Case Report Open Access
Rehabilitation of a Case of Post-Operative Paraplegia in Arthrogryposis Congenita Complex
Dziri S1, Mouhli N2*, Miri I1 and Dziri C1
1Department of Physical and Rehabilitation Medicine, National Orthopaedic Institute Mohamed Taieb Kassab, Manouba
2Medical School of Tunis, University of Tunis El Manar, Tunisia
- Corresponding Author:
- Dr. Najla Mouhli, M.D
Medical School of Tunis
University of Tunis El Manar, Tunisia
Tel: +21654448048
E-mail: najla.mouhli@gmail.com
Received Date: October 30, 2016; Accepted Date: February 02, 2017; Published Date: February 10, 2017
Citation: Dziri S, Mouhli N, Miri I, Dziri C (2017) Rehabilitation of a Case of Post-Operative Paraplegia in Arthrogryposis Congenita Complex. J Nov Physiother 7:332. doi:10.4172/2165-7025.1000332
Copyright: © 2017 Dziri S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Arthrogryposis is an orthopedic condition characterized by greater or lesser stiffness at the four members and less frequently of the spine. Treatment is with certain orthopedic surgical indications in functional aim. The purpose of this work is to present a complex case of arthrogryposis multiplex congenita with partially reversible neurological complications following spinal surgery.
Presentation of the case of a ten year old boy, who had previous surgeries in the lower limbs, addressed in the department of Physical and Rehabilitation Medicine of the National Orthopaedic Institute Mohamed Taieb Kassab, twenty one days after a kyphosis and lumbar dorsal scoliosis surgery complicated by paraplegia justifying the removal of material. The clinical examination at the admission found a paraplegia ASIA C D4 with neurogenic bladder. The multidisciplinary care was provided in the department of Physical and Rehabilitation Medicine in two hospitalizations with progressive goals (analgesia, joint gain, standing up, walk, urinary autonomy and rehabilitation).
Six months after the second hospitalization, the child had regained the standing position, walking with adapted equipment, and bladder balance.
Arthrogryposis manifests by stiff joints, interesting the four members, with skin abnormalities and occurs in children with normal intelligence. Treatment is based on assiduous care with physiotherapy care, occupational therapy and early orthopedic continued throughout growth. Surgical treatments deformations there are delicate, with poorer results than in idiopathic etiology.
The management in physical medicine were based on multidisciplinary cares, enabling the patient to walk, to have a better autonomy and urinary balance, allowing to hope for a good family and social insertion, particularly the resumption of his schooling.
Keywords
Arthrogryposis congenital complex; Kyphoscoliosis; Surgery; Paraplegia; Rehabilitation; Urinary care
Introduction
Arthrogryposis is an orthopedic disease characterized by joint stiffness and contractures affecting at least two different areas of the body. However, it can affect the 4 limbs and less frequently the spine. It is the occurrence of joint contractures of variable etiologies that start prenatally. It may result from neurologic deficit, neuromuscular disorders, connective tissue abnormalities, amniotic bands or fetal crowding. Mostly no hereditary causes are found (neuropathic, e.g.), and search for hereditary factors need to be done (myopathic form) [1]. Some authors define arthrogryposis as a non-progressive congenital rigidity disorder that affects multiple joints [2,3].
There are around 150 symptoms that are associated with multiple congenital contractures. Arthrogryposis is a part of an heterogeneous group of some 300 different conditions with a variety of etiologies. Congenital amyoplasia, the most common type of congenital arthrogryposis, usually results from impaired blood flow to the placenta leading to the death of the embryo’s marrow [4,5].
Although arthrogryposis has been thought of as a rare condition, it actually occurs in between one in 3000 and one in 5000 live births [6]. However, each specific type is relatively rare. The most common type of arthrogryposis is the sporadic one, amyoplasia. It’s frequency is one in 10,000. Arthrogryposis multiplex congenita is rarer, with a previously underestimated incidence of 1 in 3000 live births approximately, but 7 more recent studies have estimated the incidence to be between 1 in 4300-5100 [7-9].
