Research Article Open Access
Relevance between Alzheimer’s Disease Patients and Normal Subjects Using Go/No-Go Tasks and Alzheimer Assessment Scores
Koji Terasawa1*, Shotaro Misaki1, Yuki Murata1, Toshiaki Watanabe1, Saiki Terasawa2, Masao Okuhara3, Toshie Kobayashi4, Zang Yong5, Koki Nakajima6, Suchinda Jarupat Maruo7 and Keisuke Nakade81Faculty of Education, Shinshu University, Nagano, Japan
2Faculty of Electrical and Electronic Engineering, Shinshu University, Nagano, Japan
3Center of General Education and Humanities, Tokyo University of Science, Suwa, Chino, Japan
4Department of Early Childhood Education, Seisen Jogakuin College, Nagano, Japan
5Nagano Prefecture College, Nagano, Japan
6Matsumoto University, Matsumoto, Japan
7Faculty of Medicine Ramathibodi Hospital Mahidol University, Bangkok, Thailand
8Health and Welfare Department, Minowa Town Office, Kamiina, Japan
- *Corresponding Author:
- Koji Terasawa
Faculty of Education, Shinshu University
Nagano 380-8544, Japan
Tel: +81-26-238-4213
Fax: +81-26-238-4213
E-mail: kterasa@shinshu-u.ac.jp
Received Date: August 20, 2014; Accepted Date: September 18, 2014; Published Date: September 25, 2014
Citation: Terasawa K, Misaki S, Murata Y, Watanabe T and Terasawa S et al. (2014) Relevance between Alzheimer’s Disease Patients and Normal Subjects Using Go/No-Go Tasks and Alzheimer Assessment Scores. J Child Adolesc Behav 2:162. doi:10.4172/2375-4494.1000162
Copyright: © 2014 Terasawa K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
It is a well-known fact that Alzheimer increases with aging. Early detection of Alzheimer has emerged as an important, because it can prevent of further deterioration of the disease. However, early detection is not always easy because of the lack of good methods to identify the early stage of Alzheimer. The screening tests of Alzheimer used around the world. These tests are relatively time-consuming, difficult and distressing for Alzheimer patients. We consider whether go/no-go task can become the screening test of the Alzheimer patient in future. This study compared results of the Mini Mental State Examination (MMSE) and the go/no-go task for between Alzheimer disease patients and normal subjects. The average reaction time and number of total error of go/no-go task that Alzheimer patients were significantly higher than among the normal subjects. About correlation with MMSE and the go/no-go task, 6 items of MMSE had correlations of 4 or more test results concerning response time, forgets and mistakes of go/no-go tasks. These characteristics suggest that there is a possibility that go/no-go tasks could be applied as a measuring method when screening for early signs of Alzheimer.
Keywords
Alzheimer; Screening; Patients; Possibility
Introduction
People aged 65 years and over accounted for an estimated 7.6% of the world’s population in 2010, and this is projected to rise to 16.2% by 2050 [1]. In Japan, however, this figure was 23.1% in 2010 and is projected to rise to 38.8% by 2050 [2]. The structure of the world population in 2010 indicates that dementia accounted for an estimated 0.5% of the world’s population and it is projected to rise to 1.3% by 2050 [3]. In Japan, this figure was 2.1% in 2010 and is projected to rise to 3.6% by 2050 [4]. It is well known that dementia rates increase with aging [3]. Although dementia mainly affects older people, it is not a normal part of aging. Dementia is deterioration in cognitive function beyond what might be expected from normal aging. It affects memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment. The impairment in cognitive function is normally accompanied, and sometimes preceded, by deterioration in emotional control, social behavior, or motivation [5].
