Refractory Septic Shock due to Acute Cholangitis Successfully Treated with Polymyxin B Hemoperfusion: A Case Report
Received: 02-May-2019 / Accepted Date: 14-May-2019 / Published Date: 21-May-2019 DOI: 10.4172/2161-069X.1000597
Abstract
A 76-year-old man was transferred to our department because of high fever with chills. According to the Tokyo Guidelines 2018, he was diagnosed with sepsis due to Grade III (severe) acute cholangitis. Fluid resuscitation, noradrenaline administration, antibiotic therapy, and an emergency endoscopic retrograde biliary drainage were
performed. Due to these treatments, his general condition improved initially; however, on the 5th hospital day, he eventually became persistently hypotensive despite adequate fluid resuscitation while on a vasopressor. Under the diagnosis of septic shock, intensive care including endotracheal intubation followed by mechanical ventilation, thoracic drainage, administration of vasopressors, strict antibiotic therapy, and total parenteral nutrition, was promptly initiated; however, he remained in shock. We judged his condition as refractory septic shock that was resistant to conventional treatments. Therefore, endotoxin adsorption therapy with polymyxin B hemoperfusion (PMX-DHP) was attempted on the 7th hospital day, and two sessions of PMX-DHP were carried out 24 h apart. Following this procedure, he successfully recovered from septic shock, and was discharged on the 84th hospital day.
We propose that PMX-DHP might be considered for the treatment of refractory septic shock due to acute cholangitis that is resistant to appropriate conventional treatments, especially when the presence of endotoxemia has been confirmed.
Keywords: Septic shock; Acute cholangitis; Polymyxin B hemoperfusion
Introduction
Acute cholangitis is one of the most emergent and severe diseases of the digestive system, and its prognosis depends on early diagnosis followed by prompt and optimal treatment. Despite recent advances in the management of acute cholangitis, approximately 5% of all patients with this disease have a poor prognosis [1], with septic shock being the major cause of fatality. We report a case of refractory septic shock due to acute cholangitis that was resistant to conventional treatments and was successfully treated with polymyxin B-immobilized fiber column direct hemoperfusion (PMX-DHP).
Case Report
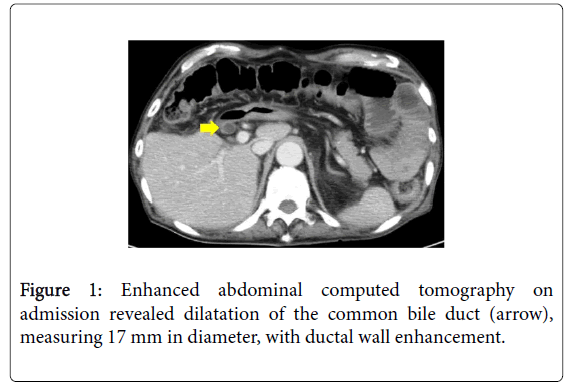
A 76-year-old man was transferred to our department because of high fever with chills. He had undergone open cholecystectomy for cholecystolithiasis 28 years previously. On admission, he appeared drowsy; his Glasgow Coma Scale score was 13 (E3V4M6). Body temperature was 40.2oC; heart rate, 122 bpm; respiratory rate, 28 breaths/min; blood pressure, 74/49 mmHg; and peripheral arterial oxygen saturation (SpO2), 85% (under room air). Physical examination revealed that his abdomen was slightly distended, with mild tenderness in the right upper quadrant, and the extremities were warm. Laboratory test results indicated a severe inflammatory response, obstructive jaundice, liver dysfunction, Disseminated Intravascular Coagulation (DIC), and endotoxemia (Table 1). A blood sample culture revealed the presence of Klebsiella pneumoniae. The Sequential Organ Failure Assessment (SOFA) score was 12, and abdominal computed tomography revealed dilatation of the common bile duct (Figure 1).
