Rehabilitation Processes involved in Rehabilitating Individuals with Alcohol and Drug Addictions at Rehabilitation Centres in Ghana
Received: 21-Jul-2018 / Accepted Date: 17-Aug-2018 / Published Date: 24-Aug-2018 DOI: 10.4172/2155-6105.1000364
Keywords: Individuals with alcohol and drug addiction; Addiction; Rehabilitation
Background
Alcohol and drug addiction begins with continuous craving and use irrespective of the intensity of its consequences [1-5]. Globally, 13 Disability-Adjusted Life Years (DALYs) lost per 1000 population are due to alcohol and illicit drug use where alcohol alone contributes to an annual loss of about 58.3 million DALYs resulting in 40 percent of DALYs in mental disorders and diseases of the nervous system [6]. It is estimated that 25 million people are regarded as drug addicts and at least 15.3 million have drug use disorders [7]. About 60% of two billion individuals who consume alcohol every year abuse alcohol and other drugs [7]. The situation is alarming in developing countries such that there were between 16 and 38 million addicts in the developing world as of the year 2008 [7]. The consequences of alcohol and drug addictions is universal but very devastating in sub-Saharan African countries [8,9]. However, these countries have limited rehabilitation programmes which are often ineffective [8,9]. Globally, about 39 deaths per 100000 populations are attributed to alcohol and illicit drug abuse, out of which 35 deaths are attributed to alcohol abuse [10]. In Ghana, for instance, about 40 percent of criminal offences prosecuted in the law courts are drug use, possession or related [8]. It is estimated that 4.1 per 100,000 deaths in Ghana are due to alcohol and drug abuse and addiction [9]. This situation, therefore, needs to be addressed.
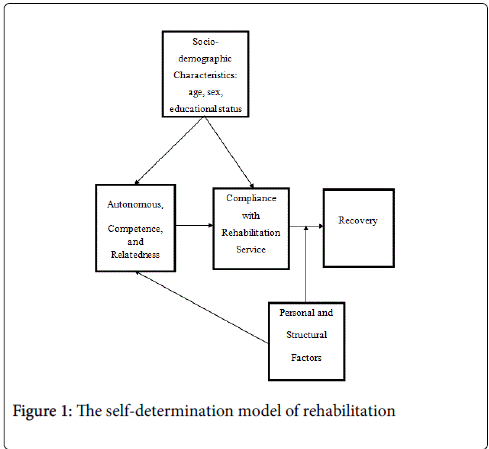
Addressing alcohol and drug addiction through rehabilitation is important in improving the medical and socio-economic conditions (health, social, and emotional wellbeing) of individuals with addictions, their families, and communities [11]. Rehabilitation involves a process by which an individual with alcohol and drugrelated problem achieves an optimal state of health, psychological functioning, and social wellbeing in order to ensure his or her reintegration into families and societies [4,11]. According to National Institute on Drug Abuse [12] and WHO [13], specific steps of one’s addiction rehabilitation process vary according to the state of addiction, the treatment plan used, and the individual. However, all rehabilitation processes share certain similarities which include intake process, detoxification process, rehabilitation process, and recovery process (Figure 1)[12].
Furthermore, Flora and Stalikas [14] establish that positive and negative factors associated with rehabilitation processes have an influence on rehabilitating people with alcohol and drug addiction which also determine clients’ level of compliance with rehabilitation services and providers as well as recovery from addiction. The Selfdetermination Model of Rehabilitation (Figure 1), adapted from Self- Determination Model, used as the conceptual framework for the study explains that variables such as socio-demographic characteristics and personal and structural factors influence experiences of autonomy, competence, and relatedness as well as compliance with rehabilitation services, and recovery [15]. The conceptual framework further implies that personal and structural factors can interfere with autonomy, competence, and relatedness as well as a patient’s recovery [15]. Access to information on rehabilitation of individuals with alcohol and drug addiction is important in the fight against drug addiction. However, information on rehabilitation of individuals with alcohol and drug addictions is limited in Ghana and for that matter, Cape Coast Metropolis. Most studies [8,9,16-19] have focused on alcohol and drugs use as well as addiction without touching on the rehabilitation processes. This study, therefore, sought to explore rehabilitation processes involved in rehabilitating individuals with alcohol and drug addictions in Ghana.