Yamada et al. reported that dementias tend to increase year by year in Japan, Alzheimer's disease (AD) in particular [6]. AD is often misunderstood, causing withdrawal and difficulties in diagnosis and care. The effect of AD on caregivers, family, and societies can be physical, psychological, social, and economic [3]. Early detection of AD has emerged as an important public health priority, because it may potentially prevent further deterioration due to the disease. Early detection will be even more important if new early treatments with long-term effectiveness are confirmed. However, early detection is not always easy because of the lack of good methods to identify the early stages of AD, and research identifying changeable risk factors of AD is scarce [7]. Therefore, many people with AD often stay undiagnosed until symptoms are moderate or severe and, in turn, lose the opportunity to receive early effective treatment. Neuropsychological tests are carried out to screen for AD. Dementing disorders are characterized by specific patterns of brain pathology and dysfunction, but differential diagnosis is often complicated [8]. The screening test for AD used around the world is the Mini-mental state examination (MMSE) [9]. In one recent study, it was reported that the Frontal Assessment Battery (FAB), the Wisconsin Card Sorting Test (WCST), and the Stroop Test are memory tests for AD. However it was reported that these tests are relatively time-consuming, difficult, and distressing for AD patients [10-13]. The present study was conducted with the aim of ascertaining the reliability and validity of the go/no-go tasks.
Method
Subjects
The subjects in the study were 104 Japanese people, comprising 32 patients with AD (5 men, 27 women) aged 84.4 ± 7.2 years (mean ± SD) and 72 normal controls (NC; 23 men, 49 women) aged 65.9 ± 4.9 years. Subjects in the AD group were selected from patients registered at a special elderly nursing home and care health center for the elderly in Obihiro of Hokkaido, Japan. All AD patients had an AD severity of 1 (mild) or 2 (moderate) based on the Clinical Dementia. Rating scale (CDR) [14]. All patients with AD met the criteria for probable AD formulated by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (NINCDS-ADRDA) Alzheimer’s Criteria [15]. All AD patients underwent head magnetic resonance imaging and/or head computed tomography. All ADpatients with evidence of stroke, as determined either by history or imaging findings, were exclude. Subjects in the NC group were recruited from community volunteer groups of participated health education in Matsumoto of Nagano, Japan. They consented to participate as controls in the study after the procedure had been fully explained. All were classified as CDR 0 (healthy) and none of them fulfilled the diagnostic criteria for possible AD [15] or for AD according to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition [5,12]. All participants and guardians of participants were informed of the potential experimental risks and gave their written informed consent, consistent with the human subject policy of Shinshu University.
MMSE
The Japanese version of the MMSE [9] was used to evaluate the severity of AD. The MMSE includes the following tasks: 1. What is the date: (year)(season)(date)(day)(month) - 5 points, 2. Where are we: (state)(county)(town)(hospital)(floor) - 5 points, 3. Name three objects: Ask the patient all three after you have said them. Give one point for each correct answer. Then repeat them until he/she learns all three. Count trials and record. The first repetition determines the score, but if the patient cannot learn the words after six trials then recall cannot be meaningfully tested. Maximum score - 3 points, 4. Serial 7s, beginning with 100 and counting backward: one point for each correct; stop after five answers. Maximum score - 5 points, 5. Ask for the three objects repeated above: one point for each correct. Maximum score - 3 points, 6. Show and ask patient to name a pencil and wrist watch - 2 points, 7. Repeat the following, "No ifs, ands, or buts.& quot; Allow only one trial - 1 point, 8. Follow a three stage command, "Take a paper in your right hand, fold it in half, and put it on the floor." Score one point for each task executed. Maximum score -3 points, 9. On a blank piece of paper write "close your eyes;" ask the patient to read and do what it says - 1 point, 10. Give the patient a blank piece of paper and ask him/her to write a sentence – 1, 11. Copy the design shown – 1.
