Research Article Open Access
Religious Beliefs towards the End of Life among Elderly Patients with Chronic Heart Failure and the Relationship with End-Of-Life Preferences
Daisy J.A. Janssen1,2*, Josiane J. Boyne3, Lucas Jörg4, Matthias E. Pfisterer5, Hans Rickli6 and Hans-Peter Brunner-La Rocca5,71CIRO, Centre of Expertise for Chronic Organ Failure, Horn, The Netherlands
2Centre of Expertise for Palliative Care, Maastricht University Medical Centre (MUMC+), Maastricht, The Netherlands
3Department of Patient & Care, Maastricht University Medical Centre (MUMC+), Maastricht, The Netherlands
4Clinic of Cardiology, University Hospital Liestal, Switzerland
5Department of Cardiology, University Hospital Basel, Switzerland
6Department of Cardiology, Kantonsspital St.Gallen, Switzerland
7Department of Cardiology, Maastricht University Medical Centre (MUMC+), Maastricht, The Netherlands
- *Corresponding Author:
- Daisy J.A. Janssen
MD PhD, Department of Research and Education
CIRO, centre of expertise for chronic organ failure
Hornerheide 1, 6085 NM Horn, The Netherlands
Tel: +31 475 587 686
Fax: +31 475 582 618
E-mail: daisyjanssen@ciro-horn.nl
Received date: January 05, 2016; Accepted date: January 18, 2016; Published date: January 21, 2016
Citation: Janssen DJA, Boyne JJ, Jörg L, Pfisterer ME, Rickli H, et al. (2016) Religious Beliefs towards the End of Life among Elderly Patients with Chronic Heart Failure and the Relationship with End-Of-Life Preferences. J Palliat Care Med 6:244. doi:10.4172/2165-7386.1000244
Copyright: © 2016 Janssen DJA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Religious beliefs may influence end-of-life decision-making among patients with Chronic Heart Failure (CHF). Objectives of the current longitudinal observational study were: 1) to explore whether and to what extent preferences for life-sustaining treatments and willingness to trade survival time for excellent health are influenced by religious beliefs among elderly patients with CHF; and 2) to explore whether and to what extent religious beliefs change towards the end-of-life among elderly patients with CHF. Methods: This longitudinal observational study included 427 elderly patients with CHF of the TIME-CHF study (69% of the original sample). Patients were recruited in several hospitals in Switzerland and Germany. Faith, religious beliefs (Religion Questionnaire), preferences for Cardiopulmonary Resuscitation (CPR) and willingness to trade survival time for excellent health were assessed. The relationship between religious beliefs and preferences for CPR and willingness to trade survival time at baseline was explored. In addition, changes in religious beliefs between baseline and 12 months were explored among patients who died between 12 and 18 months. Results: Most patients were Catholic or Protestant. Atheist patients more often preferred ‘Do Not Resuscitate’ (DNR) than Catholic patients (p=0.03). Patients with full agreement with statements of the Religion Questionnaire were less likely to prefer DNR than patients with no agreement (p<0.05). There was no relationship between faith or religious beliefs and willingness to trade survival time for excellent health (p>0.05). The belief in afterlife increased among patients who died between 12 and 18 months (p=0.04). Conclusions: This study showed a limited relationship between religion and preferences regarding CPR in patients with CHF. Religious beliefs may change towards the end of life. Therefore, exploring religious beliefs and the influence on preferences for life-sustaining treatments as part of advance care planning is needed.
Keywords
Religion; Spirituality; Life-sustaining treatment preferences; Advance care planning; Advance directives; Living will; Faith
Introduction
The palliative care needs of patients with advanced chronic heart failure (CHF) have been increasingly recognized [1]. Addressing spiritual issues is an important component of palliative care [1]. Indeed, religion or spirituality was related with less fear about dying [2]. Moreover, patients with CHF and their informal carers have expressed a need for spiritual support [3]. Religious beliefs may increase towards the end-of-life [4], but this has not yet been explored in a Western-European CHF population. Knowledge concerning religious beliefs and changes in religious beliefs towards the end-of-life is needed for the provision of spiritual support as part of palliative care for patients with CHF.