Methods
The study population for this qualitative research consisted of 28 alcohol and drug addiction patients and rehabilitation service providers at two rehabilitation centres in the Cape Coast Metropolis of Central Region, Ghana. In all, fourteen addiction patients and fourteen service providers were interviewed by semi-structured in-depth interviews through tape-recording in English. The study participants were interviewed in the languages they best understood and were comfortable with. As a result, most (25) of them spoke English while the rest spoke Fante, Twi, and Ewe. The addiction patients consisted of twelve persons undergoing rehabilitation and two former rehabilitated and discharged patients. The 12 patients who participated in the study were the only ones on admission at the two rehabilitation centres as of the time of the data collection. The socio-demographic information about the study participants (patients and service providers) are presented in Tables 1 and 2 respectively. As of the time of this study, only two alcohol and drug addiction rehabilitation centres were available in the Cape Coast Metropolis. These centres are Ankaful Rehabilitation Centre (a state-owned facility) and Mercy Rehabilitation Centre, owned by a religious organization. Purposive sampling technique was used to select the service providers and the two former rehabilitated patients while individuals with alcohol and drug addiction undergoing rehabilitation at the rehab centres were selected through accidental sampling technique. At the Ankaful Rehabilitation Centre, 13 service providers consisting of seven males and six females were selected with saturation (similar or no more patterns of data or themes emerged) while ten male patients were also interviewed. Surprisingly, only one male service provider was responsible for providing rehab services to four patients consisting of one female and three males at the Mercy Rehabilitation Centre. The data collection team consisted of six teaching and research assistants from the University of Cape Coast in Cape Coast, Ghana. The members of the data collection team were involved in the data collection based on their previous experiences in qualitative data collection and their ability to speak English and the local languages in the Cape Coast Metropolis. The research team was briefed on the objectives and the demands of the interviews as well as the category of respondents included in the study by the researchers during a pre-data collection training and orientation.
| Respondent’s ID | Age | Sex | Academic Qualification | Area of Specialisation | Marital Status | Religion | Number of years of work at the centre | Rehabilitation Centre |
|---|---|---|---|---|---|---|---|---|
| A | 54 | Male | Masters | Counsellor (Chaplain) | Single | Christian | 13 | Mercy Centre |
| B | 28 | Male | Degree | General Nursing | Single | Christian | 2 | Ankaful Centre |
| C | 30 | Female | Diploma | Mental Health Nursing | Cohabitating | Christian | 3 | Ankaful Centre |
| D | 29 | Male | Degree | General Nursing | Single | Christian | 5 | Ankaful Centre |
| E | 25 | Male | Diploma | Mental Health Nursing | Single | Christian | 2 | Ankaful Centre |
| F | 28 | Male | Diploma | Mental Health Nursing | Single | Christian | 2 | Ankaful Centre |
| G | 24 | Female | Diploma | Mental Health Nursing | Single | Christian | 4 | Ankaful Centre |
| H | 34 | Female | Degree | General Nursing | Married | Christian | 5 | Ankaful Centre |
| I | 29 | Female | Diploma | Mental Health Nursing | Cohabitating | Christian | 4 | Ankaful Centre |
| J | 34 | Male | Diploma | Mental Health Nursing | Married | Christian | 3 | Ankaful Centre |
| K | 26 | Female | Diploma | Mental Health Nursing | Married | Muslim | 4 | Ankaful Centre |
| L | 27 | Female | Diploma | Mental Health Nursing | Married | Christian | 3 | Ankaful Centre |
| M | 26 | Male | Diploma | Mental Health Nursing | Single | Christian | 2 | Ankaful Centre |
| N | 52 | Male | Degree | Clinical Psychologist | Married | Christian | 5 | Ankaful Centre |
Table 1: Socio-demographic characteristics of service providers.
| Respondent’s ID | Age | Sex | Level of Education | Marital Status | Children | Employment Status | Religion | Length of stay at the Centre | Rehabilitation Centre |
|---|---|---|---|---|---|---|---|---|---|
| A | 54 | Female | Tertiary | Single | None | Lost job | Christian | 2 months | Mercy Centre |
| B | 38 | Male | Tertiary | Single | 1 | Lost job | Christian | 2 months | Mercy Centre |
| C | 16 | Male | Primary | Single | None | Student | Christian | 1 month | Mercy Centre |
| D | 30 | Male | Secondary school | Married | 2 | Unemployed | Christian | 4 months | Ankaful Centre |
| E | 25 | Male | Secondary school | Single | None | Unemployed | Christian | 4 months | Ankaful Centre |
| F | 31 | Male | Vocational school | Married | 3 | Lost job | Christian | 5 months | Ankaful Centre |
| G | 39 | Male | Tertiary | Married | 4 | Lost job | Christian | 3 months | Ankaful Centre |
| H | 27 | Male | Vocational school | Single | None | Unemployed | Muslim | 2 months | Ankaful Centre |
| I | 42 | Male | Vocational school | Married | 4 | Lost job | Christian | 4 months | Ankaful Centre |
| J | 24 | Male | Tertiary | Single | None | Unemployed | Christian | 3 months | Ankaful Centre |
| K | 35 | Male | Primary | Married | 6 | Lost job | Christian | 5 months | Ankaful Centre |
| L | 30 | Male | Secondary school | Single | 2 | Lost job | Christian | 4 months | Ankaful Centre |
| M* | 48 | Male | Junior High School | Single | 3 | Lost job | Christian | 2 months | Mercy Centre |
| N* | 26 | Male | Secondary school | Single | None | Unemployed | Christian | 6 months | Ankaful Centre |
Table 2: Socio-demographic characteristics of patients (Addicts), *Former inmates.