Treatment is based on orthopedic and rehabilitative management, though surgery may be suggested in some cases for functional purposes. The aim of treatment is to ensure maximum independence for the patients.
Case Report
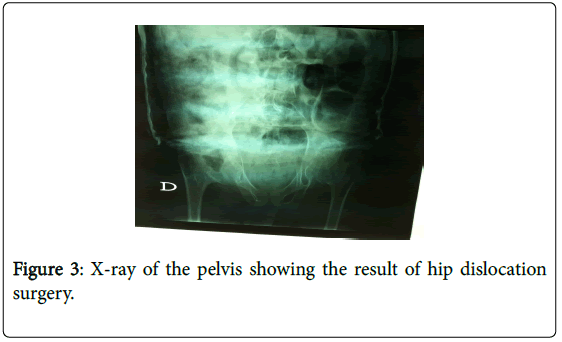
This case report is about a ten-year-old boy, suffering from stiffness in the lower limbs and spine. He first presented with gait disorders in 2006. The course was marked by worsening deformities for which had undergone several surgical operations. Indeed, he was first operated on the age of two for congenital hip dislocation, and then at the age of 6 for abnormal static knee by Judet’s intervention, with good results. In June 2014, he had a cyphoscoliosis surgery (anterior and posterior time), that was complicated by paraplegia justifying the removal of material 3 hours after surgery, relayed by corset cover in plaster.
He had been refferd to our service of Physical Medicine and Rehabilitation (PMR) of the National Institute of Orthopaedy M.Kassab in Tunisia 21 days after the surgery. The physical examination on admission revealed a paraplegia classified ASIA C D4, that is to say that motricity was kept below the line of the nipples but more than half of the tested muscles below this level had a score inferior to 3. In addition to this, he had urinary disturbances as a result of decrease in the perception of urge to urinate and continuous urinary leaks requiring wearing diapers.
The impatient management required two hospitalizations 6 months apart, with progressive objectives adapted to every phase. The patient was taken care of by a multidisciplinary team including doctors, physiotherapists, occupational therapists, nurses and psychologists.
During his first hospitalization, in June, the child still had his plaster corset, so his management wasn’t easy, but we focused on pain management by soft massage using an analgesic cream, and analgesic electrotherapy to obtain a total cooperation of the patient. The management of spasticity used almost passive movements: muscle stretching and immobilization in lengthened positions to decrease contractures caused by the spasticity, joint mobilizations to improve joint stiffness, muscular training in lower limbs and strengthening in the upper limbs to get a better autonomy in bed (turning over, sitting …) and to allow him to stand from the bed and walk easier with assistance. Besides that, we perform a respiratory rehabilitation in corset to fight pulmonary infections and ventilations disorders. Therapeutic education of the mother was made to teach her rehabilitation exercises. Throughout the patient’s and his mother stay, supportive psychotherapy was provided by all the health care staff.
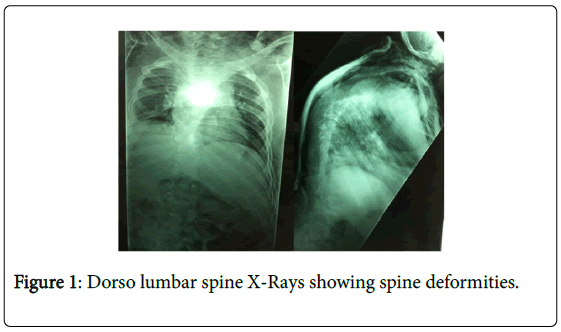
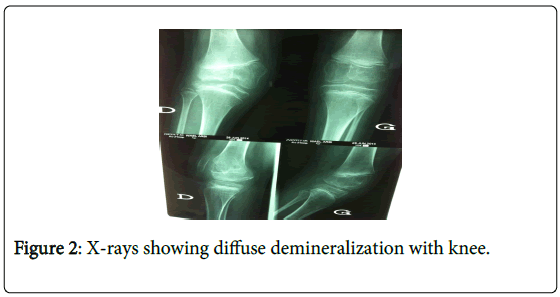
X-rays showed a significant spinal deformity with kyphosis and lumbar dorsal scoliosis, large deformity of the pelvis as well as a fracture of the knees, with bone demineralization (Figures 1-3). Urinary ultrasonography was normal.
