Research Article Open Access
Reference and Techniques used in Alveolar Bone Classification
Dutmanee Seriwatanachai1, Sirichai Kiattavorncharoen2, Nawakamon Suriyan2, Kiatanant Boonsiriseth2 and Natthamet Wongsirichat2*
1Department of Oral Biology, Faculty of Dentistry, Mahidol University, Bangkok, Thailand
2Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Mahidol University, Bangkok, Thailand
- Corresponding Author:
- Professor Natthamet Wongsirichat
Department of Oral and Maxillofacial Surgery
Faculty of Dentistry, Mahidol University
6 Yothi Street, Rajathevee, Bangkok, 10400, Thailand
Tel: +66-220078495
Fax: +66-22007844
E-mail: natthamet.won@mahidol.ac.th
Received Date: January 27, 2015; Accepted Date: March 28, 2015; Published Date: April 02, 2015
Citation: Seriwatanachai D, Kiattavorncharoen S, Suriyan N, Boonsiriseth K, Wongsirichat N (2015) Reference and Techniques used in Alveolar Bone Classification. J Interdiscipl Med Dent Sci 3:172. doi: 10.4172/2376-032X.1000172
Copyright: © 2015 Seriwatanachai D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
The marginal bone loss that usually observed around dental implant has been well documented and expected. It has related with self-reaction to the forensic body of each patient as well as the osseointegrated interface. Bone quantity and quality of the implant site may help to define the implant-bone interface, which in turn affects primary stability of the immediate implant placement. Analysis of bone quality prior to surgery provides vital information during treatment planning for dental implant. Additionally, it helps in predicting postsurgical success. The classification of bone quality, however, is difficult to follow clinically, as tactile assessments are subject to the variation among surgeons. Although imaging techniques, such as computed tomography (CT) or cone bean computed tomography (CBCT), are useful to determine bone quality, the exposure to radiation and its precision, are still of concern. This paper reviews common techniques and reference used in dental bone classification as well as the recent reports from histomorphometric analysis and molecular components. It is well acknowledged that clinical awareness of evaluating the amounts of bone surrounding the implant site by appropriate method is critical for a successful outcome.
Keywords
Alveolar ridge augmentation; Bone formation; Osteointegration; Histomorphometry; Practice guideline
Introduction
The bony structure of human jawbone is irregular in shape and size due to a non-uniform modeling during embryogenesis and early life. The mandible shows a thicker cortical and denser trabecular bone compared with the maxilla while the trabecular in posterior parts in both arch are recognized to have lower density and thickness [1-3]. The prospective clinical studies reviewed that total failure rate of implant stability is associated with bone quality surrounding the implant site [4,5]. These observations emphasize the promise of bone structural analysis in each dental implant surgery, especially in the thinner maxilla, wherein primary stability may be challenging to achieve. Despite studies in the past decades, integration of various tools used in bone type classification remained unclear. Up to now, dental technology and surgical guidelines point to a need for knowledge on bone quality and mechanical behaviour of the bone [6-8]. The stability of implant anchoring in bone crucially ensures implant success and therefore local bone quality and quantity are factors to be considered in routine assessment. The purpose of this review was to elaborate the classification system as well as techniques used in qualification of alveolar bone ridge.
Basic information about bone density in human jawbones
The position of the mandibular and maxillary teeth is commonly divergent to the position of the basal bone. The alveolar bone and basal ridge are varied from each other as more evidence has been shown in the different resorbing patterns following tooth loss [9,10]. The mandible is the largest and strongest bone of the face because of the reception of the lower teeth. It consists of a curved, horizontal portion, the body and two perpendicular portions. Using a computed tomography (CT) scan, Hounsfield unit (HU) value was collected from 4 quadrants of the mouth of over hundreds edentulous sites, both genders with age range of 18 to 89. Based on the number of HU, it has been shown that the densest region is in the anterior mandible>anterior maxilla>posterior maxilla>posterior mandible, respectively [11]. The differences of density in each zone are associated with anchorage loss and clinical situations such as anterior and posterior retraction or molar distalization. These problems brought up a number of studies in trabecular and cortical density in particular sites—i.e. incisor, canine, buccal and palatal premolar, and molar areas. Only within mandible, the buccal cortical bone at incisor demonstrated the lowest density while retromolar shows the highest density. Moreover, the rate of failure of screw implants was reported high in posterior zone of mandible. It was possibly due to excessive heat generation from the dense cortical bone within the area [12].