Permission to conduct the interviews at the two centres was sought through letters and personal contact with the heads of the centres. Informed consents (oral and written) were obtained from the study participants before the interviews took place. There was no reported refusal of participation among the respondents. The Graduate School and Department of Population and Health of the University of Cape Coast gave ethical approval for the study while anonymity and confidentiality of the study participants were observed in the study.
Findings were reported using pseudonyms. The interview on average lasted about 45 min for the patients and 60 min for the service providers. The data analysis process involved transcription of all the interviews conducted. The interviews conducted in the local languages were translated into English before analysis. The data were analysed and summarised based on the emerged themes and similarity in meanings specified with quotations [20].
Results and Discussion
Themes and quotes were used to present the findings for easy understanding of alcohol and drug addiction rehabilitation processes. The findings were presented based on the varied experiences of service providers and patients at the two rehab centres to understand the dynamics in their services. Detailed information with pseudonyms of the respondents’ sociodemographic data are presented in Tables 1 and 2 respectively.
Rehabilitation processes
Processes involved in the rehabilitation of individuals with alcohol and drug addictions play a significant role in the total recovery of patients [12]. The study, therefore, sought information on the processes involved in the rehabilitation of patients at the centres. As a result, the service providers and the addiction patients were asked to explain the rehabilitation processes used to rehabilitate addiction patients. It emerged that the rehabilitation processes at both the Ankaful and Mercy Rehabilitation Centres were similar. Service providers interviewed at both centres described the processes used to rehabilitate patients as unidirectional but multidimensional. They explained further that patients were taken through a series of linear processes with the help of an interdisciplinary team of health professionals such as physicians, therapists, and nurses which explain the multidimensional component. The service providers also elaborated that the unidirectional processes of patients included recording sociodemographic characteristics and addiction history of patients, making financial arrangements with them for their stay, diagnostic tests and medication, counselling and medication, and recovery plans. Some of the service providers had these to say:
The processes involved in rehabilitating patients at this centre follow a directional process where the patients first meet the clinical psychologist or the administrator before being admitted at the centre. We do not admit patients directly at centre unless he or she has met the clinical psychologist or the administrator for arrangements with the patients on his or her stay at the centre (D: A 29 yr old male General Nursing service provider at Ankaful Rehabilitation Centre).
I am the only service provider at this centre and therefore no patient comes and stays here without first seeing me for arrangements on how he or she will stay at the centre. There are rules and regulations at this centre and therefore all those things must be explained to patients before admission (A: A 54 yr old male Counsellor (Chaplain) at Mercy Rehabilitation Centre).
The patients at both centres as well as the two former inmates also shared similar views on the processes involved in rehabilitating patients. They explained that they had to go through a series of steps with different health professionals before admission at the centre. The patients further indicated that they had to meet or see the counsellor, clinical psychologist or the administrator before being allowed at the rehabilitation centres. They also said that during such meetings with the staff, the nature of the rehabilitation programme including financing arrangements and rules and regulations was explained to them. Some of the patients had these to say:
My relatives first took me to the clinical psychologist who asked me how long I used the drug, the effects, and if I wanted to be helped. He also made some financial arrangements with my relatives for my stay at centre because the rehabilitation programme is not free. After the meeting, he wrote down my age, name, marital status, etc. before asking a nurse to come for me to the centre (G: A 39 yr old patient at Ankaful Rehabilitation Centre).
When I arrived at the centre with my mother, the counsellor was not available that day and so we were asked to come another day or wait for a while. We waited for him and he came in about five hours’ later and attended to us. He asked me why I used the drug and if I was ready to change. He asked my mother to pay some money because the programme requires a fee. After all that was done, he sent me to a doctor in the Cape Coast town where a diagnostic test was conducted on me and later brought to join my colleagues at the centre (C: A 16 yr old single male patient at Mercy Rehabilitation Centre).
The service providers at both centres disclosed that the processes of rehabilitation applied to all the patients irrespective of their sociodemographic characteristics because any discrimination can arouse mixed feelings and jealousy among the patients and therefore could affect the rehabilitation processes and bring about non-compliance and relapse. The service providers further reported that patients with severe addictions and aggression were kept at a separate ward called ‘acute ward’ for about a week where medications were given to calm them and later transferred to the main rehabilitation ward. The participants also elaborated that addiction required a long period of rehabilitation and therefore patient often spent either three, six, or twelve months at the centre depending on the severity of one’s condition. Since services rendered at the rehab centres are not wholly free, ability to pay the fees sometimes determine the length of stay of patients at the centre, because one is discharged only after all bills are fully settled.
Every patient goes through the processes of rehabilitation and no patient is treated differently because that would amount to discrimination and unfairness. The only difference is that some patients stay at the centre for about three, six, or twelve months depending on the severity of their condition and the ability to pay because the more a patient stays, the more money he or she pays (I: A 29 yr old female Mental Health Nursing service provider at Ankaful Rehabilitation Centre).