After a 4 weeks’ stay in hospital, the orthopedic surgeon decided to remove the plaster corset and discharged the patient to go back home for a few months, with self-rehabilitation under the mother’s supervision.
During this period, his equipments (which consisted of a Garchois corset and two lower extremity splints) was made.
During his second hospitalization in December of the same year, the child had no plaster corset, and had acquired his equipment that he wore throughout the rehabilitation sessions (Figure 4).
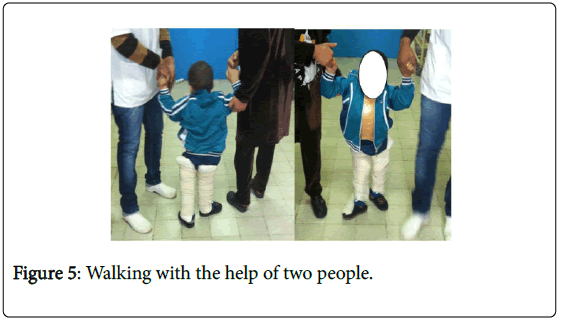
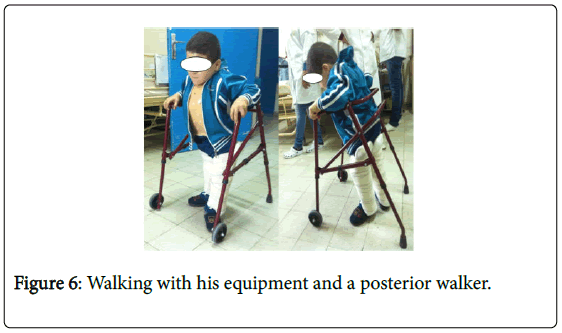
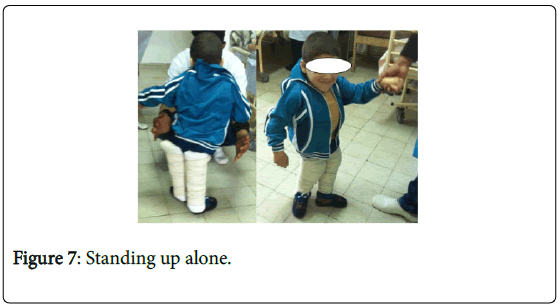
His management was at that time easier and more specific. Indeed, we started by working on the sitting balance to erect the trunk and to avoid orthostatic hypotension phenomena, then we worked on standing up. This work was made progressively. At first, the child was set in vertical position on an electric table, with an angle of progressively increasing verticalization. As soon as the complete verticalization was well tolerated (90°), the child was put on the standing up table (with support for the upper limbs and maintain of extension of the lower limbs) with progressive duration: 10 minutes on the first day, then 20 and finally 30 minutes. After that, the young patient was able to stand up on the floor with assistance, and started walking between parallel bars. Here too, we did it progressively, from a few steps up to a few meters. Once the patient felt comfortable between the parallel bars, he began walking with his mother’s assistance (Figure 5) then alone with a posterior walker (Figures 6 and 7). Of course, the basis of rehabilitation was continued throughout this hospital stay as muscular stretching and strengthening and joint mobilisations. As for the urinary disorders, the child had two perineal rehabilitation sessions.