Go/no-go tasks
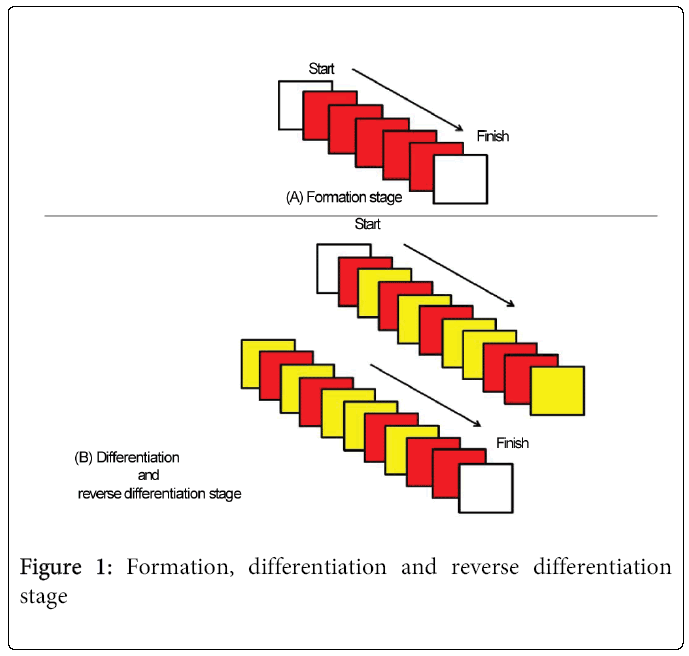
The go/no-go tasks [16] were used to assess inhibition. In the first stage of the go/no-go task, the formation experiment (Figure 1A), subjects were asked to hold a rubber bulb when a red light was lit. In the second stage, the differentiation experiment (Figure 1B), subjects were asked to hold the rubber bulb when the red light was lit but not when a yellow light was lit. The red and yellow lights were presented in random order. During the differentiation reversal session, the roles of the red and yellow lights from the differentiation experiment were reversed, so that subjects were asked to hold the rubber bulb when the yellow light was lit but not when the red light was lit. The subjects performed the formation session five times and the differentiation session and reverse differentiation session ten times each. The experiment was conducted by computer-controlled equipment (MECorporation, Nagano, Japan).
Statistical analysis
Non paired t -tests were used to determine whether the normal subjects were significantly different from the patients of Alzheimer in MMSE and go/no-go tasks. The correlation coefficient termed as R was calculated between go/no-go task score between MMSE in patients of Alzheimer. The level of significance was set at p<0.05. Statistical analyses were performed using SPSS 11.0.1 Statistical Packages (SPSS Inc., Chicago, USA). The significance level was set at p<0.05.
Results
MMSE
Table 1 shows the MMSE scores in both the AD and NC groups. The mean MMSE score for NC was 27.9 ± 2.0, and that for AD was 17.8 ± 5.4. Scores for the NC subjects were significantly higher than those of the AD patients. Eight of the 11 MMSE items showed significant differences between the groups.