| Hematology | Blood chemistry | Arterial blood gas (O2 6 L/min facial mask) | |||
|---|---|---|---|---|---|
| WBC | 51,900/mm3 | Albumin | 1.8 g/dL | pH | 7.444 |
| Myelo | 1% | TB | 3.5 mg/dL | PaCO2 | 23.7 Torr |
| Meta | 7% | DB | 2.2 mg/dL | PaO2 | 89.4 Torr |
| Stab | 18% | AST | 59 IU | HCO3- | 16.0 mmol/L |
| Seg | 71% | ALT | 43 IU | Base excess | -6.8 mmol/L |
| Lymph | 1% | LDH | 345 IU | Lactate | 2.6 mmol/L |
| RBC | 242 ×106/mm3 | ALP | 838 IU | ||
| Hb | 8.1 g/dL | γGTP | 159 IU | Others | |
| Ht | 23.8% | BUN | 41.6 mg/dL | Endotoxin | 14.5 pg/mL |
| Plt | 1.7 × 104/mm3 | Cr | 1.08 mg/dL | Procalcitonin | >100 ng/mL |
| Na | 133 mEq/L | BNP | 50.1 pg/mL | ||
| Coagulation | K | 3.9 mEq/L | |||
| PT | 20.4 sec | Cl | 107 mEq/L | ||
| PT-INR | 1.61 | Amylase | 47 IU | ||
| FDP | 40.1 μg/mL | Glucose | 119 mg/dL | ||
| AT III | 41% | CRP | 10.2 mg/dL | ||
Table 1: Laboratory data on admission.
According to the Tokyo Guidelines 2018 (TG18) [2], he was diagnosed with sepsis due to Grade III (severe) acute cholangitis; therefore, O2 administration using a facial mask, fluid resuscitation, noradrenaline administration, antibiotic therapy, and anticoagulation therapy were promptly initiated. Immediately after his hypotension had been stabilized with circulatory support, an emergency endoscopic retrograde cholangiography was performed, followed by biliary drainage. Although a definitive etiology of cholangitis was not demonstrated, a substantial amount of biliary sludge debris was drained through the drainage tube. Due to these treatments, inflammatory response and DIC were controlled, and his general condition improved. However, on the 5th hospital day, high fever with chills recurred, and his blood pressure and SpO2 worsened with a concomitant elevation of total bilirubin and C-reactive protein levels. The following day, his blood pressure continuously decreased despite adequate fluid resuscitation while on a vasopressor, and he developed acute respiratory failure with altered mental status. Arterial blood gas analysis revealed hyperlactatemia (lactate level was 3.0 mmol/L) and severe hypoxia (arterial partial pressure of O2/fraction of inspired O2 [P/F] ratio was 155 mmHg).
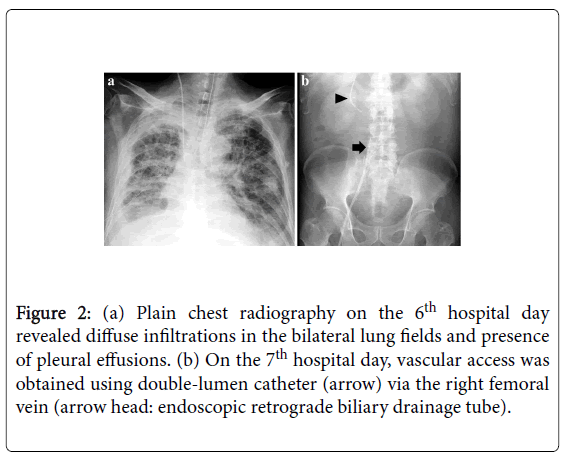
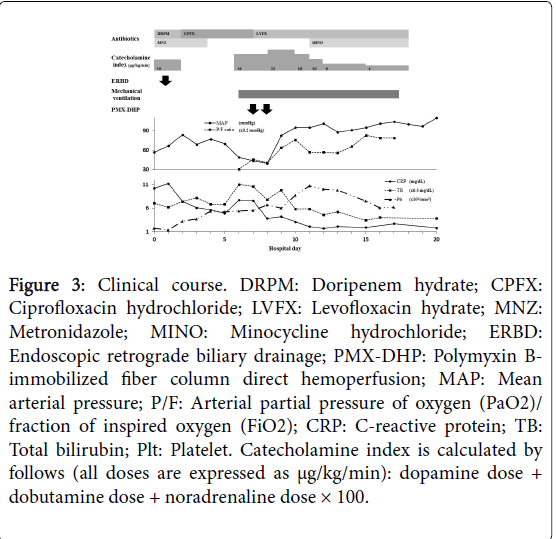
The SOFA score was 14, and plain chest radiography revealed diffuse infiltrations in the bilateral lung fields (Figure 2a). Under the diagnosis of septic shock complicated with Acute Respiratory Distress Syndrome (ARDS), emergency endotracheal intubation and right thoracic drainage were performed, and intensive care including mechanical ventilation, administration of vasopressors, strict antibiotic therapy, and Total Parenteral Nutrition (TPN), was promptly initiated. However, high doses of catecholamines were required to maintain his hemodynamics because of persistent hypotension, and he remained in shock. We judged his condition as refractory septic shock that was resistant to conventional treatments; therefore, we decided to attempt endotoxin adsorption therapy with PMX-DHP on the 7th hospital day. Vascular access catheter was inserted via the right femoral vein (Figure 2b), and hemoperfusion using Toraymyxin TM (Toray Industries, Tokyo, Japan) at a blood flow rate of 120 mL/min was performed for 3 h. Two sessions of PMX-DHP were carried out 24 h apart, with no adverse events. Following this procedure, endotoxin level decreased to th hospital day, he was withdrawn from mechanical ventilation and TPN (Figure 3). The following clinical course was uneventful. Although he required a long period of rehabilitation to regain his respiratory function, swallowing ability, and ambulation, he was discharged on the 84th hospital day in good health.