Results
After 6 months of follow-up by a multidisciplinary team in Physical Medicine and Rehabilitation department, we achieved encouraging results. Indeed, the child had less painful phenomena, measured by the Faces Pain Rating Scale, there had been an improvement in muscle testing of the lower limbs, with a gain by a point per muscle (MRC scale), and a decrease in spasticity, listed in 1 of the modified Aschworth scale of spasticity. The passive articular mobilizations allowed an increase in the range of motion. The child had a better sitting and a stable standing positions; he was also able to turn over in bed no longer without the help of his mother and to walk with a posterior walker for several meters or with his mother’s assistance. Concerning the urinary disorders, he wore no longer diapers in the day time but still had some disorders of the bladder sensivity explaining some nocturnal leaks.
All these improvements explain this improved autonomy and allowed him to lead an acceptable social life for his age.
Moreover, a medical certificate was delivered to his mother to have a suitable chair and a table at school, in order to allow him to continue his studies.
Discussion
Arthrogryposis is a congenital, non-progressive disorder. The term designates a collection which regroups collection of conditions of varying etiologies that are characterized by joint stiffness and contractures affecting at least two different areas of the body, [10] arthrogryposis multiplex congenita (AMC) is defined as a nonprogressive congenital rigidity disorder that affects multiple joints [2,3]. Arthrogryposis is a symptom rather than a diagnosis. It implies contractures in multiple body areas usually involving the limbs, but may also include limitation of full range of movement of the jaw, neck, and spine at birth [11]. As for our patient, the joint stiffness was present at birth and involved the entire spine, hips, knees and ankles, leading to multiple deformities, especially hips dislocation, knees static disorders and valgus foot slope, generating delayed motor skills. Joint development occurs during embryogenesis in the first 8 weeks of intrauterine life. Impairment of intrauterine movement leads to contractures, and the more severe the restriction in movement is, or the longer it occurs, the worse are the resultant contractures [12,13]. This condition is evident at birth, but a diagnosis of arthrogryposis may be suspected if prenatal ultrasound examination shows an absence of fetal movement, especially if accompanied by polyhydramnios [14]. There may be a family history of an arthrogrypotic condition, which allows prenatal testing [11]. The mother of our patient had not followed her pregnancy, so we do not have data on the fetal period. At birth, children will have fixed contractures and the limbs are tubular and featureless, lacking the normal skin creases seen around joints. A deep dimple is often seen over joints as a result of the skin being adherent to the underlying bone. The trunk may also be affected and devoid of creases, giving a characteristic appearance. When the upper limbs are affected, they take a particular attitude: shoulders on internal rotation and adduction, elbows fixed on extension, wrists on palmar flexion and ulnar deviation, thumbs on adduction into the palms, and fingers fixed in a flexed posture. In the lower limbs, the hips are flexed, abducted and externally rotated, congenital dislocation of the hips may also be seen. The most common lower limb deformities are rigid clubfoot and knee contractures, which are more commonly extended, rather than flexed. The limbs are not painful, but there is only a little movement in the affected joints with an inelastic endpoint beyond a limited range of movement [15]. Scoliosis is reported in 10-30% of cases [11]. The sensation is intact. As for our child, his upper limbs were safe, and the pathology affected the legs with hips dislocation, knee contractures fixed on extension, and the spine with kyphosis and lumbar dorsal scoliosis for which he had been operated on when he was 10. His had also a preserved sensation.
Concerning urinary disorders, different studies concluded that neurogenic bladder can be found in patients with arthrogryposis. In infancy, it is generally a congenital disease and can result in various neurological disorders that may affect the innervations of the lower urinary tract, such as myelomeningocele and sacral agenesis. In patients with arthrogryposis, urinary tract disorders seem to have the same origin as disorders of the spinal cord. There may be neurogenic changes, like damage to the anterior horn cells of the spinal cord, probably due to maternal hypertension and focal hypoxia during early pregnancy, or even as a result of an intrauterine vascular accident. Urinary incontinence is the most frequent clinical symptom and urodynamic evaluation revealed a predominance of detrusor overactivity, followed by changes in detrusor compliance [16-20].
The urinary ultrasound may be normal (61%), like in our patient or show ectasia, dilatation or post-voiding residual [14,16].