Advance care planning (ACP) is another important component of palliative care [1]. ACP is needed to prepare patients and their loved ones for and guide them through the process of decision-making about life-sustaining treatments and end-of-life care [5]. A previous analysis of the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF) showed a relationship between resuscitation preference and younger age, male sex, lower symptoms of depression, being married, less orthostatic response, higher left-ventricular ejection fraction, no history of anaemia and history of syncope [6]. However, the relationship between religious beliefs and preferences for life-sustaining treatments in CHF remains unknown. A study among cancer patients has shown that religion is related with a preference for treatments to extent life [7]. A study including US patients with cancer, COPD or CHF showed mixed results. Patients who reported to grow closer to God and growing spirituality were more willing to undergo life-sustaining treatments. However, a relationship between willingness to undergo life-sustaining treatments and other dimensions of religiousness was lacking [8]. Naghi et al. [9] showed that realistic goals and expectations can be affected by spirituality in patients with CHF and concluded that spirituality should be discussed in the context of ACP and may provide the framework that patients use to accept the realism of death in the relatively near future. However, understanding the relationship between religious beliefs and preferences regarding life-sustaining treatments is needed to support patients in the process of decisionmaking.
Therefore, the objectives of the current longitudinal observational study were: 1) to explore whether and to what extent preferences for life-sustaining treatments and willingness to trade survival time for excellent health are influenced by religious beliefs among elderly patients with CHF; and 2) to explore whether and to what extent religious beliefs change towards the end-of-life among elderly patients with CHF. We hypothesized a priori that stronger religious beliefs are related with a preference to undergo life-sustaining treatments among elderly patients with CHF. In addition, we hypothesized that religious beliefs will increase towards the end-of-life in these patients.
Methodology
Design
The current study is a secondary analysis of the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF) [10]. The methodology of this trial has been described in detail before [10]. In short, in this multicentre randomized controlled trial an intensified N-terminal-pro-B-type natriuretic peptide (NT-BNP) guided treatment was compared with a standard symptom-guided treatment. In total, 622 patients were recruited in several centres in Switzerland and Germany and were followed for 18 months. The study was approved by the Ethics Committees of every participating centre and patients provided their written informed consent. The study complies with the Declaration of Helsinki [10].
Participants
Eligible patients were 60 years of age or older; had symptomatic CHF (defined as New York Heart Association (NYHA) class II or more); had been hospitalized because of CHF in the previous year; and had a NT-proBNP-level of at least two times the upper limit of normal. Exclusion criteria were, among others, dyspnea not mainly caused by CHF or a life expectancy of less than three years because of diseases other than cardiovascular [10].
Measurements
Measurements performed at baseline and included in the current analysis are: demographics (age; sex; marital status); clinical characteristics (Body Mass Index (BMI); smoking status; cause of CHF; left-ventricular ejection fraction; NT-BNP; NYHA class; comorbidities (Charlson Comorbidity Index [11])); disease-specific quality of life (Minnesota Living with Heart Failure Questionnaire (MLHFQ) [12]); and symptoms of depression (Geriatric Depression Scale Short Form (GDS-SF) [13]).
At baseline, patient’s faith was recorded: Protestantism, Catholic, Jewish, Islam, Christian Orthodoxy, other faith, or atheist. In addition, at baseline and after 12 months patients were asked to complete a seven-item Religion Questionnaire to assess religious beliefs. This questionnaire consists of validated components of two questionnaires concerning religion in general and the after-death belief [14,15]. Each item is scored on a six-point scale from 0 (not at all) to 5 points (fully agree).
At baseline, 12, and 18 months patients were asked for their Cardiopulmonary resuscitation (CPR) preference after explaining the meaning and circumstances of CPR. In addition, at baseline, 12 and 18 months a Time Trade-Off (TTO) tool [16] was used to explore whether patients were willing to trade survival time for time living in excellent health. Patients were asked whether they preferred living two years in their current health state or living one year in excellent health. If one year in excellent health was chosen, the patients were asked whether they would prefer two years in their current health state or six months in excellent health. If they preferred two years in the current health state, they were asked whether they would prefer two years in their current health state or 18 months in excellent health. These questions were continued until the point at which the choices were equivalent. This time point subtracted from 24 months is the number of months of survival time that the patient would be willing to trade [6,16]. CPR preferences and willingness to trade survival time at baseline, 12 and, 18 months were published before [6].