| No. of MMSE | Normal subjects | Normal subjects |
|---|---|---|
| No. 1 | 4.9 ± 0.3 | 2.1 ± 1.6 |
| No. 2 | 5.0 ± 0.2 | 3.0 ± 1.7 |
| No. 3 | 3.0 ± 0.0 | 3.0 ± 0.2 |
| No. 4 | 3.6 ± 1.7 | 1.2 ± 1.4 |
| No. 5 | 2.8 ± 0.7 | 1.2 ± 1.3 |
| No. 6 | 2.0 ± 0.0 | 2.0 ± 0.0 |
| No. 7 | 1.0 ± 0.1 | 0.7 ± 0.5 |
| No. 8 | 3.0 ± 0.0 | 2.9 ± 0.3 |
| No. 9 | 1.0 ± 0.0 | 0.8 ± 0.4 |
| No. 10 | 1.0 ± 0.0 | 0.6 ± 0.5 |
| No. 11 | 1.0 ± 0.0 | 0.4 ± 0.5 |
| Total | 27.0 ± 2.0 | 17.8 ± 5.4 |
Mean ± SD NS: No significant different *: p<0.05, ***: p< 0.01
Table 1: Comparison of MMSE score between normal subjects and patients of dementia
Go/no-go tasks
Table 2 shows the go/no-go task results for both groups. The mean reaction times in the formation experiment were significantly faster among NC (225.5 ± 35.2 ms) than in the AD patients (460.7 ± 133.5 ms) (t = -12.7; p<0.001). Reaction times were also significantly faster in NC during the differentiation session (NC: 319.4 ± 49.0 ms; AD: 488.2 ± 90.9 ms; t= -11.8; p<0.001). Similarly, in the differentiation reversal session, the mean reaction time for NC was 347.8 ± 49.0 ms while that for AD was 528.0 ± 104.3 ms (t = -11.1; p<0.001). The overall average reaction time for all three experiments was 312.3 ± 40.4 ms for NC and 507.0 ± 93.7 ms for AD. Overall, NC subjects were significantly faster than AD patients (t= -13.8; p<0.001). In the differentiation session, NC subjects almost never forgot to squeeze the bulb (0.0 ± 0.1 times); in contrast, AD subjects forgot significantly more often (AD: 2.9 ± 3.6 times; t = -6.3; p<0.001). Both groups mistakenly squeezed the bulb; the mean frequency in NC was 2.5 ± 1.9 times, and in AD it was 3.6 ± 2.8 times. In the differentiation reversal session, however, AD subjects forgot to squeeze the bulb significantly more often (NC: 0.0 ± 0.1 times; AD: 3.7 ± 3.9; t = -7.4; p<0.001). Again, both groups mistakenly squeezed the bulb; the mean for NC was 1.6 ± 1.6 and for AD it was 2.0 ± 2.9. There was no difference between groups for mistakenly squeezing.
| Paragraph | normal subjects | patients of dementia | p value |
|---|---|---|---|
| Formation response time | 225.5 ± 35.2 | 460.7 ± 133.5 | *** |
| Differentation response time | 319.4 ± 49.0 | 488.2 ± 90.9 | *** |
| Reverse differentation response time | 347.8 ± 48.9 | 528.0 ± 104.3 | *** |
| Response time average | 312.3 ± 40.4 | 507.0 ± 93.7 | *** |
| Differentation forget | 0.0 ± 0.1 | 2.9 ± 3.6 | *** |
| Differentation mistake | 2.5 ± 1.9 | 3.6 ± 2.8 | NS |
| Reverse differentation forget | 0.0 ± 0.1 | 3.7 ± 3.9 | *** |
| Reverse differentation mistake | 1.6 ± 1.6 | 2.0 ± 2.9 | NS |
| Total forget | 0.0 ± 0.2 | 6.7 ± 7.3 | *** |
| Total mistake | 0.0 ± 0.2 | 5.6 ± 5.2 | NS |
| Total error | 4.2 ± 3.1 | 12.3 ± 7.3 | *** |
Mean ± SD NS: No significant different ***: p< 0.01
Table 2: Comparison of go/no-go task score between normal subjects and patients of dementia
Correlations between MMSE items and the go/no-go task measures. We inspected the correlation with the items of the go/no-go task and the items of MMSE whether we could use go/no-go task as an assessment of Alzheimer. For correlation with MMSE and the go/no-go task of normal subjects, No.2 of MMSE was the only correlation with the reverse differentiation mistake (R = -0.33, p<0.05), there was no other significant difference recognized. Table 3 shows the correlations between items of the MMSE and measures from the go/no-go tasks for Alzheimer patients. Item 6 was removed since all answers were correct and. the results were the same. Items 2, 5, 7, 9, 10, and 11 of the MMSE had correlations 4 of more test results concerning response time, forgetting, and mistakes on the go/no-go tasks. The correlation of item 2 of the MMSE and go/no-go tasks was the following: the formation response time ( R = -0.40, p<0.05), the differentiation forget ( R= -0.42, p<0.05), the reverse differentiation