Using a radiographic scale to determine bone quality, the two highest density of alveolar and basal buccal cortical in maxilla were located in canine and premolar sites whereas incisor and premolar sites caught a similar range of density. Notably, the maxillary retromolar in all regions were categorized only into type III or IV by Misch’s classification, which implied that great anchorage loss could be expected in the maxillary posterior teeth. Furthermore, the density of cancellous bone in maxilla is comparable to that of the mandible (incisor, premolar, and molar) except the retromolar and canine which were reported to be of lowest density of all sites in maxilla bone [13].
Reference used in alveolar bone classification
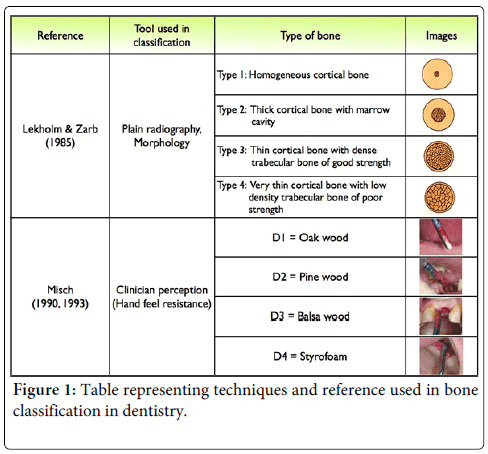
Lekholm & Zarb (1985): The oldest and most frequently used reference in bone classification system is proposed by Lekholm and Zarb (L&Z) [14], which is based on conventional radiograph and histological component [6,7,15]. The classification of each bone type is described in schematic images as presented in Table (Figure 1). There have been many studies that attempted to relate the Lekholm and Zarb classification with their parameters and techniques [16]. It is still unclear in the radiographic assessment whether Lekholm and Zarb’s study was conducted during surgery or prior to surgery. Furthermore, the overall accuracy of this classification reported a low percentage (<50%) when compared with a plain radiography with and without reference image from a trabecular bone morphology. The lowest accuracy percentage (28%) was found when the classification was applied with a sparse trabeculation of mandible [2,17]. All of mentioned above, it is plausible that trabecular volume seen in human mandible was different from L&Z schematic drawing images, suggesting that this feature may not be relevant to human jawbone which is well composed of dense/sparse trabeculations [18].
Misch (1990- 2008): Following the Misch classification, bone type was defined according to four density groups (D1–D4) in all regions of the jaws based on descriptive morphology and clinician tactile analog (Figure 2). Lately, these data were used to compare with anatomical location and radiographic scale [19].
D1 bone type represents a homogenous dense cortical, mostly found in anterior mandibles with moderate bone resorption [20]. The cortical lamellar bone in D1 type mostly contributes to the density. This induces healing with little interim woven bone formation, and ensures excellent primary stability next to the implant. In addition, the post-surgical strongest osseointegration in this type is derived from high bone-implant contact. However, the fewer blood vessels and heat generation at the apical portion of the D1 bone may cause some problems with insufficient nutritional supply and delayed bone healing. D2 is a combination of dense-to-porous cortical bone on the crest and trabecular bone from 40% to 60% on the inside, most frequently in the anterior mandible, followed by the posterior mandible. This bone type provides an excellent implant interface healing, and predictable osseointegration.Fair blood supply within the bone tissue allows bleeding during the osteotomy, which in turn is very useful in reducing overheating during surgical bed preparation. D3 is composed of thinner porous cortical bone on the crest and fine trabecular bone within the ridge. The inside portions of the trabeculae are found lesser than 50%. D3 bone is frequently found in the anterior maxilla and posterior regions of the mouth in either arch. However, the D3 anterior maxilla is usually of narrower ridge than its mandibular D3. Not only weaker than D2 bone, the bone-implant contact is also less favourable in D3 bone which cause a higher risk of implant failure. D4 bone has the least trabecular density with little or no cortical crestal bone. It is the opposite structure of D1 (dense cortical bone). The most common locations for this type of bone are the posterior region of the maxilla. It is rarely observed in mandible. The bone trabeculae may be up to 10 times weaker than the cortical bone of D1. In addition, the bone-implant contact after initial loading is often less than 25% as they are sparse bone, initial fixation of any implant design presents a surgical challenge. Implant failure after initial loading reported the highest score in this type. Moreover, it takes the longest time to integrate with the implant after placement. Bone grafting or expansion is often required for improving initial implant fixation as well as incremental loading of the implants over time was suggested to improve stability in this type.