The findings from the study, therefore, show that the processes involved in the rehabilitation of individuals with alcohol and drug addictions comprised a unidirectional process and interdisciplinary team of health professionals at both Ankaful and Mercy Rehabilitation Centres in the Cape Coast Metropolis. The processes involved in the rehabilitation of patients at the centres included recording sociodemographic characteristics and addiction history of patients, making financial arrangements with them for their stay, diagnostic tests and medication, counselling and medication, and recovery plans. It was, in addition, revealed from the study that even though the processes involved in rehabilitation applied to all the patients equally, the severity of their conditions determined the possibility of been admitted to the acute ward first before been transferred to the main rehabilitation ward. Consistent with this finding, the Stages of Change Theory by Prochaska and Di Clemente [21] as cited in Noar et al. [22] explained that processes are involved in behaviour change with progress through a series of stages and therefore people move through a series of stages when modifying behaviour. Similarly, Martin [23] stated that involving numerous and diverse as well as an interdisciplinary team of health professionals in rehabilitation services promote effective treatment and facilitate recovery because addiction involves multidimensional processes. National Institute on Drug Abuse [12] is also of the view that rehabilitation processes are linear (intake process, detoxification process, rehabilitation process, and recovery process).
Recording of socio-demographic characteristics of patients
As part of the rehabilitation processes, the socio-demographic characteristics of patients were taken by service providers upon arrival of patients at the centres. The service providers at both rehabilitation centres emphasised that, immediately upon the arrival of the patients at the centres, their socio-demographic information and addiction history were taken. These vital information were taken by either an administrative staff, counsellor or a clinical psychologist. It emerged that the socio-demographic characteristics of importance were the patient’s age, sex, marital status and number of children, a level of education, employment status, religion, type of drug(s) used and reasons for use. The respondents reported that these information obtained aid personnel at the centre to properly handle and manage the patients. The service providers further specified that the recording of the socio-demographic characteristics of the patients was performed in order to know the category of individuals with addictions that accessed rehabilitation services at the centres.
I normally record the socio-demographic characteristics of the patients to know the category of patients that come to the centre and to know the type of addiction they experience. I am the clinical psychologist and therefore every patient comes to me first for psychological, physical, and emotional assessment. If I am not available at work, the administrative staff takes charge. I have to explain the patient’s condition to him or her to ensure his or her readiness for the rehabilitation services. The rehabilitation services we operate here are voluntary and not like a prison where inmates have to be forced (N: A 52 yr old male Clinical Psychologist at Ankaful Rehabilitation Centre).
If I do not take the socio-demographic characteristics of my patients, I would not know the age, sex, and etc. category of addicts that come to my centre. Taking their background information helps me to provide effective services because I would be able to provide resources per the kind of clients that come to the centre (A: A 54 yr old male Counsellor at Mercy Rehabilitation Centre).
Similarly, the patients interviewed at both centres as well as the two former inmates explained that their socio-demographic characteristics were taken before they were admitted at the centres. They further indicated that their age, sex, marital and employment statuses, educational level, and type of drug used were taken by the clinical psychologist, administrative staff or a counsellor. This was indicated in the statements by some of the patients;
When I met the counsellor with my friend, he asked and wrote my name, age, sex, educational level, work, marital status, number of children, and my addiction history (B: A 38 yr old single male patient at Mercy Rehabilitation Centre).
The administrator attended to me that day and asked for my age, addiction history, employment status, marital status, and educational level (J: A 24 yr old married male patient at Ankaful Rehabilitation Centre).
It became evident from the study that obtaining the sociodemographic characteristics and addiction history of patients provided information on the patients which helped the service providers at the centres to know the category of addicts that access rehabilitation services at the centres in order to properly handle the patients. This is in line with National Institute on Drug Abuse [12] elaboration that rehabilitation processes also involve recording addiction history of the patient and a rehabilitation plan is tailored to the patient’s individual needs.
Financial arrangements
United Nations Office on Drugs and Crime [24] observed that rehabilitation processes include financial arrangements with the patients or their guardians. It was evident from the study that financial arrangements were made between the rehab centres and patients for rehabilitation services. The service providers including the clinical psychologist and the counsellor indicated in the interview that the rehabilitation services were not free but National Health Insurance Scheme (NHIS) covered all minor sicknesses and ailments including but not limited to cases of malaria, stomach aches, and headaches. The service providers also emphasised that financial arrangements were made with the patients to establish the patients’ or their guardians’ readiness to pay for the number of months that the patient would stay at the centre. It was also established by the service providers that any patient who had not finished paying or could not continue to pay the fees faced evacuation from the centre even before the said patient has fully recovered.
Before we conduct any medical diagnosis and give medicines to any patient, his or her guardian should be prepared to pay for the services and for the number of months that the patient would stay at the centre (H: A 34 yr old female General Nursing service provider at Ankaful Rehabilitation Centre).
