnessing similar strategies in Burkina Faso under the pretext of shortages. In Niger, facing the difficulties of distribution of the central purchasing agency, several health facilities were supplied in Nigeria, importing informally uncontrolled products [13].
As of today in Cameroon, there is no clear direction on how the losses caused by the policy must be compensated. The success of a user fees abolition policy relies greatly on the effectiveness of the compensation process of the health facilities, whether financially, human resources or drugs and consumables.
A transparent and robust transfer system of resources to health facilities to compensate for loss of income and cover new spending is crucial. The resources must reach health facilities where services are provided within a reasonable time. This requires the definition of appropriate pricing of services and clear channels for the transfer of funds and/or drugs.
Messen et al. identify a compensation approach based on inputs in Liberia, outputs in Ghana and Burkina Faso, and a mixed approach in Senegal [32]. Not satisfied with the approach based on inputs in the past, Burkina Faso decided that health facilities should be compensated according to their activity (output-based payment). This payment includes the cost of drugs and supplies, but also all other inputs, including a bonus for the staff and transport for the reference case [33].
It might be that Cameroon has implicitly chosen an "input-based" approach for drugs compensation, nevertheless the management of this system remains unclear and its effectiveness is controversial by implementers.
It is important to draw the necessary adjustments to the system to mitigate the identified adverse impacts and maximize the benefits of the policy. In this sense, we must rely on the good practice developed elsewhere, for example through proper planning of the drug supply, deployment of additional staff and incentives. This should be planned well in advance [34].
When exemption policies are well designed, implemented with the necessary accompanying measures and properly funded, they improve people's access to health care. However, insufficient funding may lead households to spend more for their health care.
The particularity of our study is that it is based on a mixed method research, combining both quantitative and qualitative approaches. In our knowledge, very few studies have done so. It combines data from health facilities, data from community surveys, and data from different stakeholders from all levels of the health system. This gives a comprehensive understanding of this policy both on the supply and demand, and gives findings greater significance, but also several bias inherent to the method used.
In interpreting the time series data like ours, the more the series is collected over a long period, the more information on the pattern of before and during the policy change, as well as the possible presence of seasonal effects and if or not the policy has a lasting effect on the result is accurate. Our data are limited to one year before and one year of the implementation of the exemption policy and it would be difficult to exclude autocorrelation, seasonal or non stationarity bias [35].
The interpretation of our data collected from the management tools in the context of routine is subject to the usual limitations of any observational study, including missing values, incomplete or inconsistent. Collecting information on financial data proved very delicate, limiting some of our estimates or making them inaccurate. However, we have recruited a sufficiently broad range of participants in order to obtain a maximum variation of respondents and to draw some general conclusions.
A point to consider is the importance of going beyond utilization to measure health outcomes in the evaluation of health policy [36]. Considering that a policy process lead to a complex causal chain, it is crucial to measure outcomes that reflect its final objective. A key lesson for future research, and one that concurs with the conclusions offered by Card et al. [37]. is that identifying an impact of health care financing reforms on health outcome is challenging. Progress will call for innovative and rigorous research designs that are powered to seize any effects in multiple dimensions of health [38].
The presidential decision to remove user fees for U5 uncomplicated malaria treatment in Cameroon aims to improve access to health services and reduce inequities.
This study shows that the policy improved health services utilization, however, the measure failed to reduce inequalities among social groups.
Difficulties observed in the implementation were mainly related to poor providers’ adherence, largely due to the absence of accompanying measures, inadequate supervision and failure to involve them in the formulation. This had encouraged the development of coping strategies, resulting in the persistence of informal costs for a good part of the population.
It is also important to observe these dysfunctions of the implementation through the prism of a broader failure of the health financing architecture. Efforts to remove financial barriers remain highly balkanized in the country. Hence there is a need to develop a more coherent policy system of health financing in Cameroon to strengthen the health system as a whole. There is a window of opportunity offered by political reform going on in the country. A step in the right direction would for be for example to build a bridge between the exemption policy and the performance-based financing program which has been recently launched in the country.
Acknowledgements
We are grateful to the officials of the ministry of health in Yaoundé and Ngaoundéré region for their support and all the information shared. We also thank UNICEF who funded the study. We are very thankful to all the persons who agreed to be interviewed for the purpose of the surveys. Sincere thanks to interviewers teams who facilitated the work.
Conflict of Interest
We have no conflict of interest to declare. All the ideas expressed in this article represent those of the authors and not of their organizations and institutions
Author Contributions
Conceived and designed the study: IS EB JCK ATN. Performed the field work: IS EB JCK ATN. Analyzed the data: JCK ATN. Wrote the paper: IS HAY.
References
- WHO (2010) World Health Organization, Fact sheet No. 94. 2010.
- Programme National de Lutte contre le Paludisme. Rapport d’activité du Programme de Lutte cintre le Paludisme 2011(2012).
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, et al. (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet Lond Engl 379:2151-2161.
- Inter-agency Group for Child Mortality Estimation. Levels & Trends in Child Mortality. (2012).
- WHO (2006) WHO briefing on Malaria Treatment Guidelines and artemisinin monotherapie
- Ministère de la Santé Publique (2006) Lettre circulaire du ministre de la santé D36-26/LC/MSP/SG/DPM/SDM du 08 mai 2006.
- Ministère de la Santé Publique (2007) Plan stratégique national de lutte contre le paludisme au Cameroun 2007-2010.
- Ponsar F, Van Herp M, Zachariah R, Gerard S, Philips M, et al. (2011) Abolishing user fees for children and pregnant women trebled uptake of malaria-related interventions in Kangaba, Mali. Health Policy Plan 2:ii72-83.
- Gilson L, McIntyre D (2005) Removing user fees for primary care in Africa: the need for careful action. BMJ 331: 762-765.