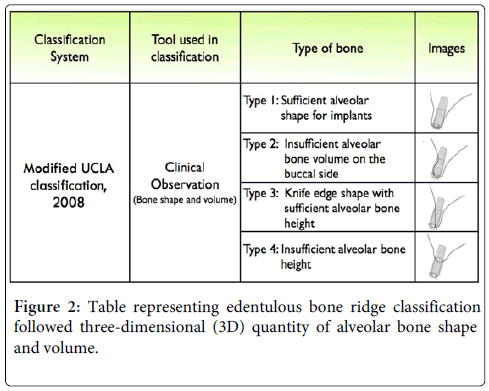
University of California Los Angeles (UCLA) classification: University of California Los Angeles (UCLA) defined a classification of edentulous alveolar bone according to bone volume and shape in three dimensions. The bone volume in the horizontal and vertical dimensions was assessed by clinician observation during the implant placement in the ideal restorative driven position. By degree of deficient ridge volume in apical, horizontal patterns, there were characterized up to 8 classes [21]. Recently, this classification was modified and regrouped into four types, as shown in Figure 2. Type I is a case with sufficient bone in horizontal and vertical dimensions, making it ideal for implant placement. Type II is a case with insufficient bone volume on the buccal side. Type III is a case with knife-shaped like alveolar bone or major deficiency bone volume on the buccal side, but with sufficient heights. Type IV is a case with insufficient alveolar heights and width with all sides of implant, are exposed. Type IV is a complete opposite of Type I in this category [21].
Integration of techniques used in bone quality measurement
The tactile assessment: The tactile assessments are the noninvasive method for evaluating bone quality. They are the most applicable, yet subjective for drilling resistance assessment. These methods are recorded during the surgery or after surgery (i.e, insertion torque, periotest). It has to be taken in early perception that the clinician experience and implant shape/structure reflecting drilling assessment in each study will be involved in the assessment and outcome. For example, insertion torques assessment, electronic devices offer a computerized programme to simultaneously read resistance torque value for evaluating bone density. To avoid bias during the test, it in genuinely suggested that a single experienced operator should carry out all instrumentations and drill set should be changed every 10 or lesser osteotomy. The insertion torques value is normally recorded every quarter turn as measured by subjective tactile perception during implant preparation. There are many possible scenarios which can occur. For instance, pre-maximum torque and the number of supra-alveolar threads are obtained before complete insertion by hand wrench. On the other hand, full insertion may be completed while the pre-maximum torque is also reached. Lastly, full insertion is completed before pre-maximum torque is reached, thus, the tapered implant may be replaced and remeasured in this scenario [19,22]. The retrospective clinical study determined a strong correlation between the insertion torques values (ISV) and implant stability quotient (ISQ), as well as the mean bone density (P<0.001) from over a hundred implants in forty-two volunteers [23]. Furthermore, the correlation between the insertion resistance values and micro CT parameters such as Trabecular number (TbN), Bone volume/Tissue volume (BV/TV), Trabecular bone Pattern factor (TbPf), was reported. In addition, the highest correlation was found between the ISV and bone density variables such as BV and BV/TV. However, ISQ and bone density either from living bone or cadaveric bone did not show any correlation [24,25].
The radiography scale, Hounsfield unit (HU)
Computerized tomography (CT) is a well-established method to evaluate bone density and providing quantitative data for trabecular and cortical bone. In dentistry, CT scan was introduced for pre-operative assessment of dental implant candidates [26]. As a result of three-dimensional anatomic image, it provides a visual set of images in the mesiodistal, buccolingual, and superioinferior dimensions together within jawbone. This technology allows clinicians determine alveolar thickness surrounding the implant bed. The surgical acrylic stents may be a useful tool to apply prior to the CT scan to set accuracy [27]. The scan produces axial images perpendicular to the long axis of the body which creates the images. Axial image has 260,000 pixels and the CT number unit, as defined by the Hounsfield unit (HU), relate to the density within the pixel. HU scale provides a quantitative assessment of bone density as measured by its ability to intensify an x-ray beam. The linear scale can be set into two points from dry air (minus 1000 HU) to pure water (0 HU). Several studies investigated bone density in a living bone or cadaver cortical bone, which showed a scale range of 1000 to 1600 [28]. One of its limitations is the ultimate scale of samples since they are mostly varied from the type of specimens, instrument model, settings, and investigator experience. Data obtained from the CT scan was used to incorporate with the Misch classification [29]. A mean difference of 180 HU at least, was required for clinical call in order to discriminate one level of radiographic density among other levels [30].