Statistics
Continuous data were checked for normality and are presented as mean (SD) or median (IQR). To answer the first objective, the proportion of patients preferring ‘Do Not Resuscitate’ (DNR) was compared between faiths (Protestant; Catholic; other faith; or atheist) using Chi Square tests. The proportion of patients preferring DNR or willing to trade survival time was compared between patients who responded “not at all” and patients who responded “full agree” to the items of the Religion Questionnaire using Chi Square tests. A Kruskall- Wallis test was used to compare the median (IQR) number of days willing to trade for excellent health between faiths (Protestant; Catholic; other faith; or atheist). In addition, the correlation was assessed between responses to the Religion Questionnaire and the number of days patients were willing to trade for excellent health using Spearman correlation coefficients. To answer the second objective, median scores for all items of the Religion Questionnaire were compared between baseline and 12 months using Wilcoxon signed ranks tests. The same analysis was done while including only patients who died between 12 and 18 months follow-up. A priori, a p-value of ≤0.05 was considered statistically significant. Statistics were done using IBM SPSS Statistics 21.
Results
Patient characteristics
In total, 427 patients (68.6% of the original sample) had valid data for the primary outcomes of this study (CPR preference and all items of the Religion Questionnaire) at baseline and were included in the cross-sectional analyses (objective 1).
Nineteen patients (3.1% of the original sample) had missing data for CPR preference, 60 patients (9.6% of the original sample) did not respond to any item of the Religion Questionnaire and 128 patients (20.6% of the original sample) did not respond to some items of the Religion Questionnaire. Age and left-ventricular ejection fraction were comparable for patients included and excluded from the current analysis (p>0.05).
Patients who were excluded because of missing data were more often female than included patients (47.2% versus 37.7%, respectively, p=0.03). In addition, the proportion of atheist patients was higher among excluded patients than among patients included in the current analysis (11.3% versus 5.9%, respectively, p=0.03). Between baseline and 12 months 68 patients (10.9% of the original sample) died. At 12 months follow-up, 249 patients (40.0% of the original sample) also had valid data for the Religion Questionnaire and were included in the longitudinal analyses (objective 2).
In general, patients were elderly with moderate to very severe CHF. Most patients were male and married or living with a partner. The majority was Catholic or Protestant. Other faiths were rarely reported. Atheism was reported by 5.9% (Table 1).
| Age (years) | 76.6 (7.5) |
| Male | 266 (62.3%) |
| Married / living with other | 262 (61.4%) |
| BMI (kg/m2)* | 25.9 (4.5) |
| Current smoker | 55 (12.9%) |
| Cause of HF | |
| CAD | 232 (54.3%) |
| DCM | 56 (13.1%) |
| HHD | 122 (28.6%) |
| Other | 17 (4.0%) |
| LVEF | 35.0 (13.0) |
| LVEF > 45% | 81 (19.0%) |
| NT-BNP (pg/mL) | 3503 (1808-6585) |
| NYHA class | |
| NYHA II | 107 (25.1%) |
| NYHA III | 266 (62.3%) |
| NYHA IV | 54 (12.6%) |
| Charlson Comorbidity Index (points) | 3.1 (1.7) |
| MLHFQ (points)† | 41.3 (19.8) |
| GDS-SF (points)† | 4.4 (3.1) |
| Faith | |
| Protestantism | 179 (41.9%) |
| Catholic | 202 (47.4%) |
| Jewish | 2 (0.5%) |
| Islam | 1 (0.2%) |
| Christian Orthodoxy | 1 (0.2%) |
| Other | 10 (2.3%) |
| Atheist | 25 (5.9%) |
| Unknown | 7 (1.6%) |
n=427. *n=426. †n=425. Data reported as n (%), mean (SD) or median (IQR). Abbreviations: BMI=Body Mass Index; CAD=coronary artery disease; DCM, dilated cardiomyopathy; HHD, hypertensive heart disease; LVEF=Left-ventricular ejection fraction; NT-BNP=N-terminal- pro-B-type natriuretic peptide; NYHA=New York Heart Association; MLHFQ=Minnesota Living with Heart Failure Questionnaire; GDS-SF=Geriatric Depression Scale-Short Form
Table 1: Patient characteristics.