The two main goals of management in arthrogryposis are, firstly, to maintain ambulation, and secondly, to preserve independent function of the upper limbs, to preserve the activities of daily living [11], but in our case the support included the paraplegia too. These are Some tips for a successful management: to address lower limb misalignment to allow a standing posture with the foot flat to the floor, maintain preexisting joint mobility and ensure that the movement is within a useful range for activities of daily living, consider the use of muscle or tendon transfers to enhance active movement if it’s possible and bring stiff joints into positions that aid function. The management must have a minimal impact on the development; treatment will differ depending on the age of the child. In infancy, the early use of splintage and gentle manipulation are common practice.
Corrective surgery, focused on addressing lower limb deformity that would prevent standing and walking can be done early, like in our patient who had a surgical correction of his hips dislocation. As for the upper limbs, surgery is usually delayed until later in childhood so that adequate assessment of hand function can be made, to allow the surgical intervention to be individualized to the child’s needs. However, major joint repositioning surgery should probably be performed before the age of four. With increasing age, there is increasing occurrence of the joint stiffness and limbs abnormal positions [14].
For the rehabilitation management, we had to combine two intricate rehabilitative programs: one for arthrogryposis and one for paraplegia. The arthrogryposis one is mostly based on passive articular mobilizations in the lower limbs and strength training is primarily via active work against manual resistance [11,15].
As for the paraplegic one, the care includes progressive verticalization programs and early get up (cardiopulmonary rehabilitation orthostatic), muscle strengthening in the upper limbs and trunk according to level, maintaining a correct orthopedic condition and working trunk balance. Working on transfers and all the techniques needed to preserve the patient’s autonomy in all acts of daily life (food, washing, dressing, transfers ...) is common to both programs. The walking rehabilitation is essential in the patient with incomplete paraplegia. It can be done with an orthotic device, after getting a good balance standing.
We also need to assure a pulmonary rehabilitation insofar as the respiratory complications are the second cause of death (28%) during the first year post paraplegia [21-23].
Reintegration tries to compensate for the deficiencies and limitations activities (disabilities) that persist despite rehabilitation, with the aim of allowing the best possible integration of the person in their environment. This process requires some material assistance such as medical devices and technical aids, aids to rehabilitation, human helps, adaptations of the environment in the private or public domain [23,24]. That is what we did with our patient when we gave the mother a certificate to get him an adapted chair and table for school for example.
Besides, the follow-up of a child with arthrogryposis should include the investigation of urinary symptoms. If they are absent, only a renal ultrasonography and serum creatinine need to be performed, because it is unlikely that additional testing would reveal further abnormalities. When the clinical history is positive, uroflowmetry and urodynamic evaluation should be considered. If the tests confirm neurogenic bladder, treatment should be instituted early (anticholinergics and clean intermittent catheterization) and if not, frequent follow-up visits are advised [13]. Our patient had a decrease in the perception of urge to urinate and leakages. His urinary ultrasound was normal as well as his laboratory findings.
Conclusion
Management in physical medicine should be based on multidisciplinary care, and should aim at enabling the patient to walk, to have a better autonomy and a urinary balance, allowing the hope for a good family and social insertion, particularly the resumption of his schooling.
Management of arthrogryposis in a PMR department is indicated at all stages, including the perioperative period and in case of complications.
References
- Bonilla-Musoles F, Machado LE, Osborne NG (2002) Multiple congenital contractures (congenital multiple arthrogryposis). J Perinat Med 30: 99-104.
- Mennen U, van Heest A, Ezaki MB, Tonkin M, Gericke G (2005) Arthrogryposis multiplex congenita. J Hand Surg Br 30: 468-474.
- Narkis G, Ofir R, Manor E, Landau D, Elbedour K, et al. (2007) Lethal congenital contractural syndrome type 2 (LCCS2) is caused by a mutation in ERBB3 (Her3), a modulator of the phosphatidylinositol-3-kinase/Akt pathway. Am J Hum Genet 81: 589-595.