Cone beam computed tomography (CBCT) is determined by the individual volume elements or voxels and the dimensions primarily depend on the pixel size of the investigated area. The resolution of the directing area is given in submillimeter for bone quality assessment for dental implants [27,31]. The 3D cubic block of data known as “voxel” represent a degree of x-ray absorption. Voxel values obtained from CBCT images are not absolute values, like the HU values obtained from CT. CBCT generates cone-shaped beams and the images are acquired in one rotation by an image intensifier of flat panel detector [31-33]. The area of interest can be accessed from several different viewpoints as well as from three-dimensional views. During the rotation between 150 and 600 planar projection images sequential of the field of view (FOV) are acquired in a complete or partial arch. The most widely used technique in medical CBCT is maximum intensity projection (MIP) because of its simplicity and user-friendly steps. This technique provides an indication of the maximum available bucco-lingual width (axial view) which is therefore a very useful imaging for implant. CBCT is easily accessed, with proper cost to the patient, and are associated with low levels of radiation dosage. It was reported that the radiation dosages is 15 times lesser than that of conventional CT scans. The dramatically low radiation exposure is preferable to patients who have underlying disorders, as it is thought to be the most important advantage of using CBCT instead of CT. It is important to note that although computer aided implant placement is a common technique; the linear and angular deviation due to arch position can be a major concern for interpretation [33,34].
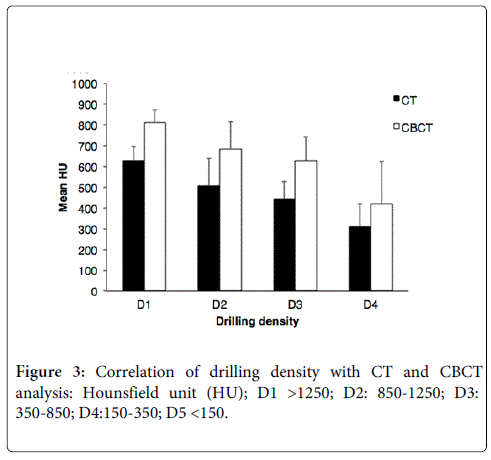
The subjective hand-felt resistance during forty-two implant surgeries were recorded for comparing with the HU value obtained from CBCT and CT. The mean HU from CBCT shows proportional higher value to those from CT. Bone densities are graded among all bone types (Figure 3). Although the mean HU density from bone Type D2 and D3 obtained from CT are a bit clearer than that from CBCT, the difficulty for distinguishing between D2 and D3 remains in both analyses. This overlap was also reported when it was associated with surgeon hand resistance assessment during bone drilling [35].