At baseline, a considerable part considered themselves as religious and/or felt supported by their religion (Table 2).
| 0 Not at all | 1 | 2 | 3 | 4 | 5 Full agreement | |
|---|---|---|---|---|---|---|
| I consider myself as religious | 67 (15.7%) | 29 (6.8%) | 74 (17.3%) | 67 (15.7%) | 53 (12.4%) | 137 (32.1%) |
| My religion helps me especially in case of worries and misfortune | 86 (20.2%) | 42 (9.8%) | 45 (10.5%) | 60 (14.1%) | 57 (13.3%) | 137 (32.1%) |
| If something bad happened, I had wondered why God would punish me | 216 (50.7%) | 44 (10.3%) | 42 (9.8%) | 54 (12.6%) | 26 (6.1%) | 45 (10.5%) |
| I believe that there is a God (or a higher power) | 48 (11.2%) | 14 (3.3%) | 27 (6.3%) | 31 (7.3%) | 44 (10.3%) | 263 (61.6%) |
| After death everything ends | 168 (39.4%) | 27 (6.3%) | 50 (11.7%) | 33 (7.7%) | 25 (5.9%) | 124 (29.0%) |
| There will be a rebirth (reincarnation) of the soul in another life | 207 (48.5%) | 38 (8.9%) | 44 (10.3%) | 38 (8.9%) | 27 (6.3%) | 73 (17.1%) |
| The resurrection of Jesus Christ gives some sense to my death | 112 (26.2%) | 31 (7.3%) | 45 (10.5%) | 36 (8.4%) | 43 (10.1%) | 160 (37.5%) |
n=427. Data reported as n (%)
Table 2: Religion Questionnaire–baseline.
Furthermore, most patients believed in a God or higher power. Many patients believed in afterlife. “The resurrection of Jesus Christ gives some sense to my death” was fully agreed with by more than onethird of the patients.
Relationship between religion and preferences for lifesustaining treatments and willingness to trade survival time
The proportion of patients preferring DNR was higher among atheist patients (56.0%) than among Catholic patients (32.2%). The proportion of patients preferring DNR was comparable for all other faiths (Figure 1).
We found no differences between faiths (including atheism) when including all patients with valid data for faith and DNR preference at baseline (n=592, p=0.06).
Patients reporting full agreement with the statements “I consider myself as religious”, “My religion helps me especially in case of worries and misfortune”, or “I believe that there is a God (or a higher power)” were less likely to prefer DNR than patients reporting “not at all” for these items (Table 3).
| DNR preference | p-value | ||
|---|---|---|---|
| I consider myself as religious | Not at all (n=67) | 38 (56.7%) | 0.01 |
| Full agreement (n=137) | 48 (35.0%) | ||
| My religion helps me especially in case of worries and misfortune | Not at all (n=86) | 45 (52.3%) | 0.02 |
| Full agreement (n=137) | 48 (35.0%) | ||
| If something bad happened, I had wondered why God would punish me | Not at all (n=216) | 92 (42.6%) | 0.88 |
| Full agreement (n=45) | 18 (40.0%) | ||
| I believe that there is a God (or a higher power) | Not at all (n=48) | 26 (54.2%) | 0.05 |
| Full agreement (n=263) | 99 (37.6%) | ||
| After death everything ends | Not at all (n=168) | 67 (39.9%) | 0.71 |
| Full agreement (n=124) | 53 (42.7%) | ||
| There will be a rebirth (reincarnation) of the soul in another life | Not at all (n=207) | 79 (38.2%) | 0.61 |
| Full agreement (n=73) | 31 (42.5%) | ||
| The resurrection of Jesus Christ gives some sense to my death | Not at all (n=112) | 48 (42.9%) | 0.28 |
| Full agreement (n=160) | 57 (35.6%) |
Data reported as n (%). Abbreviation: DNR=Do Not Resuscitate.
Table 3: Relationship between DNR preference and religious beliefs.
There was no relationship with other items of the Religion Questionnaire. In addition, there was no relationship between the proportion of patients willing to trade survival time and reporting “not at all” or “fully agree” with items of the Religion Questionnaire (all p>0.05).
In total, 29 patients had missing items on the TTO tool. Most patients (n=303, 71.0%) were unwilling to trade survival time for excellent health. The proportion of patients willing to trade survival time for excellent health was comparable for Protestant patients (n=41, 24.4%); Catholic patients (n=44, 23.3%); atheist patients (n=5, 21.7%); and patients with another faith (n=4, 36.4%) (p=0.79). The median (IQR) number of days willing to trade for excellent health was comparable for Protestant patients (0 (0-0)); Catholic patients (0 (0-0)); atheist patients (0 (0-0)); and patients with another faith (0 (0-182)) (p=0.83). Correlations between scores of all items of the Religion Questionnaire and the number of days willing to trade for excellent health were non-significant (p>0.05).