forget ( R = -0.41, p<0.05), and the total forget ( R = -0.42, p<0.05) of go/no-go tasks. The correlation of item 5 of the MMSE and go/no-go tasks was the following: the reverse differentiation response time ( R = 0.45, p<0.05), the differentiation mistake ( R = -0.40, p<0.05), the reverse differentiation of mistake ( R = -0.39, p<0.05), the total mistake ( R = -0.45, p<0.05), and the total error ( R = -0.42, p<0.05) of go/no-go tasks. The correlation of item 7 of the MMSE and go/no-go tasks was the following: the formation response time ( R = -0.42, p<0.05), the differentiation response time ( R = -0.49, p<0.05), the response time average ( R = -0.47, p<0.01), the differentiation forget ( R = -0.67, p<0.001), the reverse differentiation forget( R = -0.68, p<0.001), the total forget ( R = -0.68, p<0.001) and the total error ( R = -0.60, p<0.001) of go/no-go tasks, and the correlation of item 9 of the MMSE and go/no-go tasks was the following: the formation response time ( R = -0.49, p<0.01), the differentiation forget ( R = -0.50, p<0.01), the reverse differentiation forget ( R = -0.49, p<0.01), the total forget ( R = -0.49, p<0.01) and the total error ( R = -0.53, p<0.01) of go/no-go tasks. The correlation of item 10 of the MMSE and go/no-go tasks was the following: the differentiation forget ( R = -0.48, p<0.01), the reverse differentiation forget ( R = -0.53, p<0.001), the total forget ( R = -0.53, p<0.01) and the total error ( R = -0.41, p<0.05) of go/no-go tasks, and the correlation of item 11 of the MMSE and go/no-go tasks was the following: the differentiation response time ( R = -0.39, p<0.05), the reverse differentiation response time ( R = -0.44, p<0.01), the response time average ( R = -0.45, p<0.01), the differentiation forget ( R = -0.47, p<0.01) and the reverse differentiation forget ( R = -0.47, p<0.01) and the total forget ( R=0.44, p<0.01) of go/no-go tasks.
| Go/no-go task | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Formation response time | 0.07 | -0.40† | -0.25 | -0.18 | 0.04 | ― | -0.42† | 0.19 | -0.49†† | -0.17 | -0.20 |
| Differentiation response time | 0.08 | -0.23 | -0.03 | -0.19 | -0.14 | ― | -0.49† | 0.00 | -0.03 | -0.34 | -0.39† |
| Reverse differentiation response time | 0.25 | 0.04 | -0.14 | 0.01 | 0.45† | ― | -0.19 | -0.11 | 0.07 | 0.01 | -0.44†† |
| Mean response time | 0.15 | -0.22 | -0.11 | -0.15 | 0.07 | ― | -0.47†† | 0.12 | -0.15 | -0.27 | -0.45†† |
| Differentiation forgetting | -0.17 | -0.42† | -0.21 | -0.24 | -0.06 | ― | -0.67†† | -0.08 | -0.50†† | -0.48†† | -0.47†† |
| Differentiation mistakes | -0.36† | 0.12 | 0.16 | -0.23 | -0.40† | ― | 0.16 | 0.05 | 0.02 | 0.12 | 0.28 |
| Reverse differentiation forgetting | -0.20 | -0.41† | -0.26 | -0.28 | -0.10 | ― | -0.68†† | -0.08 | -0.49†† | -0.53†† | -0.47†† |
| Reverse differentiation mistakes | -0.16 | 0.17 | 0.06 | -0.23 | -0.39† | ― | 0.04 | -0.30 | -0.10 | 0.13 | 0.27 |
| Total forgetting | -0.21 | -0.42† | -0.26 | -0.27 | -0.12 | ― | -0.68†† | -0.09 | -0.49†† | -0.53†† | -0.44†† |
| Total mistakes | -0.29 | 0.16 | 0.13 | -0.19 | -0.45† | ― | 0.11 | -0.15 | -0.05 | 0.16 | 0.27 |
| Total errors | -0.42† | -0.29 | 0.17 | -0.41† | -0.42† | ― | -0.60†† | -0.19 | -0.53†† | -0.41† | -0.28 |
Table 3: Correlation between go/no-go task score and MMSE item score in AD patients
Discussion
The maximum MMSE total score is 30. Under the standard indications for the MMSE, a score of 27-30 points is normal, 22-26 points is suspected as mild AD, and 0-21 points are diagnosed with AD. In our study, the mean MMSE score for NC subjects was 27.9 ± 2.0 and for AD patients was 17.8 ± 5.4. As anticipated, we found that MMSE measurements for AD were significantly lower than NC. Yoshida et al. [17] reported mean MMSE scores of 20.7 ± 3.5 in AD patients (age: 75.3 ± 5.6), similar to our study. Their grouping (NC or AD) would align with our patient grouping according to MMSE criteria.