- Hall JG, Reed SD, Greene G (1982) The distal arthrogryposis: delineation of new entities-review and nosologic discussion. Am J Med Genet 11: 185-239.
- Herva R, Conradi NG, Kalimo H, Leisti J, Sourander P (1988) A syndrome of multiple congenital contractures: neuropathological analysis on five fetal cases. AmJ Med Genet 29: 67-76.
- Lowry RB, Sibbald B, Bedard T, Hall JG (2010) Prevalence of multiple congenital contractures including arthrogryposis multiplex congenital in Alberta, Canada, and a strategy for classification and coding. Birth Defects Res Part A: ClinMolTeratol 88: 1057-1061.
- Hall JG, Reed SD, Driscoll EP (1983) Part I. Amyoplasia: a common, sporadic condition with congenital contractures. Am J Med Genet 15: 571-590.
- Darin N, Kimber E, Kroksmark AK, Tulinius M (2002) Multiple congenital contractures: birth prevalence, etiology, and outcome. J Pediatr 140: 61-67.
- Hall JG, Aldinger KA, Tanaka KI (2014) Amyoplasia revisited. Am J Med Genet A 164A: 700-730.
- Ferguson J, Wainwright A (2013) Arthrogryposis, Children orthopaedics. 27: 171-180.
- Hall JG (2014) Arthrogryposis (multiple congenital contractures): Diagnostic approach to etiology, classification, genetics, and general principles. Eur J Med Genet 57: 464-472.
- Moessinger AC (1983) Fetal akinesia deformation sequence: an animal model. Pediatrics 72: 857-863.
- Hall JG, Opitz JM, Reynolds JF (1986) Analysis of Pena Shokeir phenotype. Am J Med Genet 25: 99-117
- Piper SL, Dicke JM, Wall LB, Shen TS, Goldfarb CA (2015) Prenatal Detection of Upper Limb Differences With Obstetric Ultrasound. J Hand Surg Am 40: 1310-1317.
- Azbell K, Dannemiller L (2015) A Case Report of an Infant With Arthrogryposis. PediatrPhys Ther27: 293-301.
- Arantes de Araújo L, Ferraz de ArrudaMusegante A, de Oliveira Damasceno E, Barroso U Jr, Badaro R (2013) Investigation into neurogenic bladder in arthrogryposis multiplex congenital. J Pediatric Urol 9: 895-899.
- Arantesde Araújo L, Ferraz de ArrudaMusegante A, de Oliveira Damasceno E, Barroso U Jr, Badaro R (2013) Investigation into neurogenic bladder in arthrogryposis multiplex congenita. J PediatrUrol 9: 895-899.
- Merenda L, Brown JP (2004) Bladder and bowel management for the child with spinal cord dysfunction. J Spinal Cord Med 27 Suppl 1: S16-23.
- Banker BQ (1986) Arthrogryposis multiplex congenita: spectrum of pathologic changes. Hum Pathol 17: 656-672.
- Hall JG (1985) Genetic aspects of arthrogryposis. ClinOrthopRelat Res 194: 44-53.
- Coelho KE, Sarmento MF, Veiga CM, Speck-Martins CE, Safatle HP, et al. (2011) Misoprostol embryotoxicity: clinical evaluation of fifteen patients with arthrogryposis. Am J Med Genet 95: 297-301.
- HAS (2007) Service des affections de longue durée et accords conventionnels ADL 20 Paraplégie.
- Roulet V, Gourdon C, Santisteban L (2008) Exercicesthérapeutiques en vue de la reprise de la marche du paraplégique incomplete.Kinesither Rev(80-81): 53-62.
- Albert(2012) Physical and rehabilitation medicine (PRM) care pathways: “Spinal cord injury”. Ann PhysRehabil Med 55: 440–450.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 3865
- [From(publication date):
April-2017 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 2967
- PDF downloads : 898