Relationship between Maternal Vitamin D Levels and Risk of Low Birth Weight in Term Newborns: A Case Control Study
Received: 06-Jan-2019 / Accepted Date: 18-Feb-2019 / Published Date: 26-Feb-2019 DOI: 10.4172/2572-4983.1000179
Abstract
Introduction: Vitamin D is classically involved in the regulation of calcium and phosphate homeostasis. It is increasingly being recognized to have a multitude of effects on various cell systems and signaling pathways. Vitamin D level of the mother during pregnancy is also assuming great importance as it is expected to have the potential to influence the birth weight.
Objectives: To identify associations between maternal vitamin D deficiency and risk of low birth weight among term newborns and evaluate the socio-demographic factors associated with it.
Material and Methods: A case control study was carried out in the Neonatal Division, JNMCH, during September 2016 to August 2018. Mothers (n=208) were divided into two groups with newborns birth weight <2.5 kg (cases) and 2.5 kg or more (controls). Maternal socio-demographic history and anthropometric examinations of the newborns were noted in a proforma. Maternal vitamin D levels were estimated. Maternal vitamin D statuses of both groups were compared. Analysis was done by SPSS 25.
Results: Mean vitamin D level in mothers of LBW (Low Birth Weight) new-borns (Cases) 12.375 ± 4.20 ng/mL while in mothers of normal birth weight new-borns (Controls) was 16.987 ± 6.38 ng/mL and there is statistically significant correlation between maternal vitamin D and birth weight of term newborns (p<0.01). Also there is positive correlation between maternal vitamin D status and residence, calcium supplementation, seasonal variation, daily sun exposure and shows no correlation with maternal age, educational qualification, parity of mother, BMI and occupation of mothers.
Conclusions: We found high prevalence of hypovitaminosis D in mothers. Low vitamin D levels were significantly associated with LBW and it was found to be associated with certain modifiable and non-modifiable risk factors. There is a need for recommendation for vitamin D supplementation during pregnancy.
Keywords: Pregnancy; Newborns; Birth weight; Vitamin D status; Socio-demographic status
Introduction
Hypovitaminosis D, especially among pregnant women, is a major public health problem with a very high prevalence ranging from 18% to 84%. The levels depend on the residence and local clothing style [1,2]. Pregnancy in vitamin D deficient mothers poses an extra load reducing maternal 25(OH)D levels even further [3,4]. Maternal vitamin D levels have been shown to positively correlate with birth weight centile as has been shown in studies from various countries [5-7].
In a population that already has a high burden of low levels of vitamin D and poor calcium intake in the diet, the scenerio is likely to worsen during pregnancy as the active transplacental transport of calcium to the developing fetus. Low level of vitamin D during pregnancy has important consequences for the newborn including low birth weight [8,9]. SGA (Small for Gestational Age) births are reported more frequent in pregnancies occurring in the winter with vitamin D deficiency [10].
Vitamin D deficiency is unexpected in India, a tropical country where there is adequate overhead sun for most of the time all of the year. Nevertheless, low level of vitamin D, resulting in severe manifestations, has been observed in India [11]. This paradox may be partly explained by the local social and cultural practices in India that preclude adequate exposure of adolescent girls and young women to sunshine. Recent urbanization that results in poor outdoor activity and greater pollution burden, coupled with other factors, may further aggravate this problem [12,13].
In this study, which was the first investigation in this part of the country, we were intended to compare the maternal low vitamin D levels between LBW and normal birth weight newborns.
Objectives
Primary
To identify associations between maternal low vitamin D levels and risk of LBW among term newborns.
Secondary
To evaluate the socio-demographic factors associated with low vitamin D levels in mothers.