- Nkuo Akenji TK, Ntonifor NN, Ching JK, Kimbi HK, Ndamukong KN, et al. (2005) Evaluating a malaria intervention strategy using knowledge, practices and coverage surveys in rural Bolifamba, southwest Cameroon. Trans R Soc Trop Med Hyg99:325-332.
- Ridde V (2006) Users fees and worst off: it's time to find a solution.J Epidemiol Community Health 60: 398.
- Lagarde M, Palmer N (2011) The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database Syst Rev 2011.
- Ridde V, Morestin F (2009) Recension des écrits scientifiques sur l’abolition des frais aux usagers dans les services de santé en Afrique?: document de travail.
- Commeyras C, Ndo JR, Merabet O, Koné H, Rakotondrabé FP (2005) Étude de l’accessibilité et des déterminants de recours aux soins et aux médicaments au Cameroun. I. Élaboration et validation de la méthode d’analyse de l’interface offre/demande en santé. Cah Détudes Rech Francoph Santé 15:161-166.
- Dowding D (2013) Best Practices for Mixed Methods Research in the Health Sciences John W. Creswell, Ann Carroll Klassen, Vicki L. Plano Clark, Katherine Clegg Smith for the Office of Behavioral and Social Sciences Research; Qualitative Methods Overview Jo Moriarty. Qual Soc Work 12:541-545.
- Pluye P, Hong QN (2014) Combining the Power of Stories and the Power of Numbers: Mixed Methods Research and Mixed Studies Reviews. Annu Rev Public Health 35:29-45.
- Henderson RH, Sundaresan T (1982) Cluster sampling to assess immunization coverage: a review of experience with a simplified sampling method. Bull World Health Organ 60:253-260.
- Xu K (2008) Analysing health equity using household survey data: a guide to techniques and their implementation. Bull World Health Organ86:816.
- Filmer D, Pritchett LH (2001) Estimating wealth effects without expenditure data--or tears: an application to educational enrollments in states of India. Demography 38:115-32.
- Ridde V, Diarra A (2009) A process evaluation of user fees abolition for pregnant women and children under five years in two districts in Niger (West Africa). BMC Health Serv Res 9:89.
- Romay-Barja M, Jarrin I, Ncogo P, Nseng G, Sagrado MJ, et al. (2015) Rural-Urban Differences in Household Treatment-Seeking Behaviour for Suspected Malaria in Children at Bata District, Equatorial Guinea. PloS One 10:e0135887.
- Burnham GM, Pariyo G, Galiwango E, Wabwire-Mangen F (2004) Discontinuation of cost sharing in Uganda.Bull World Health Organ 82: 187-195.
- Witter S, Arhinful DK, Kusi A, Zakariah-Akoto S (2007) The experience of Ghana in implementing a user fee exemption policy to provide free delivery care. Reprod Health Matters 15:61-71.
- Walker L, Gilson L (2004) ‘We are bitter but we are satisfied’: nurses as street-level bureaucrats in South Africa. Soc Sci Med 59:1251-61.
- Penfold S, Harrison E, Bell J, Fitzmaurice A (2007) Evaluation of the delivery fee exemption policy in ghana: population estimates of changes in delivery service utilization in two regions. Ghana Med J 41:100-9.
- Deininger K, Mpuga P (2005) Economic and Welfare Impact of the Abolition of Health User Fees: Evidence from Uganda. J Afr Econ 14:55-91.
- Nabyonga J, Desmet M, Karamagi H, Kadama PY, Omaswa FG, et al. (2005) Abolition of cost-sharing is pro-poor: evidence from Uganda.Health Policy Plan 20: 100-108.
- Kajula PW, Kintu F, Barugahare J, Neema S (2004) Political analysis of rapid change in Uganda’s health financing policy and consequences on service delivery for malaria control. J Health Plan Manag.
- Witter S, Adjei S (2007) Start-stop funding, its causes and consequences: a case study of the delivery exemptions policy in Ghana. Int J Health Plann Manage 22:133-43.
- Witter S, Kusi A, Aikins M (2007) Working practices and incomes of health workers: evidence from an evaluation of a delivery fee exemption scheme in Ghana.Hum Resour Health 5: 2.
- Ridde V, Bicaba A (2009) Revue des politiques d’exemption/subvention du paiement au Burkina Faso: la stratégie de subvention des soins obstétricaux et néonataux d’urgence [Internet]. Accès aux soins de santé & évaluation de programmes - Access to healthcare & program evaluation.
- Meessen B, Hercot D, Noirhomme M, Ridde V, Tibouti A, et al. (2011) Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Policy Plan 26:ii16-29.
- Richard F, Witter S, de Brouwere V (2010) Innovative approaches to reducing financial barriers to obstetric care in low-income countries.Am J Public Health 100: 1845-1852.
- Hercot D, Meessen B, Ridde V, Gilson L (2011) Removing user fees for health services in low-income countries: a multi-country review framework for assessing the process of policy change. Health Policy Plan. 26:ii5-15.
- Lagarde M (2012) How to do (or not to do) …Assessing the impact of a policy change with routine longitudinal data. Health Policy Plan 27:76-83.
- Powell-Jackson T, Hanson K, Whitty CJM, Ansah EK (2014) Who benefits from free healthcare? Evidence from a randomized experiment in Ghana. J Dev Econ 107:305-19.
- Card D, Dobkin C, Maestas N (2009) DOES MEDICARE SAVE LIVES?Q J Econ 124: 597-636.
- Finkelstein A, McKnight R (2008) What did Medicare do? The initial impact of Medicare on mortality and out of pocket medical spending. J Public Econ 92:1644-68.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 11744
- [From(publication date):
December-2015 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 10793
- PDF downloads : 951