The services I offer at this centre are not free and so the patients or their guardians have to make financial commitments first before any further service is offered (A: A 54 yr old male Counsellor at Mercy Rehabilitation Centre).
Patients who are not able to settle their bills are usually evacuated from the centre because the services are not free (L: A 27 yr old female Mental Health Nursing service provider at Ankaful Rehabilitation Centre).
Consistently, the patients at both Ankaful and Mercy Rehabilitation Centres and the two former inmates also disclosed that high level of fees associated with their rehabilitation at the centres frustrate them. Therefore, according to the respondents, they comply and take the rehabilitation services serious in order not to incur any extra cost due to their prolong stay at the centre. They further explained that the fees which their guardians pay covered food, accommodation, counselling, medication, and utilities at the centres.
Even though the fee covers what we use here, it is too expensive that I do not want to stay here more than the number of months my friend has agreed to pay for. I am doing all I can to assist the service providers to help me recover on time (G: A 39 yr old married male patient at Ankaful Rehabilitation Centre).
The counsellor asked my mother to finish paying my fees on time to avoid my dismal because he uses the fees to look after us at centre (C: A 16 yr old male patient at Mercy Rehabilitation Centre).
It was therefore evident from the study that a patient’s ability to access rehabilitation services depended on his or her ability to pay for the services and the length of stay at the rehabilitation centre. Also, a patient’s ability to stay at a rehabilitation centre and to recover was contingent upon his or her ability to settle an associated rehab service bill. This, therefore, confirms what was revealed in the Selfdetermination Model of Rehabilitation by Deci and Ryan [15] that structural factors such as rehabilitation care organisation including payment for rehabilitation services affect behaviour and value priorities. The findings from the study also show that charging fees for rehabilitation services facilitated compliance and early recovery because patients feared to incur extra cost for their further stay at the rehabilitation centres. The Self-Determination Model of Rehabilitation [15] explains that patients’ ability to comply and recover is affected by personal and structural factors such as income and cost of rehabilitation services. The findings also support the position of Kant and Plummer [25] that cost of rehabilitation services affects patients’ compliance and recovery. Furthermore, Chosen Rehab [26] disclosed that the cost of rehabilitation services affects recovery of patients from addiction in that some patients leave rehabilitation centres unrecovered and vice versa due to the cost of services provided.
Diagnosis and medication
It emerged that after financial arrangements have been included, diagnostic tests were conducted to establish the severity of the patient’s condition. Also, it was mentioned by the service providers that the diagnoses were conducted to establish whether the patient had any associated health conditions that needed urgent and specific expert’s attention. They further reported that medications were also given to the patients to alleviate depression or other disorders which some of the patients might be suffering from. As some of the service providers pointed out:
A diagnostic test is conducted to establish the severity of the condition and type of medication to be prescribed. It (the diagnostic test) is also done to know any accompanied illness like heart diseases, liver problems, etc. (B: A 28 yr old male General Nursing service provider at Ankaful Rehabilitation Centre).
Some addiction conditions need urgent attention and so diagnostic test helps in early detection and treatment of those conditions with medication. Some of the patients come with severe addiction conditions and therefore medicines are administered to them to reduce the craving for a drug in them (M: A 26 yr old male Mental Health nursing service provider at Ankaful Rehabilitation Centre).
Similarly, the patients at both rehabilitation centres articulated that they were given medications after the service providers have assessed their conditions. They also elaborated that the medications helped them to regain consciousness and to recover from the pains.
My condition was assessed by the clinical psychologist who later brought some medicines to me to take and asked me to take it because that would help reduce the depression. After taking the medicines, about five hours later, I realised that my mood started changing and that continued for sometimes till I was not feeling for alcohol again (I: A 42 yr old married male patient at Ankaful Rehabilitation Centre).
The moment I got to the centre with my friend, the counsellor took me to a doctor for diagnosis and I was given medication by the doctor (B: A 38 yr old single male patient at Mercy Rehabilitation Centre).
It was discovered from the study that rehabilitation processes included diagnosis to assess the patient’s condition and the appropriate medicines to be prescribed. It was also evident from the study that diagnosis was conducted because patients might have different conditions and therefore had varied health needs including medication. In addition, it was identified from the study that different drugs used by patients might have different reactions and associated health conditions with different patients. In line with the findings, Republic of Kenya Ministry of Agriculture [27] identified that the severity of detoxification process varies from patient to patient depending on the substance used, how long the patient took the drug and at what dosage levels and any other addictions involved. Similarly, National Institute on Drug Abuse [12] recommends that alcohol and drug addiction patients should be assessed or diagnosed for the presence of co-occurring conditions and other infectious diseases. Targeted risk-reduction counselling services must also be provided to help patients modify or change behaviours that place them at risk of contracting or spreading infectious diseases [12].