Change in religious beliefs toward the end-of-life
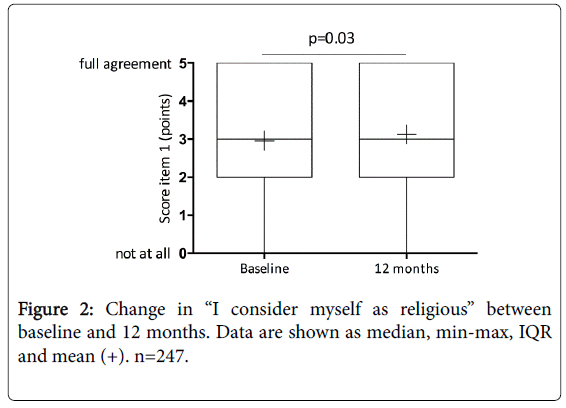
Agreement with the item “I consider myself as religious” increased between baseline and 12 months (p=0.03) (Figure 2). All other religious beliefs did not change between baseline and 12 months (p>0.05).
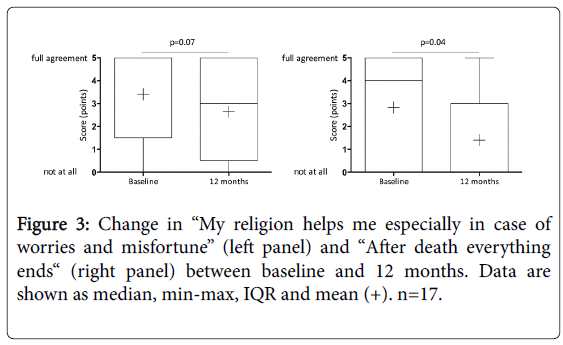
However, among patients who died between 12 and 18 months, the belief in the item “After death everything ends” decreased significantly.
In addition, the agreement with the item “My religion helps me especially in case of worries and misfortune” tended to decrease (Figure 3). Other items did not change between baseline and 12 months (p>0.05).
Discussion
The current longitudinal study among elderly patients with moderate to very severe CHF showed a limited relationship between religion and preferences regarding CPR. Patients with full agreement with religious statements were less likely to prefer DNR than patients with no agreement with religious statements. We did not find a relationship between religion and willingness to trade survival time. Finally, the belief in afterlife may increase towards the end-of-life in patients with CHF.
Religion among patients with CHF
The present study shows that religion may be important for many elderly patients with CHF. Indeed, a large majority of the patients reported to believe in God or a higher power. A considerable part of the patients reported to experience support from their religion in case of worries and misfortune. Finally, a considerable number of patients believed in life after death. These findings are in accordance with a previous study among patients with CHF in the US [17]. This study showed relatively high levels of religiousness in the domains forgiveness, daily spiritual experience, belief in afterlife, religious identity, religious support, public practices, positive religious or spiritual coping. Daily religious experiences were related with less death anxiety [17]. Nevertheless, the relationship between religiousness and concerns about death is complex. While for some patients religiousness is associated with comfort and less concern about death, other patients experience religious struggle, which increases concerns about death [18]. Interestingly, in our patient population of elderly patients with advanced heart failure, DNR preference was lower in those with more religious belief. Moreover, we found a trend towards feeling less supported by religion in case of worries and misfortune towards the end-of-life. This suggests that religiousness might not lead to less death anxiety although we did not directly address this question in our patients. Therefore, this needs to be addressed in future studies.
Relationship between religion and preferences for lifesustaining treatments and willingness to trade survival time
Feeling religious, experiencing support from religion in case of worries, and believing in God or a higher power were related to some extent with more willingness to undergo CPR. There was, however, no relationship with other religious beliefs and no relationship between religious beliefs and willingness to trade survival time for excellent health. Thus, the overall influence of religious beliefs on end-of-life wishes was limited in our population of elderly patients with advanced CHF. This is in line with some, but not all previous studies. A study among African-American dialysis patients did not show a relationship between religious beliefs and preferences regarding life-sustaining treatments [19]. Moreover, a large US study with predominantly African American hospitalized patients found no relationship between advance directives or a DNR order and religious beliefs [20]. However, patients with stronger religious beliefs were more likely to have appointed a surrogate decision-maker [20]. In patients with cancer, a religious coping style was related with a low likelihood of having a living will and more life-prolonging treatments before death [21]. Another study among cancer patients showed that religion was related with a preference for life-sustaining treatments [7]. So, it seems that while religious beliefs may influence preferences for end-of-life care and life-sustaining treatments, this may vary between populations, different diseases, and individuals. Therefore, individual religious beliefs should be discussed as part of advance care planning and the influence on preferences for life-sustaining treatments and end-of-life care should be explored.