Figure 2: (a) Plain chest radiography on the 6th hospital day revealed diffuse infiltrations in the bilateral lung fields and presence of pleural effusions. (b) On the 7th hospital day, vascular access was obtained using double-lumen catheter (arrow) via the right femoral vein (arrow head: endoscopic retrograde biliary drainage tube).
Figure 3: Clinical course. DRPM: Doripenem hydrate; CPFX: Ciprofloxacin hydrochloride; LVFX: Levofloxacin hydrate; MNZ: Metronidazole; MINO: Minocycline hydrochloride; ERBD: Endoscopic retrograde biliary drainage; PMX-DHP: Polymyxin Bimmobilized fiber column direct hemoperfusion; MAP: Mean arterial pressure; P/F: Arterial partial pressure of oxygen (PaO2)/ fraction of inspired oxygen (FiO2); CRP: C-reactive protein; TB: Total bilirubin; Plt: Platelet. Catecholamine index is calculated by follows (all doses are expressed as µg/kg/min): dopamine dose + dobutamine dose + noradrenaline dose × 100.
Discussion
An international practice guideline for acute cholangitis was initially developed in 2007 as the Tokyo Guidelines 2007 [3], and it was revised as the TG18 in 2018. According to the TG18, principles of management for acute cholangitis consist of antibiotic therapy, biliary drainage, and treatment of the etiology, and for Grade III cholangitis, which is defined as cholangitis with sepsis-induced organ damage, biliary drainage should be performed as soon as possible after the patient’s general condition has improved by respiratory/circulatory support [2]. However, even when appropriately managed in accordance with the TG18, treatment-resistant and life-threatening acute cholangitis is certainly present, and the mortality rate of Grade III cholangitis has been reported to be 8.4% [1]. In addition, extensive spread of antimicrobial resistance among gram-negative bacteria, such as extended-spectrum β-lactamase-producing gram-negative bacilli, makes it difficult to treat affected patients [1].
Polymyxin B (PMX), which is a cyclic cationic polypeptide antibiotic derived from Bacillus polymyxa, exhibits antimicrobial activity against gram-negative bacteria and the ability to bind to and neutralize endotoxin [4]. However, intravenous administration of PMX is limited because of its nephrotoxicity and neurotoxicity [5]. To retain the endotoxin-binding and neutralizing properties as well as to minimize systemic toxicity, PMX was immobilized to a polystyrene fiber column, and this column was connected to an extracorporeal hemoperfusion circuit to adsorb circulating endotoxin. This endotoxin adsorption and removal system was initially designed in Japan in the 1980s and developed as PMX-DHP [6] and has been used for the treatment of septic shock. Regarding the target of PMX-DHP therapy, the most frequent etiology of septic shock is intra-abdominal infection, particularly peritonitis due to gastrointestinal perforation [5,7,8]. However, the definite indication criteria of PMX-DHP therapy have not been established yet, and the clinical efficacy of this therapy for septic shock remains debatable [5,7-11]. Several studies [7,9] reported that PMX-DHP significantly improved hemodynamics and organ functions and reduced the 28-day mortality in patients with septic shock. However, several other studies [8,10] reported controversial results. Recently, using PMX-DHP, survival benefit in septic shock with high disease severity and/or elevated endotoxin level, as in our case, has been suggested [9,11], and several authors [5,9,11] have described that selecting appropriate patients for PMX-DHP therapy is essential to improve prognosis of septic shock. Adverse events related to PMX-DHP including hemodynamic instability, decrease in platelet count, hemorrhage, and technical problems, are sometimes considerable [9]; therefore, establishment of strict indication criteria of this high-cost but promising therapy is expected.