Counselling and medication
Counselling and medication were explained by the service providers interviewed as the component of the processes involved in rehabilitation where alcohol and drug addiction patients were made to understand their condition and the risk associated with it in order to ensure readiness and compliance with the rehabilitation services. The service providers specified that patients were provided with daily routine individual and group counselling. According to them, the counselling provided involved guiding and advising the patients to accept their condition. The respondents further explained that the group counselling, which ensured catharsis, helped all the patients to interact and to share their experiences as well as to recognise that they were not alone with addiction and therefore this encouraged the patients to learn from one another. The group counselling, as indicated by the service providers, involved the 12 Steps of Alcoholics Anonymous. The respondents elaborated that the 12 Steps involved counselling and guiding the patients to accept their current condition of addiction in order to be helped to change behaviour and thoughts through group meetings and practices. The service providers also emphasised that the 12 Steps of Alcoholics Anonymous was where the patients were taught how to admit that they had a problem and therefore were ready to be helped and also to have good relationships with each other at the centre.
Counselling and at times medication is given to the patient until either the three, six, or twelve months registered for the patient elapses. The counselling we offer here basically depends on the 12 Steps of Alcoholics Anonymous where the patients are taught about admitting their condition and allowing us to help them. We offer individual and group therapies for the patients to better understand themselves and to promote group interest through group affiliation and interactions (H: A 34 yr old female General Nursing service provider at Ankaful Rehabilitation Centre).
Even though we are nurses here, we offer counselling based on the cognitive, physiological, behavioural, and social health of the patients to ensure that every part of the patient has recovered (D: A 29 yr old male General Nursing service provider at Ankaful Rehabilitation Centre).
The service providers acknowledged during the interview that they sometimes referred the patients to near-by hospitals for treatments of conditions were beyond their level of professionalism. The service providers mentioned liver cirrhosis, heart conditions, sight and hearing problems, and speech problems as some of the conditions that they normally referred to health care facilities. They again indicated that the referral fees were borne by the patients or their guardians because it was not included in the fees the patients’ guardians paid for the rehabilitation services.
The referrals assist us to provide additional services to the patients in our care because we are only nurses here and therefore we refer patients with conditions that need a doctor’s or any other person’s expertise (L: A 27 yr old female Mental Health Nursing service provider at Ankaful Rehabilitation Centre).
Some referrals are very expensive to the extent that the guardian of that patient has to bear the cost. Referrals involving the liver, heart, hearing, vision, etc. are very expensive and therefore the guardians of patients suffering from those conditions are made aware of the referrals (A: A 54 yr old male Counselling service provider at Mercy Rehabilitation Centre).
The patients at both Ankaful and Mercy Rehabilitation Centres and the two former inmates interviewed also reported that they were provided with food three times daily (that is, breakfast, lunch, and supper) by the service providers, medications when necessary, daily individual and group counselling. They also explained that the counselling helped them to stay focused on the rehabilitation process. Some of the patients further indicated that they were taken to other health facilities for treatment.
We go for group counselling every day with the service providers. We at times also go for individual counselling for us to express our personal sentiments to the service providers to enable them to help us. The service providers also administer medications to us whenever we are sick and so those of us on medications have to always take our medicines (E: A 25 yr old single male patient at Ankaful Rehabilitation Centre).
It was observed from the study that rehabilitation involving counselling and medication helped to address the physical, mental, and social health of the patients. It was also established that counselling promoted catharsis and patients became aware of the need to make changes in their life and behaviour. It was further identified from the study that as part of the rehabilitation, service providers used referral systems to assist patients in accessing health care services that were not available at the rehabilitation centres. It was therefore apparent from the study that rehabilitation further involved referral due to socioeconomic factors including limited skills and personnel, infrastructure, and logistics. United Nations Office on Drugs and Crime [24] also explained that rehabilitation helps patients to understand the main reasons behind their addictions. Consistent with these findings, Dennis and Scott [28] found that rehabilitation process usually includes group therapy because it allows recovering addiction patients to interact with their colleagues who are in the same situation. This encourages the patients and assures them that they are not alone in their struggles of rehabilitation and recovering. In a similar context, Deci and Ryan [15] also identified that relatedness deals with the desire to interact with, be connected to, and experience caring for other people and therefore actions and daily activities involve other people through which people seek a feeling of belongingness. According to Alcoholics Anonymous [29] cited in Humphreys [30], the main agent of change or recovery is group affiliation and practice of behaviour through attending meetings, self-reflection, and learning new coping strategy. That is, through group therapy a patient’s understanding of himself or herself and his or her relationships to others is transformed [30]. These findings also confirm what was revealed by United Nations Office on Drugs and Crime [24] that rehabilitation comprises physical, mental, and social healing as well as patient therapy and medication for associated health conditions.