The current study suggests that CHF patients with a Catholic faith were less likely to prefer DNR than atheist patients. This finding should be interpreted with caution, while the number of atheist patients was low. Nevertheless, a relationship between faith and DNR preference had also been shown in other populations. For example, among nursing home residents in the US, a Jewish faith and reliance on God were related with willingness to undergo life-sustaining treatments [22]. Surrogate decision-makers of patients in a skilled nursing facility in Jerusalem with an Ultra-Orthodox, National-Religious, or Muslim affiliation were less likely than surrogates with a traditional or secular background to forego CPR [23]. Faith might also be related with the willingness to engage in advance care planning. A study among US outpatients with CHF, cancer or diabetesshowed that advance care planning discussions were the most common among Jewish respondents, while conservative Protestant respondents were the least likely to have had advance care planning discussions. Conservative Protestants had the strongest beliefs that God controls the end of life [24]. Therefore, in the process of advance care planning clinicians should discuss with their patients their faith and the influence of their faith on their treatment preferences. This may help in understanding patients values and their wishes for end-of-life care.
Changes in religious beliefs towards the end-of-life
Religious beliefs were in general stable over time in this study. We found a minor statistically significant increase in the item “I consider myself as religious”, which does not seem clinically relevant. This is in contrast with a recent study by Trevino et al. [25] among 43 patients after a myocardial infarction or a coronary artery revascularization bypass grafting (CABG). They showed an increased frequency of church attendance and prayer/meditation over time, a decreased experience of religious reverence and comfort, and a decrease in religious coping with their illness. Several dissimilarities might explain differences with the current study. Patients in the study from Trevino et al. [25] were younger, more often male, and most of them were Protestant. Moreover, patients had a myocardial infarction or had undergone CABG, while in the current study patients suffered from a chronic and often progressive disease.
Interestingly, among patients who died within six months the belief in afterlife significantly increased, whereas the experience of support from religion in case of worries and misfortune tended to decrease. Other religious beliefs did not change towards the end-of-life. A study from Park et al. [4] including 111 US patients with advanced CHF showed that shifting longevity estimates toward less time or uncertainty was related with increases in religious life meaning and forgiveness and a decrease in spiritual struggle. A major difference with the current study is that the relationship was assessed between religious beliefs and patients’ estimates of life expectancy, while in the current study the relationship was assessed with actual survival. Obviously, patients who died between 12 and 18 months might not have been aware of their poor prognosis, as patients with advanced CHF are frequently unaware of their prognosis [26]. So, while the current study suggests that religious beliefs may change towards the end-of-life in patients with CHF, future studies should further explore this issue to corroborate our findings. Such studies should take into account the patients’ estimates of their prognosis and should explore whether changes in religious beliefs influence completion at the end of life. Completion is seen by patients and their loved ones as an important component of a good death. Completion includes faith issues, spirituality and meaningfulness [27]. Therefore, discussing the meaning of religion with a dying patient and providing spiritual support if needed might facilitate achieving a good death. However, data about change in religious beliefs and the relationship with completion and achieving a good death in chronic diseases are lacking.
Spiritual care counselling may be warranted for patients with more complex spiritual needs. Collaboration of spiritual care counsellors with other healthcare providers in an interdisciplinary team is seen as a key factor to successful spiritual care [28].