To the best of our knowledge, apart from this report, a similar case report exists in the English literature, which used PMX-DHP for the treatment of cholangitis-induced septic shock [12]. From our experience, although it is not mentioned in the TG18, PMX-DHP might be an acceptable option for the treatment of cholangitis-induced septic shock that is resistant to combination of antibiotic therapy, biliary drainage, and respiratory/circulatory support. Because of the lack of experience, it is unclear which patients with cholangitisinduced septic shock will benefit from PMX-DHP therapy; however, we believe that the presence of endotoxemia might be one of the indication criteria of PMX-DHP for the treatment of cholangitisinduced refractory septic shock.
Conclusion
We propose that PMX-DHP might be considered for the treatment of refractory septic shock due to acute cholangitis that is resistant to appropriate conventional treatments, especially when the presence of endotoxemia has been confirmed.
Conflicts of Interest
Conflict of interest disclosed was none.
References
- Gomi H, Takada T, Hwang TL, Akazawa K, Mori R, et al. (2017) Updated comprehensive epidemiology, microbiology, and outcomes among patients with acute cholangitis. J Hepatobiliary Pancreat Sci 24:310-318.
- Miura F, Okamoto K, Takada T, Strasberg SM, Asbun HJ, et al. (2018) Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci 25:31-40.
- Mayumi T, Takada T, Kawarada Y, Nimura Y, Yoshida M, et al. (2007) Results of the Tokyo Consensus Meeting Tokyo Guidelines. J Hepatobiliary Pancreat Surg 14:114-121.
- Davies B, Cohen J (2011) Endotoxin removal devices for the treatment of sepsis and septic shock. Lancet Infect Dis 11:65-71.
- Matsukuma S, Sakamoto K, Nishiyama M, Tamesa T, Yoshino S, et al. (2015) Prognostic factors in patients with septic shock in digestive surgery who have undergone direct hemoperfusion with polymyxin B-immobilized fibers: a retrospective observational study. J Intensive Care 3:13.
- Hanasawa K, Tani T, Oka T, Yoshioka T, Aoki H, et al. (1988) Selective removal of endotoxin from the blood by extracorporeal hemoperfusion with polymyxin B immobilized fiber. Prog Clin Biol Res 264:337-341.
- Cruz DN, Antonelli M, Fumagalli R, Foltran F, Brienza N, et al. (2009) Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA 301:2445-2452.
- Payen DM, Guilhot J, Launey Y, Lukaszewicz AC, Kaaki M, et al. (2015) Early use of polymyxin B hemoperfusion in patients with septic shock due to peritonitis: a multicenter randomized control trial. Intensive Care Med 41:975-984.
- Chang T, Tu YK, Lee CT, Chao A, Huang CH, et al. (2017) Effects of polymyxin B hemoperfusion on mortality in patients with severe sepsis and septic shock: a systemic review, meta-analysis update, and disease severity subgroup meta-analysis. Crit Care Med 45:e858-e864.
- Dellinger RP, Bagshaw SM, Antonelli M, Foster DM, Klein DJ, et al. (2018) Effect of targeted polymyxin B hemoperfusion on 28-day mortality in patients with septic shock and elevated endotoxin level: the EUPHRATES randomized clinical trial. JAMA 320:1455-1463.
- Iba T, Fowler L (2017) Is polymyxin B-immobilized fiber column ineffective for septic shock? A discussion on the press release for EUPHRATES trial. J Intensive Care 5:40.
- Inoue Y, Fujino Y, Onodera M, Kikuchi S, Takahashi G, et al. (2013) Endotoxin adsorption therapy using polymyxin B-immobilized fiber as a treatment for septic shock-associated severe acute cholangitis. Clin J Gastroenterol 6:390-394.
Citation: Ohtsuka Y, Tsuchiya S (2019) Refractory Septic Shock due to Acute Cholangitis Successfully Treated with Polymyxin B Hemoperfusion: A Case Report. J Gastrointest Dig Syst 9: 597 DOI: 10.4172/2161-069X.1000597
Copyright: © 2019 Ohtsuka Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3116
- [From(publication date): 0-2019 - Dec 21, 2024]
- Breakdown by view type
- HTML page views: 2489
- PDF downloads: 627