Recovery plans
The service providers at both centres stated that the patient was provided with follow-ups services after recovery and discharge from the facility. The service providers also reported that the patient was given a referral note after recovery to be taken to the nearest health facility for any assistance if that patient lives far from rehabilitation centre concerned. The sole service provider at the Mercy Rehabilitation Centre further recounted that the follow-up took the form of referring the recovered patient to Alcoholics Anonymous (AA) group in his or her locality to attend AA meetings, which was necessary for sustaining recovery. Follow-ups, as explained by the service providers, were considered to help the recovered patients to sustain to avoid relapse of their conditions. As such, the respondents acknowledged the fact that inpatient/residential rehabilitation services alone did not guarantee a complete recovery because patients relapse and return to the centres for services either formally or informally. The reported challenges associated with the follow-ups, as identified by the service providers, were a loss to follow (unable to contact), limited phone credit to call the recovered patients, and unavailability of vehicles for travelling to the patients’ locations. A service provider emphasised this as:
Follow-ups are crucial to maintaining and sustaining the recovery by the patient and also because some patients do not recover fully before they leave the centre and therefore the follow-ups help them to recover. Some patients if not followed and monitored after they leave the centre, they may go home and relapse. Some patients also leave the centre not fully recovered because their guardians do not have money to pay for their stay to be extended till they have fully recovered (H: A 34 yr old female General Nursing service provider at Ankaful Rehabilitation Centre).
To confirm what the service providers said, the two former inmates who participated in the study explained that before they left the rehabilitation centres, their contacts were taken by the service providers in order to be checking on them. One of the former inmates indicated that the service providers used to visit him initially but stopped visiting as time went on. He also stated that he sometimes used to drink alcohol again because he did not recover fully before leaving the centre. However, the other former inmate articulated that he was always called or visited by the service provider: a situation which helped him to avoid relapse. A former inmate had this to say:
I did not recover fully before leaving the centre due to financial problems. The service providers promised to be assisting me at home and were coming initially but subsequently stopped the process. I was not hearing from them again so I thought I was left alone again. I sometimes take alcohol just to make me forget the loneliness (N*: A 26 yr old single male patient at Ankaful Rehabilitation Centre).
It therefore became patent from the study that even though followups assists patients to maintain a healthy condition and to recover fully, some service providers were unable to provide follow-ups services due to administrative challenges. Relapse of recovered patients was, thus, possible because of the inability of service providers to offer additional services to recovered and discharged patients to sustain their sobriety. Landale and Roderick [1] suggested that since recovery is a lifelong process, it may involve many life challenges and therefore lifelong support such as follow-up is essential.
Conclusion
It was evident from the study that variations in rehab services at the two centers were infrastructure and human resources; there were wellmaintained infrastructure but limited service providers at the private rehab centre than at the state-owned centre. The results from the study showed that the processes involved in rehabilitating individuals with addiction were unidirectional but multidimensional involving a limited interdisciplinary team of health professionals at the rehabilitation centres and paying attention to the full physical, psychological, emotional, and social makeup of the patients. Thus, the findings revealed that the unidirectional or linear processes involved in rehabilitating individuals with addiction were; recording the sociodemographic characteristics of the patients, their addiction history, making financial arrangements with patients for their stay, diagnostic tests and medication, counselling, and designing of recovery plans. The multidimensional concept, as explained by the respondents, involved an interdisciplinary team of health professionals such as physicians, a clinical psychologist, a counsellor, and nurses. However, the challenges recognised in the study were limited interdisciplinary team of health professionals, infrastructure, and inadequate follow-up logistics. Also, socio-demographic characteristics and addiction history of patients as a component of the rehabilitation processes had influences on rehabilitation activities, patients’ compliance, and recovery. Provision of appropriate and need-based rehabilitation services and activities to the patients at the centres were based on their socio-demographic characteristics and addiction history. However, the current rehabilitation processes did not take into consideration diversity and differences in the characteristics of the patients. The need-based services and activities were limited and as such provision of rehabilitation services were often performed to all the patients regardless of their socio-demographic characteristics and or addiction history. Consequently, the inadequate services most often resulted in patients’ noncompliance, relapse, service providers’ frustrations, and unfriendly relationship between patients and service providers.
Even though counselling and medication were important in facilitating patients’ compliance and recovery and catharsis, there were limited skilled personnel, infrastructure, and logistics at the rehabilitation centres studied. The addiction patients’ length of stay on the rehabilitation programmes and at the rehabilitation centres was determined by availability of rehabilitation facilities and skilled personnel, and their ability to pay for fees charged for the rehabilitation programmes. Consequently, the individuals with addiction’s ability to complete their rehabilitation programmes and recover from their addiction conditions was influenced by their length of stay in the programmes and ability to pay the fees as well as the nature or severity of their conditions. Individuals with alcohol and drug addiction may not fully recover from their condition and as such relapse could be possible due to the limited interdisciplinary team of health workers and the cost of rehabilitation programmes. Hence, recovery processes and the patients’ access to rehabilitation services could be hindered. The findings from this study, therefore, contribute to the paucity of literature on the dynamics of rehabilitation processes involve in rehabilitating individuals with alcohol and drug addictions in Ghana. Rehabilitation processes should be deemed necessary to improve the provision of effective rehabilitation outcomes and prevention of relapse. Consistently, more interdisciplinary team of rehabilitation service providers should be recruited and trained with relevant skills to improve multidimensional assessment of patients and to facilitate efficient provision of rehab services and emergency services for co-occurring conditions. It is also recommended that the government of Ghana, NGOs, and other benevolent individuals interested in rehabilitation of individuals with addiction should aid in the provision of more funds and other resources for the rehab services to reduce the cost of rehab services to patients to ensure their full recovery. In addition, more resources should be provided for follow-up logistics to prevent or reduce patients’ relapse and improve their family and community reintegration.