Methodological Considerations
Several methodological issues should be considered in interpreting the results. First, in the current study, patients with faiths other than Catholic or Protestantism were underrepresented. Only a few patients were atheist, Muslim, or had another faith. The relationship between faith and preferences for life-sustaining treatments might have been stronger when a higher proportion of patients with other faiths had been included. Indeed, in most Muslims cultures, illness is considered as a whole-family affair. Family members may prefer to make decisions concerning life-sustaining treatments and end-of-life care and may be unwilling to forego life-sustaining interventions [29]. In addition, no Buddhist patients were included. A qualitative study among Thai patients with CHF has shown the important influence of Buddhism on the experience of living with CHF. For example, practicing Buddhism through meditation and prayer provided comfort, a sense of control and a renewed sense of happiness [30]. Whether and to what extent Buddhism influences life-sustaining treatment preferences among patients with CHF is, however, unknown. Second, the proportion of atheist patients was higher among excluded participants in the current analysis, because of missing data on the Religion Questionnaire. It’s reasonable to assume that if these participants had completed the Religion Questionnaire, the proportion of patients without or with low religious beliefs would have been higher and this might have influenced our results. Third, only 17 patients died between 12 and 18 months. Therefore, the fact that we did not find a statistically significant change in religious beliefs other than belief in afterlife could be explained by the limited sample size. Fourth, the present study included elderly patients with CHF and it remains unknown whether and to what extent the results are generalizable to younger CHF patients. Fifth, data were collected between 2003 and 2008 [31]. Nevertheless, this study shows previously unpublished data that merit consideration for clinicians in planning end-of life care for patients and their families. Finally, we used the German-language Religion Questionnaire. However, multiple instruments are available to assess religious beliefs, such as the Duke Religion Index, the Ironson-Woods Spirituality/Religiousness Index or the Beliefs and Values Scale [32]. The use of another instrument than the Religion Index might have changed our results. Moreover, standardization of questionnaires about religious beliefs is limited and should be considered in future studies.
Conclusion
This study showed a limited relationship between religion and preferences regarding CPR in patients with CHF. Patients with full agreement with religious statements are less likely to prefer DNR than patients with no agreement with religious statements. Belief in afterlife may increase towards the end-of-life. Therefore, exploring religious beliefs and the influence of the individual religious beliefs on preferences for life-sustaining treatments and end-of-life care as part of advance care planning is needed. The current study mainly included Catholic or Protestant patients. Future studies should explore the relationship between religious beliefs and preferences regarding lifesustaining treatments and end-of-life care among CHF patients with other faiths. In addition, future studies should further explore changes in religious beliefs towards the end-of-life in patients with CHF and the relationship with completion and achieving a good death.
Acknowledgements and Funding
We thank all TIME-CHF investigators for their role in the study. This work was supported by the Horten Research Foundation (Lugano, Switzerland; 55% of the study’s budget), and by smaller unrestricted grants from AstraZeneca Pharma, Novartis Pharma, Menarini Pharma, Pfizer Pharma, Servier, Roche Diagnostics, Roche Pharma, and Merck Pharma. The sponsors had no role in design of the current study; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
References
- Jaarsma T, Beattie JM, Ryder M, Rutten FH, McDonagh T, et al. (2009) Palliative care in heart failure: a position statement from the palliative care workshop of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 11: 433-443.
- Sacco SJ, Park CL, Suresh DP, Bliss D (2014) Living with heart failure: psychosocial resources, meaning, gratitude and well-being. Heart Lung 43: 213-218.
- Ross L, Austin J (2015) Spiritual needs and spiritual support preferences of people with end-stage heart failure and their carers: implications for nurse managers. J Nurs Manag 23: 87-95.
- Park CL (2008) Estimated longevity and changes in spirituality in the context of advanced congestive heart failure. Palliat Support Care 6: 3-11.
- Sudore RL, Fried TR (2010) Redefining the "planning" in advance care planning: preparing for end-of-life decision making. Ann Intern Med 153: 256-261.
- Brunner-La Rocca HP, Rickenbacher P, Muzzarelli S, Schindler R, Maeder MT, et al. (2012) End-of-life preferences of elderly patients with chronic heart failure. Eur Heart J 33: 752-759.
- Balboni TA, Vanderwerker LC, Block SD, Paulk ME, Lathan CS, et al. (2007) Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol 25: 555-60.
- Van Ness PH, Towle VR, O'Leary JR, Fried TR (2008) Religion, risk, and medical decision making at the end of life. J Aging Health 20: 545-559.
- Naghi JJ, Philip KJ, Phan A, Cleenewerck L, Schwarz ER (2012) The effects of spirituality and religion on outcomes in patients with chronic heart failure. J Relig Health 51: 1124-1136.