Materials and Methods
This study (a case control study) was conducted in the Neonatal Division department of pediatrics in collaboration with department of Obstetrics & Gynecology and Rajiv Gandhi Centre for Diabetes and Endocrinology, JNMCH, AMU, Aligarh from September 2016 to August 2018. Two hundred eight babies born with gestational age 37-41 weeks with birth weight <2500 g (Cases=104) or >2500 g (Controls=104) were included in the study. Babies with congenital malformations, GA <37 weeks or >42 weeks, mothers with any systemic diseases or on any medications that influence vitamin D metabolisms and refusal to give consent were excluded. The ethical clearance was obtained from Institutional Ethics Committee, JNMCH, Faculty of Medicine, AMU, Aligarh.
Brief Procedure
After taking written informed consent from the parent of the eligible subjects, a detailed history and physical examination was done and the findings were recorded on a pre-designed proforma. Approximately 5 mL of maternal blood was withdrawn for estimation of serum vitamin D level. Total circulating 25(OH)-D was assayed on Access 2 immunoassay system (Beckman Coulter) using chemiluminescence in the laboratory. The levels were classified as deficiency :<12 ng/mL, insufficiency:12-20 ng/mL sufficiency >20 ng/mL (Food and Nutrition Board, Ministry of Women and Child Health and Indian academy of Pediatrics) The analysis was done using the SPSS software Version 25.
Observation and Results
Maternal vitamin D status was found to have a positive correlation with birth weight (p<0.01), birth length (p<0.01), head circumference (p<0.01) and chest circumference (p<0.01) taking p value significant at a level <0.05 by ANOVA Analysis. This study also shows that there were 54.8% deficient, 38.5% insufficient and only 6.7% sufficient Vitamin D status in mothers of LBW newborns (Cases) while 29.8% deficient, 24% insufficient and 46.2% sufficient Vitamin D status in mothers of normal birth weight newborns (Normal) (Tables 1-4).
| Variables | Cases | Controls | p value |
|---|---|---|---|
| 1. Maternal Age | |||
| ≤ 25 years | 60 (51.7%) | 56 (48.3%) | 0.574 |
| >25 years | 43 (47.8%) | 47 (52.2%) | |
| 2. Gestational Age | |||
| 37th Weeks | 40 (50%) | 40 (50%) | 0.130 |
| 38th Weeks | 35 (61.4%) | 22 (38.6%) | |
| 39th Weeks | 16 (38.1%) | 26 (61.9%) | |
| 40th Weeks | 13 (44.8%) | 16 (55.2%) | |
| 3. Education | |||
| Illiterate | 4 (33.3%) | 8 (66.7%) | 0.114 |
| <Secondary | 29 (42.6%) | 39 (57.4%) | |
| ≥ secondary | 71 (55.5%) | 57 (44.5%) | |
| 4. Residence | |||
| Rural | 34 (42.5%) | 46 (57.5%) | 0.087 |
| Urban | 70 (54.7%) | 58 (45.3%) | |
| 5. Occupation | |||
| Housewife | 83 (48%) | 90 (52%) | 0.194 |
| Working | 21 (60%) | 14 (40%) | |
| 6. Parity | |||
| Primiparous | 37 (46.8%) | 42 (53.2%) | 0.475 |
| Multiparous | 67 (51.9%) | 62 (48.1%) | |
| 7. Daily Sun Exposure (30 min) | |||
| Yes | 38 (48.1%) | 41 (51.9%) | 0.668 |
| No | 66 (51.2%) | 63 (48.8%) | |
| 8. Calcium Supplements (4 months) | |||
| Yes | 53 (44.5%) | 66 (55.5%) | 0.068 |
| No | 51 (57.3%) | 38 (42.7%) | |
| 9. Body Mass index (BMI) | |||
| <30 | 73 (46.5%) | 4 (53.5%) | 0.076 |
| ≥ 30 | 31 (60.8%) | 20 (39.2%) | |
| 10. Mode of delivery | |||
| NVD | 71 (47.7%) | 78 (52.3%) | 0.282 |
| LSCS | 33 (55.9%) | 26 (44.1%) | |
| 11. Delivery Season | |||
| Winter (Dec to Feb) | 45 (58.4%) | 32 (41.6%) | 0.064 |
| Spring (Mar to May) | 19 (35.8%) | 34 (64.2%) | |
| Summer (Jun to Aug) | 13 (44.8%) | 16 (55.2%) | |
| Autumn (Sep to Nov) | 27 (55.1%) | 22 (44.9%) | |
Table 1: Maternal demographic characteristics of cases and controls.