Authors’ Contributions
DA: performed the design of the study, executed the data collection, performed the data analysis, and served as the lead author of the manuscript. DTD: contributed to the design of the study, reviewed the manuscript for important scholarly content, and consented for the manuscript to be published. ABAG: participated in the design of the study, reviewed the manuscript for important scholarly content, and contributed to finalisation of the manuscript. All authors read and approved the final manuscript.
Acknowledgement
Our first and deep gratitude goes to the rehabilitation centres’ managements for the Ethical approval for this research. The authors would also like to acknowledge the tremendous contributions of the study participants for their participation and cooperation. In addition, we appreciate the efforts of all persons that contributed in various ways toward the success of this research.
References
- Landale S, Roderick M (2014) Recovery from addiction and the potential role of sport: Using a life-course theory to study change. International Review for the Sociology of Sport 49: 468-484.
- Sussman S, Lisha N, Griffiths M (2011) Prevalence of the addictions: A problem of the majority or the minority? Eval Health Prof 34: 3-56.
- Chandler KR, Fletcher BW, Volkow DN (2010) Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. JAMA 301: 183-190.
- Durrant R, Adamson S, Todd F, Sellman D (2009) Drug use and addiction: Evolutionary perspective. Aust N Z J Psychiatry 43: 1049-1056.
- Jeewa A, Kasiram M (2008) Treatment for substance abuse in the 21st century: A South African perspective. S Afr Fam Prac 50: 44.
- WHO (2010) The global status report on alcohol and health. Geneva: WHO.
- United Nations Office on Drugs and Crime (2012) World drug report 2012. New York: United Nations.
- WHO (2011) Expert committee on problems related to alcohol consumption. Geneva: WHO.
- United Nations (2012) Drug abuse kills 200,000 people each year: UN report. New York: United Nations.
- National Indigenous Drug and Alcohol Committee (2014) Alcohol and other drug treatment for Aboriginal and Torres Strait Islander peoples. Canberra: Australian National Council on Drugs.
- National Institute on Drug Abuse (2009) Treatment approaches for drug addiction: Department of Health and Human Services.
- WHO (2014) Resources for the prevention and treatment of substance use disorders. Geneva: WHO.
- Flora K, Stalikas AÂ (2013) Factors affecting substance abuse treatment across different treatment phases. Int J Rehabil Res 17:Â 89-104.
- Deci EL, Ryan MR (2008) Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychological Association 49: 182-185.
- Binney AF (2013) Increase in the intake of alcohol and drug abuse among the youth. Accra: Royal Kingdom Security Network.
- Ghana statistical service, Ghana health service & ICF Marco (2009) Ghana demographic and health survey 2008. Accra, Ghana: GSS, GHS, and ICF Macro.
- John-Langba J, Ezeh A, Guiella G, Kumi-Kyereme A, Neema S (2006) Alcohol, drug use, and sexual-risk behaviours among adolescents in four sub-Saharan African countries.
- Corbin J, Strauss A (2008) Basics of qualitative research. Thousand Oaks: Sage publication LDT.
- Prochaska JO, DiClemente CC (1983) Stages and process of self-change of smoking towards an integrative model of change. J Consult Clin Psychol 51: 390-395.
- Noar SM, Benac CN, Harris MS (2007) Does tailoring matter? Meta-analytic review of tailored print health behaviour change interventions. Psychol Bull 4: 673-693.
- Martin D (2012) Inpatient treatment for substance abuse offer quick recoveries.
- United Nations Office on Drugs and Crime (2003) Drug abuse treatment and rehabilitation: A practical planning and implementation guide. New York: United Nations.
- Kant CK, Plummer D (2012) Unpacking drug detoxification in Nepal: In-depth interviews with participants to identify reasons for success and failure. Int J Psych Rehab 16: 50-61.
- Rehab C (2013) Drug addicts and alcoholics need rehabilitation not jail term.
- Republic of Kenya Ministry of Agriculture (2012) Alcohol and drug abuse workplace policy. Nairobi: Agricultural information resource centre.
- Dennis M, Scott CK (2007) Managing addiction as a chronic condition. Addict Sci Clin Pract 4: 45-55.
- Alcoholics anonymous (2002) Twelve steps and twelve traditions. New York, NY: Alcoholics anonymous world services.
- Humphreys K (2006) The trials of alcoholics anonymous. Addiction 101: 617-618.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4835
- [From(publication date): 0-2018 - Dec 27, 2024]
- Breakdown by view type
- HTML page views: 4124
- PDF downloads: 711