Histomorphometrical analysis
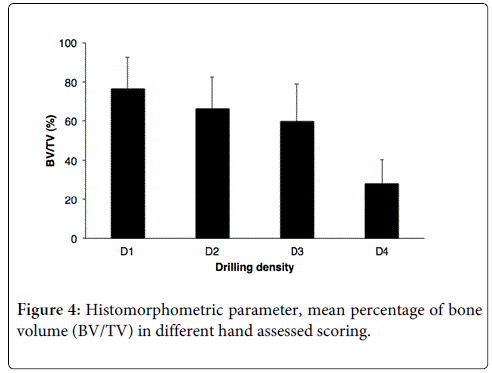
Bone histomorphometry has been inferred as a gold standard method for the evaluation of bone microarchitecture, as it allows two-dimensional analysis, inferred estimation of the spatial organisation of the trabecular net configuration measured from a set of histological sections [36]. Histomorphometric parameters were obtained using the formulas proposed by Parfitt et.al 1983 to explain bone compositions [37,38]. In accordance to the bone classification proposed by Lekholm and Zarb, Type I indicated a homogeneous cortical bone with small marrow cavity while Type III or Type IV are more heterogeneous, mostly composed of the trabeculae portion with a thin layer cortical bone. Thus, the correlations found between BS/BV, Tb.Th, Tb.Sp and the Lekholm and Zarb classification may be not be harmonized. Pereira and colleagues studied a histomorphometrical analysis correlated with the Lekholm and Zarb classification in bone biopsy from 32 implant sites. At least two fields in average were analyzed in each bone specimen. Total bone length, bone area and total tissue (soft and hard) area were measured. The results demonstrated that Type I or II were associated with lower BS/BV, higher Tb.Th, and lower Tb.Sp while Type III and IV were associated with lower Tb.Th, higher Tb.Sp, and BS/BV [39]. Nevertheless, the positive correlation between the Lekholm and Zarb classification and histomorphometric parameter was found significantly only when compared with BV/TV and Tb.Sp. It suggested that a single variable should not be solely used to define a type of bone. Another study was done in comparison among anatomical quadrants of the jawbone. The posterior maxilla was reported to be the lowest trabecular volume with thinner thickness and lower trabecular number (Tb.N) when compared with other quadrants [40]. Mean percentage of histomorphometric bone volume (BV/TV) from biopsies was used to correlate with clinical scoring based on the Misch classification, as shown in Figure 4 [35].
A large range of deviation demonstrated an overlap between Type D2 and D3 under the Misch classification. This could imply that this classification may not be practical to indicate actual bone density and may not be valid for all four types of bone. Besides the histomorphometric aspects, biological or molecular events also involve bone metabolism which may influence the bone microarchitecture. In this context, bone remodeling process occurs at discrete sites on cortical and trabecular bone surfaces, and involves sequential actions of osteoclasts and osteoblasts in normal and pathological bone [41].
Molecular parameters and immunohistochemistry
Bone multicellular unit integrating in bone remodelling mechanism is regulated by a crosstalk between osteoblasts and osteoclasts. A crucial regulating pathway involves balance of receptor activated nuclear factor ÒÂ?B (RANK), Receptor activated nuclear factor ÒÂ?B ligand (RANKL), and osteoprotegerin (OPG) [41]. These proteins as well as their mRNA expressions were used in the validation of the classification of the bone type. A recent study reported the correlation between clinical-radiographic aspects and molecular parameters of endosseous specimen obtained from implant site in healthy population. RANKL, OPG, and cathepsin K (a cysteine protease expressed in osteoclast) and osteocalcin (a noncollagenous protein mostly found in osteoblasts and odontoblasts) were measured from protein expressions to the level of gene expression in human jawbone specimen. A correlation between the histomorphometric parameters and specific cellular/molecular variables was also observed. The combination of bone relative parameters such as osteocalcin-positive osteocyte density (mm2), OPG-positive osteocyte density, OPG-positive osteoblast density, and RANKL-positive osteoblast, demonstrated statistical difference relating to the Lekholm and Zarb classification. However, none of these parameters alone could be used to distinguish the four types of bone quality [39]. It is worth to note that the Lekholm and Zarb classification of each bone type in this study were used and given by two surgical evaluations during the osteotomy, thus the possibility of inter-observations error could occur.
Conclusion and Future Prospect
Accurate and thorough measurement of the jawbone density is crucial information to support clinician decision regarding patient selection, implant shape/structure, and surgical technique used. Although many techniques commonly used to determine alveolar bone quality, based on this review, the correlation between radiographic techniques and bone type (L&Z) is the most reliable for evaluating alveolar bone type. Studies on a component of multicellar unit of bone and osteogenic genes or growth regulating factors are increasing [42-44], however, there is no single bone remodeling marker can be used for representing the quality of bone type. It suggested that further studies in molecular analyses associated with alveolar bone quality are required in this field.
Acknowledgements
The authors thank the Master of Science Programme in Implant Dentistry, Faculty of Dentistry, Mahidol University, the Thailand Research Fund (TRF); TRG5680022 and Mahidol University for the financial support given to Dutmanee Seriwatanachai.
Conflict of Interest
Authors declare no conflict of interest.