| Variables | Total (n=208) | Vitamin D deficient | Vitamin D insufficient | Vitamin D sufficient | p value |
|---|---|---|---|---|---|
| 1. Birth weight | |||||
| <2.5 kg | 104 (50%) | 57 (54.8%) | 40 (38.5%) | 7 (6.7%) | p<0.01 (Significant) |
| ≥ 2.5 kg | 104 (50%) | 31 (29.8%) | 25 (24%) | 48 (46.2%) | |
| 2. Birth Length | |||||
| ≤ 47 cm | 106 (51%) | 58 (54.7%) | 38 (35.8%) | 10 (9.4%) | p<0.01 (Significant) |
| >47 cm | 102 (49%) | 30 (29.4%) | 27 (26.5%) | 45 (44.1%) | |
| 3. Head Circumference | |||||
| ≤ 33 cm | 161 (77.4%) | 75 (46.6%) | 55 (34.2%) | 31 (19.3%) | p<0.01 (Significant) |
| >33 cm | 47 (22.6%) | 13 (27.7%) | 10 (21.3%) | 24 (51.1%) | |
| 4. Chest Circumference | |||||
| <= 30 cm | 92 (44.4%) | 47 (51.1%) | 32 (34.8%) | 13 (14.1%) | p<0.01 (Significant) |
| >30 cm | 115 (55.6%) | 40 (34.8%) | 33 (28.7%) | 42 (36.5%) | |
Table 2: Newborns characteristics in comparison to maternal vitamin D status.
| Groups | Mean Vitamin-D level | Deficiency n (%) | Insufficiency n (%) | Sufficiency n (%) |
|---|---|---|---|---|
| Mothers of LBW neonates (Cases) |
12.375 (SD=4.20) | 57 (54.8%) | 40 (38.5%) | 7 (6.7%) |
| Mothers of normal birth weight neonates (Controls) | 16.987 (SD=6.38) |
31 (29.8%) | 25 (24%) | 48 (46.2%) |
Table 3: Maternal vitamin D levels in cases and controls.
| Variables | Vitamin D deficiency (N=88) |
Vitamin D insufficiency (N=65) |
Vitamin D sufficiency (N=55) |
p value |
|---|---|---|---|---|
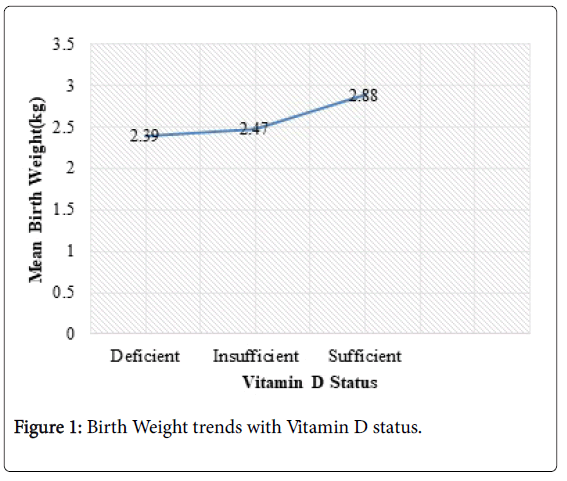
| Birth weight | 2.39 ± 0.232.47 | 2.47 ± 0.39 | 2.88 ± 0.43 | <0.01 |
| Birth length | 47.34 ± 2.0 | 47.44 ± 2.33 | 49.15 ± 1.89 | <0.01 |
| Head Circumference | 31.69 ± 1.60 | 31.74 ± 1.63 | 32.73 ± 1.88 | <0.01 |
| Chest Circumference | 29.96 ± 1.57 | 30.07 ± 1.67 | 31.12 ± 1.99 | <0.01 |
Statistically significant p value at <0.05 level by ANOVA Analysis
Table 4: Newborn characteristics association with maternal vitamin D level.