- Brunner-La Rocca HP, Buser PT, Schindler R, Bernheim A, Rickenbacher P, et al. (2006) Management of elderly patients with congestive heart failure--design of the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure (TIME-CHF). Am Heart J 151: 949-955.
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383.
- Riegel B, Moser DK, Glaser D, Carlson B, Deaton C, et al. (2002) The minnesota living with heart failure questionnaire: Sensitivity to differences and responsiveness to intervention intensity in a clinical population. Nurs Res 51: 209-18.
- Vaccarino V, Kasl SV, Abramson J, Krumholz HM (2001) Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 38: 199-205.
- Bruhn M, Grözinger A (2000) Impulse aus der ökumenischen basler kirchenstudie. Freiburg/Schweiz: Universitätsverlag Freiburg/Schweiz.
- Pargament KI, Kennell J, Hathaway W, Grevengoed N, Newman J, et al. (1988) Religion and the problem-solving process: Three styles of coping. Journal for the Scientific Study of Religion 27: 90-104.
- Stevenson LW, Hellkamp AS, Leier CV, Sopko G, Koelling T, et al. (2008) Changing preferences for survival after hospitalization with advanced heart failure. J Am Coll Cardiol 52: 1702-1708.
- Park CL, Lim H, Newlon M, Suresh DP, Bliss DE (2014) Dimensions of religiousness and spirituality as predictors of well-being in advanced chronic heart failure patients. J Relig Health 53: 579-590.
- Edmondson D, Park CL, Chaudoir SR, Wortmann JH (2008) Death without God: religious struggle, death concerns, and depression in the terminally ill. Psychol Sci 19: 754-758.
- Song MK, Hanson LC (2009) Relationships between psychosocial-spiritual well-being and end-of-life preferences and values in african american dialysis patients. J Pain Symptom Manage 38: 372-80.
- Karches KE, Chung GS, Arora V, Meltzer DO, Curlin FA (2012) Religiosity, spirituality, and end-of-life planning: a single-site survey of medical inpatients. J Pain Symptom Manage 44: 843-851.
- Maciejewski PK, Phelps AC, Kacel EL, Balboni TA, Balboni M, et al. (2012) Religious coping and behavioral disengagement: opposing influences on advance care planning and receipt of intensive care near death. Psychooncology 21: 714-723.
- Ejaz FK (2000) The influence of religious and personal values on nursing home residents' attitudes toward life-sustaining treatments. Soc Work Health Care 32: 23-39.
- Jaul E, Zabari Y, Brodsky J (2014) Spiritual background and its association with the medical decision of, DNR at terminal life stages. Arch Gerontol Geriatr 58: 25-29.
- Garrido MM, Idler EL, Leventhal H, Carr D (2013) Pathways from religion to advance care planning: beliefs about control over length of life and end-of-life values. Gerontologist 53: 801-816.
- Trevino KM, McConnell TR (2014) Religiosity and religious coping in patients with cardiovascular disease: change over time and associations with illness adjustment. J Relig Health 53: 1907-1917.
- Harding R, Selman L, Beynon T, Hodson F, Coady E, et al. (2008) Meeting the communication and information needs of chronic heart failure patients. J Pain Symptom Manage 36: 149-156.
- Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, et al. (2000) In search of a good death: observations of patients, families, and providers. Ann Intern Med 132: 825-832.
- Sinclair S, Mysak M, Hagen NA (2009) What are the core elements of oncology spiritual care programs? Palliat Support Care 7: 415-422.
- Al-Jahdali H, Baharoon S, Al Sayyari A, Al-Ahmad G (2013) Advance medical directives: a proposed new approach and terminology from an Islamic perspective. Med Health Care Philos 16: 163-169.
- Chiaranai C (2014) A phenomenological study of day-to-day experiences of living with heart failure: do cultural differences matter? J Cardiovasc Nurs 29: E9-17.
- Pfisterer M, Buser P, Rickli H, Gutmann M, Erne P, et al. (2009) Bnp-guided vs symptom-guided heart failure therapy: The trial of intensified vs standard medical therapy in elderly patients with congestive heart failure (time-chf) randomized trial. JAMA 301: 383-92.
- Monod S, Brennan M, Rochat E, Martin E, Rochat S, et al. (2011) Instruments measuring spirituality in clinical research: a systematic review. J Gen Intern Med 26: 1345-1357.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 11210
- [From(publication date):
January-2016 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 10225
- PDF downloads : 985