References
- Lindh C (1996) Radiography of the mandible prior to endosseousimplant treatment. Localization of the mandibular canal and assessment of trabecular bone. Swed Dent J Suppl 112: 1-45.
- Ulm C, Kneissel M, Schedle A, Solar P, Matejka M, et al. (1999) Characteristic features of trabecular bone in edentulous maxillae. Clin Oral Implants Res 10: 459-467.
- Park HS, Lee YJ, Jeong SH, Kwon TG (2008) Density of the alveolar and basal bones of the maxilla and the mandible. Am J Orthod Dentofacial Orthop 133: 30-37.
- Jaffin RA, Berman CL (1991) The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol 62: 2-4.
- Lee JY, Kim YK, Yi YJ, Choi JH (2013) Clinical evaluation of ridge augmentation using autogenous tooth bone graft material: case series study. J Korean Assoc Oral MaxillofacSurg 39: 156-160.
- Ribeiro-Rotta RF, Lindh C, Pereira AC, Rohlin M (2011) Ambiguity in bone tissue characteristics as presented in studies on dental implant planning and placement: a systematic review. Clin Oral Implants Res 22: 789-801.
- Ribeiro-Rotta RF, Lindh C, Rohlin M (2007) Efficacy of clinical methods to assess jawbone tissue prior to and during endosseous dental implant placement: a systematic literature review. Int J Oral Maxillofac Implants 22: 289-300.
- Papaspyridakos P, Chen CJ, Singh M, Weber HP, Gallucci GO (2012) Success criteria in implant dentistry: a systematic review. Journal of Dental Research 91: 242-248.
- Nevins M, Camelo M, De Paoli S, Friedland B, Schenk RK, et al. (2006) A study of the fate of the buccal wall of extraction sockets of teeth with prominent roots. Int J Periodontics Restorative Dent 26: 19-29.
- Schropp L, Wenzel A, Kostopoulos L, Karring T (2003) Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 23: 313-323.
- Shapurian T, Damoulis PD, Reiser GM, Griffin TJ, Rand WM (2006) Quantitative evaluation of bone density using the Hounsfield index. Int J Oral Maxillofac Implants 21: 290-297.
- Park GT, Morasso MI (2002) Bone morphogenetic protein-2 (BMP-2) transactivates Dlx3 through Smad1 and Smad4: alternative mode for Dlx3 induction in mouse keratinocytes. Nucleic Acids Res 30: 515-522.
- Park MC, Chung SJ, Park YB, Lee SK (2008) Bone and cartilage turnover markers, bone mineral density, and radiographic damage in men with ankylosing spondylitis. Yonsei Med J 49: 288-294.
- Lekholm U, Zarb GA (1985) Patient selection and preparation. Tissue integrated prostheses: osseointegration in clinical dentistry. Quintessence Publishing Company, Chicago, USA. 1985:199-209.
- Ribeiro-Rotta RF, Pereira AC, Oliveira GH, Freire MC, Leles CR, et al. (2010) An exploratory survey of diagnostic methods for bone quality assessment used by Brazilian dental implant specialists. J Oral Rehabil 37: 698-703.
- Norton MR, Gamble C (2001) Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res 12: 79-84.
- Bergkvist G, Koh KJ, Sahlholm S, Klintstrom E, Lindh C (2010) Bone density at implant sites and its relationship to assessment of bone quality and treatment outcome. Int J Oral Maxillofac Implants 25: 321-328.
- Lindh C, Petersson A, Rohlin M (1996) Assessment of the trabecular pattern before endosseous implant treatment: diagnostic outcome of periapical radiography in the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 82: 335-343.
- Lee S, Gantes B, Riggs M, Crigger M (2007) Bone density assessments of dental implant sites: 3. Bone quality evaluation during osteotomy and implant placement. Int J Oral Maxillofac Implants 22: 208-212.
- Misch CE, Bidez MW (1994) Implant-protected occlusion: a biomechanical rationale. Compendium 15: 1330.
- Wakimoto M, Matsumura T, Ueno T, Mizukawa N, Yanagi Y, et al. (2012) Bone quality and quantity of the anterior maxillary trabecular bone in dental implant sites. Clin Oral Implants Res 23: 1314-1319
- Johansson, Strid (1994) Assessment of bone quality from cutting resistance during implant surgery. Int J Oral Maxillofac Implants 9: 279-288.