We compared results of the go/no-go tasks between the AD and NC groups. Reaction times for the forming experiment, differentiation experiment, and differentiation reversal experiment were significantly faster among the NC subjects. Collette et al. [12] reported that response time of go/no-go tasks in AD patients (age: 69.0 ± 7.4) was 506.3 ± 118.5 ms, very similar to our current findings, and in that study, the overall average reaction time for all three experiments was also significantly slower in AD patients. In the differentiation and differentiation reversal experiments, no significant differences in the number of mistaken squeezes were observed between the two groups. In both the differentiation and reverse differentiation experiments, however, AD patients forgot to squeeze more often than NC subjects, implying attention and concentration to continue go/no-go task declines in patients with AD. It can be considered that the results of the go/no-go tasks have two features. The first is that AD patients had slower reaction times. The second is that AD patients more often forgot to squeeze. Tamm et al. [18] reported that go/no-go tasks require multiple executive functions including working memory,interference avoidance, and response withholding, which have been established as prepotent responses. Core executive functions are inhibition and interference control, working memory, and cognitive flexibility [19]. Response inhibition is an essential executive function implemented by the prefrontal cortex. Performance of go/no-go tasks, which are frequently used to investigate response inhibition, requires a variety of cognitive components besides response inhibition [20]. This implies that AD is not characterized by response inhibition, but rather by a problem occurring with essential executive function. For this reason, to improve cognitive function in AD, training that targets activation of brain functions related to concentration may be effective.
For subjects, normal controls had a mean age of 65.9, and the mean age of AD patients was 84.4, the age differences between the two participant groups were huge, almost 20 years. We had performed go/no-go task to approximately 10 normal elderly people from 80 to 90 years old, some delays were seen at reaction time. But significant differences were not recorded in the reaction time and the number of error between the 52 normal subjects (aged 65.9 ± 4.9 year) and the 10 more elderly people. However, in the future we will gather normal elderly people from 80 to 90 years old and carry out a similar experiment. According to the results of the go/no-go task, Alzheimer patients are not characterized by response inhibition, but rather by a problem occurring with essential executive function. However, we must discuss of future assessments of Alzheimer will be performed in the future. Therefore, we conclude become of the correlation of MMSE and the go/no-go task, that the go/no-go task can generally be used as an assessment of Alzheimer.
There were correlations between many of the MMSE items and response times, forgetting, and errors on the go/no-go task. Together with the group differences in go/no-go tasks, these characteristics suggest a possibility that go/no-go tasks could be applied as a measuring method when screening for early signs of AD.