We have also found that out of 104 low birth weight (<2.5 kg) babies, their maternal vitamin D status were following: 54.8% have deficient, 38.5% have insufficient and only 6.7% have sufficient vitamin D status while in normal birth weight (≥2.5 kg) babies, their maternal vitamin D status were following: 29.8% have deficient, 24% have insufficient and 46.2% have sufficient vitamin D level. Figure 1 showing birth weight trends with vitamin D status.
Discussion
Aligarh lies at latitude of 27.88°N and longitude of 78.08°E and 178 m above sea level. There is ample of sunshine throughout the summer days. Yet, the apparently healthy populations including pregnant mothers in this area were found to be deficient in Vitamin D as suggested by unpublished studies conducted in our institution.
Maternal vitamin D status and birth size
Our study showed that mean vitamin D level in mothers of LBW (cases) 12.375 ± 4.20 ng/mL was lower than in mothers of normal birth weight (controls) newborns 16.987 ± 6.38 ng/mL and this findings was consistent with the study by Khalessi et al. [14] and other studies [5,7]. Maternal vitamin D levels were found to be positively correlated with birth weight (p<0.01). This finding was also seen in the study by Bodner et al. [15] Australian researchers found that mean birth weight was 200 g lower (p <0.01) in babies of vitamin D deficient mothers [6]. Many other studies have also reported an association between infant size and vitamin D status. We have also found a positive correlation of maternal vitamin D status with birth length (p<0.01), head circumference (p<0.01) and chest circumference (<0.01) and this was compatible with studies by Song et al. [16] and Satish et al. [17] was against findings by Khalessi et al. [14].
Maternal vitamin D status in comparison to sociodemographic characteristics
We found a positive correlation between maternal vitamin D status and place of residence (p<0.01), duration of sun exposure (p<0.01), season of the year (p<0.01) and intake of calcium supplements (p<0.01) which was also supported by studies by Prasad et al. [18] and by Dave et al. [19]. Our study found no significant association between maternal vitamin D levels (status) and maternal age, maternal education, occupation or parity. Similar findings were noted by Khalessi et al. [14] but not in the study by Prasad et al. [18].
Like other case control studies, this study too was not free from limitations. Maternal nutritional status and socio-economic status was not evaluated in the questionnaire. In addition, estimation cord blood calcium, PTH and ALP was not done. The status of vitamin D in the newborns could also not be done due to financial constraints. We propose that the given factors may be considered in the future studies. Despite these limitations, the strength of our study lies in the fact that we had taken good number sample size and was adequately powered to detect a clinically meaningful difference in Vitamin D levels between cases and controls.
Conclusions
We found high prevalence of low vitamin D in mothers. Low vitamin D levels were significantly associated with LBW and low size of the newborns. Vitamin D status was found to be associated with certain modifiable and non-modifiable risk factors. There is a need for recommendation for vitamin D supplementation during pregnancy.
Conflict of Interest
There is no conflict of interest by the authors.
References
- Vandevijvere S, Amsalkhir S, Van Oyen H, Moreno-Reyes R (2012) High prevalence of vitamin D deficiency in pregnant women: a national cross-sectional survey. PLoS One 7: e43868.
- Dawodu A, Wagner CL (2007) Mother-child vitamin D deficiency: an international perspective. Arch Dis Child 92: 737-740.
- Ardawi MS, Nasrat HA, Ba’Aqueel HS (1997) Calcium-regulating hormones and parathyroid hormone-related peptide in normal human pregnancy and postpartum: a longitudinal study. Eur J Endocrinol 137: 402-409.
- Fernández-Alonso AM, Dionis-Sánchez EC, Chedraui P, González-Salmerón MD, Pérez-López FR, et al. (2012) First-trimester maternal serum 25-hydroxyvitamin D₃ status and pregnancy outcome. Int J Gynaecol Obstet 116: 6-9.