- Turkyilmaz I, McGlumphy EA (2008) Is there a lower threshold value of bone density for early loading protocols of dental implants? J Oral Rehabil 35: 775-781.
- Ribeiro-Rotta RF, de Oliveira RC, Dias DR, Lindh C, Leles CR (2014) Bone tissue microarchitectural characteristics at dental implant sites part 2: correlation with bone classification and primary stability. Clin Oral Implants Res 25: 47-53
- Roze J, Babu S, Saffarzadeh A, Gayet-Delacroix M, Hoornaert A, et al. (2009) Correlating implant stability to bone structure. Clin Oral Implants Res 20: 1140-1145.
- Schwarz MS, Rothman SL, Rhodes ML, Chafetz N (1987) Computed tomography: Part I. Preoperative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants 2: 137-141.
- Benson BW, Shetty V (2009) Dental Implants, In: White SC, Oral Radiology Principles and Interpretation, St. Louis, MO: Mosby Publishing Inc 597-612.
- Katsumata A, Hirukawa A, Okumura S, Naitoh M, Fujishita M, Ariji E, et al. (2007) Effects of image artifacts on gray-value density in limited-volume cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104: 829-836.
- Misch CE (2008) Contemporary Implant Dentistry. 3rd ed. St. Louis, MO: Mosby Publishing Inc 135-139.
- Aranyarachkul P, Caruso J, Gantes B, Schulz E, Riggs M, Dus I, et al. (2005) Bone density assessments of dental implant sites: 2. Quantitative cone-beam computerized tomography. Int J Oral Maxillofac Implants 20: 416-424.
- Scarfe WC, Farman AG (2008) What is Cone-Beam CT and How Does it Work? Dent Clin North Am 52: 707-730
- Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K (1999) Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 28: 245-248.
- Chan HL, Misch K, Wang HL (2010) Dental imaging in implant treatment planning. Implant Dent 19: 288-298.
- Ganz SD (2008) Computer-aided design/computer-aided manufacturing applications using CT and cone beam CT scanning technology. Dent Clin North Am 52: 777-808.
- Trisi P, Rao W (1999) Bone classification: clinical-histomorphometric comparison. Clin Oral Implants Res 10: 1-7.
- Muller R, Van Campenhout H, Van Damme B, Van Der Perre G, Dequeker J, et al. (1998) Morphometric analysis of human bone biopsies: a quantitative structural comparison of histological sections and micro-computed tomography. Bone 23: 59-66.
- Parfitt AM, Drezner MK, Glorieux FH, Kanis JA, Malluche H, et al. (1987) Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 2: 595-610.
- Parfitt AM, Mathews CH, Villanueva AR, Kleerekoper M, Frame B, Rao DS (1983) Relationships between surface, volume, and thickness of iliac trabecular bone in aging and in osteoporosis. Implications for the microanatomic and cellular mechanisms of bone loss. J Clin Invest 72: 1396-409.
- Pereira AC, Souza PP, Souza JA, Silva TA, Batista AC, et al. (2013) Histomorphometrical and molecular evaluation of endosseous dental implants sites in humans: correlation with clinical and radiographic aspects. Clin Oral Implants Res 24: 414-421.
- Drage NA, Palmer RM, Blake G, Wilson R, Crane F, et al. (2007) A comparison of bone mineral density in the spine, hip and jaws of edentulous subjects. Clin Oral Implants Res 18: 496-500.
- Kearns AE, Khosla S, Kostenuik PJ (2008) Receptor activator of nuclear factor kappaB ligand and osteoprotegerin regulation of bone remodeling in health and disease. Endocrine reviews 29: 155-192.
- Wilson CG, Martin-Saavedra FM, Vilaboa N, Franceschi RT (2013) Advanced BMP gene therapies for temporal and spatial control of bone regeneration. J Dent Res 92: 409-417.
- Mason S, Tarle SA, Osibin W, Kinfu Y, Kaigler D (2014) Standardization and safety of alveolar bone derived stem cell isolation. J Dent Res 93: 55-61.
- Lin Z, Fateh A, Salem DM, Intini G (2014) Periosteum: biology and applications in craniofacial bone regeneration. J Dent Res 93: 109-116.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 29178
- [From(publication date):
April-2015 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 23538
- PDF downloads : 5640