Conclusion
Early detection of Alzheimer has emerged as an important, because it can prevent of further deterioration of the disease. However, early detection is not always easy because of the lack of .good methods to identify the early stage of Alzheimer. The screening tests of Alzheimer used around the world. These tests are relatively time-consuming, difficult and distressing for Alzheimer patients. We consider whether go/no-go task can become the screening test of the Alzheimer patient in future. The purpose of this study was to carry out go/no-go tasks and MMSE on Alzheimer patients and normal subjects, and bring out the relevance between Alzheimer disease patients and normal subjects. As the results, the average reaction time and number of total error of go/no-go task that Alzheimer patients were significantly higher than among the normal subjects. There were correlations between many of the MMSE items and response times, forgetting, and errors on the go/no-go task. Together with the group differences in go/no-go tasks, these characteristics suggest a possibility that go/no-go tasks could be applied as a measuring method when screening for early signs of AD.
Acknowledgements
Koji Terasawa are supported by a Grant-in-Aid for the Scientist (Houga: 26560380, Kiban A: 25257101) of the Ministry of Education, Culture, Sports, Science and Technology of Japan.This study was supported grant of the Preventive Medical Center of Shinshu University Hospital from Ministry of Education, Culture, Science and Technology.
References
- Department of economic and social affairs office of the high commissioner for human rights (2010) Current status of the social situation, wellbeing, participation in development and right of older persons worldwide. United Nation.
- Japan institute for labour policy and training (2012) Data book of international labor statistics.
- World Health Organization and Alzheimer's Disease International: Alzheimer. A Public Health Priority.
- National Institute of Population and Social Security Research (2011) Ministry of Health, Labour and Welfare.
- American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, (4th end.,) Washington, DC: American Psychiatric Association.
- Yamada M, Mimori Y, Kasagi F, Miyachi T, Ohshita T, et al. (2008) Incidence of dementia, Alzheimer disease, and vascular dementia in a Japanese population: Radiation Effects Research Foundation adult health study. Neuroepidemiology 30: 152-160.
- Grober E, Hall C, McGinn M, Nicholls T, Stanford S, et al. (2008) Neuropsychological strategies for detecting early dementia. J IntNeuropsycholSoc 14: 130-142.
- Bier JC, Ventura M, Donckels V, Van Eyll E, Claes T, et al. (2004) Is the Addenbrooke's cognitive examination effective to detect frontotemporal dementia? J Neurol 251: 428-431.
- Folstein MF, Folstein SE, McHugh PR (1975) "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189-198.
- Holsinger T, Deveau J, Boustani M, Williams JW Jr (2007) Does this patient have dementia? JAMA 297: 2391-2404.
- Kugo A, Terada S, Ata T, Ido Y, Kado Y, et al. (2007) Japanese version of the Frontal Assessment Battery for dementia. Psychiatry Res 153: 69-75.
- Collette F, Van der Linden M, Delrue G, Salmon E (2002) Frontal hypometabolism does not explain inhibitory dysfunction in Alzheimer disease. Alzheimer Dis AssocDisord 16: 228-238.
- Amieva H, Phillips LH, Della Sala S, Henry JD (2004) Inhibitory functioning in Alzheimer's disease. Brain 127: 949-964.
- Hughes C P, Berg L, Danziger WL, Coben LA, Martin R L (1982) A new clinical scale for the staging of dementia. British Journal Psychaiatry 140: 566-572.
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, et al. (1984) Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease. Neurology 34: 939-944.
- Masaki T, Moriyama G (1971) A study on the types of the human higher nervous activity. J Tokyo Science Univ 4: 69-81
- Yoshida H, Terada S, Sato S, Kishimoto Y, Ata T, et al. (2009) Frontal assessment battery and brain perfusion imaging in early dementia. Dement GeriatrCognDisord 27: 133-138.
- Tamm L, Menon V, Reiss AL (2002) Maturation of brain function associated with response inhibition. J Am Acad Child Adolesc Psychiatry 41: 1231-1238.
- Diamond A (2013) Executive functions. Annu Rev Psychol 64: 135-168.
- Chikazoe J (2010) Localizing performance of go/no-go tasks to prefrontal cortical subregions. CurrOpin Psychiatry 23: 267-272.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 16013
- [From(publication date):
October-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11308
- PDF downloads : 4705