- Robinson CJ, Wagner CL, Hollis BW, Baatz JE, Johnson DD (2011) Maternal vitamin D and fetal growth in early-onset severe preeclampsia. Am J Obstet Gynecol 204: 556.e1-556.e4.
- Leffelaar ER, Vrijkotte TG, van Eijsden M (2010) Maternal early pregnancy vitamin D status in relation to fetal and neonatal growth: results of the multi-ethnic Amsterdam Born Children and their Development cohort. Br J Nutr 104: 108-117.
- Bowyer L, Catling-Paull C, Diamond T, Homer C, Davis G, et al. (2009) Vitamin D, PTH and calcium levels in pregnant women and their neonates. Clin Endocrinol 70: 372-377.
- Delvin EE, Salle BL, Glorieux FH, Adeleine P, David LS (1986) Vitamin D supplementation during pregnancy: effect on neonatal calcium homeostasis. J Pediatr 109: 328-334.
- Purvis RJ, Barrie WJ, MacKay GS, Wilkinson EM, Cockburn F, et al. (1973) Enamel hypoplasia of the teeth associated with neonatal tetany: a manifestation of maternal vitamin D deficiency. Lancet 2: 811-814.
- Ford JH (2011) Preconception factors and SGA babies; papilloma virus, omega 3 and fat soluble vitamin deficiencies. Early Hum Dev 87: 785-789.
- Rajeswari J, Balasubramanian K, Bhatia V, Sharma VP, Agarwal AK (2003) Aetiology and clinical profile of osteomalacia in adolescent girls in northern India. Natl Med J India 16: 139-142.
- Agarwal KS, Mughal MZ, Upadhyay P, Berry JL, Mawer EB, et al. (2002) The impact of atmospheric pollution on vitamin D status of infants and toddlers in Delhi, India. Arch Dis Child 87: 111-113.
- Dror D, King JC, Durand DJ, Allen LH (2011) Association of Modifiable and Nonmodifiable Factors with Vitamin D Status in Pregnant Women and Neonates in Oakland, CA. J Am Diet Assoc 111: 111-116.
- Khalessi N, Kalani M, Araghi M, Farahani Z (2015) The Relationship between Maternal Vitamin D Deficiency and Low Birth Weight Neonates. J Family Reprod Health 9: 113-117.
- Bodnar LM, Catov JM, Zmuda JM, Cooper ME, Parrott MS, et al. (2010) Maternal serum 25-hydroxyvitamin D concentrations are associated with small-for-gestational age births in white women. J Nutr 140: 999-1006.
- Song SJ, Si S, Liu J, Chen X, Zhou L, et al. (2012) Vitamin D status in Chinese pregnant women and their newborns in Beijing and their relationships to birth size. Pub Health Nutr 16: 1-6.
- Sathish P, Raveendran S, Padma R, Balakrishnan D, Muthusami M (2016) Correlation between maternal and neonatal blood vitamin D levels and its effect on the newborn anthropometry. Int J Reprod Contracept Obstet Gynecol 5: 2983-2988.
- Prasad D, Smita, Singh K, Nisha S (2018) Vitamin D in Pregnancy and its Correlation with Feto Maternal Outcome. Int J Contemp Med Res 5: 31.
- Dave A, Verma M, Jain N, Dave A (2017) A study of vitamin D levels and associated deficiency in pregnancy and its effect on maternal and fetal outcome. Int J Reprod Contracept Obstet Gynecol 6: 84-88.
Citation: Zamal A, Ali SM, Firdaus U, Noor N, Siddiqi SS (2019) Relationship between Maternal Vitamin D Levels and Risk of Low Birth Weight in Term Newborns: A Case Control Study . Neonat Pediatr Med 5: 179. DOI: 10.4172/2572-4983.1000179
Copyright: © 2019 Zamal A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3256
- [From(publication date): 0-2019 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 2431
- PDF downloads: 825