Reduction of Foot Overpronation to Improve Iliotibial Band Syndrome in Runners: A Case Series
Received: 06-Jun-2018 / Accepted Date: 14-Jun-2018 / Published Date: 21-Jun-2018 DOI: 10.4172/2329-910X.1000272
Abstract
Introduction: Foot overpronation is commonly associated with injuries in runners, and may contribute to iliotibial band syndrome, although to date, the effect of overpronation on this injury has been little studied. The aim of this study was to assess the effect of anti-pronation orthotic insoles on pain and hip and knee kinematics in runners with overpronation and iliotibial band syndrome.
Case description: Three runners with iliotibial band syndrome underwent repeated kinematic analysis during a three-week period of training with bilateral orthotic insoles. Pain during running (visual analogue scale) and peak hip and knee internal rotation and hip adduction were analyzed.
Results: After three weeks of training with the orthotic insoles, mean pain during running decreased from 10 points on the visual analogue scale to 1.6 ± 1.5. Mean peak internal hip rotation decreased by -7.6 ± 0.3 degree (S1=-7.4 degree; S2=-7.9 degree and S3=-7.3 degree) and mean peak internal knee rotation decreased by -6.9 ± 6.4 degree (S1=-4.2 degree, S2=-14.3 degree and S3= 2.5 degree). The results for hip adduction were not consistent.
Discussion: Reduction of overpronation using orthotic insole may be an effective treatment for iliotibial band syndrome in some runners. The reduction in peak hip and knee internal rotation may have reduced strain on the iliotibial band during running, reducing pain. Kinematic analysis of running should be carried out in individuals with iliotibial band syndrome to determine the cause of the injury.
Keywords: Iliotibial band; Orthotics; Kinematics; Pronation; Running
Introduction
Iliotibial band syndrome (ITBS) is the second greatest cause of knee pain in runners, and the greatest cause of lateral knee pain [1,2]. The pain is located approximately 2 cm above the lateral joint line and is frequently described as sharp or burning [3]. The etiology of ITBS is multifactorial and highly debated [1,4], both intrinsic and extrinsic factors have been reported to be involved. Extrinsic factors include illadapted footwear, and changes in training volume such as a rapid increase in distance and hill training [3,5]. Intrinsic factors include genu varum, foot pronation, a leg length discrepancy, and muscle imbalances, which can alter the normal kinematics of the hip and knee [6–8].
Two anatomically-based models have been proposed to explain the pathophysiology of ITBS: compression and friction [4]. The iliotibial band (ITB) arises from the tensor fascia latae and gluteus maximus muscles and attaches distally to the infracondylar tubercule of the tibia and head of the fibula. The friction theory states that excessive tension is caused by anterior-posterior displacement of the ITB over the lateral femoral epicondyle, leading to inflammation and pain. The friction is reported to occur between 0 degree and 30 degree-45 degree of knee flexion, causing pain with repeated movements such as those that occur in running [9]. The compression theory states that medial-lateral excursion of the ITB compresses blood vessels, nerves and Pacinian corpuscles [9] in the epicondylar region, causing pain. Abnormal running kinematics has been associated with an increased risk of ITBS. Indeed, excessive hip and knee motion in the frontal and transverse planes could accentuate both friction and compression. However, motion in the sagittal plane does not appear to be associated with ITBS [4,10].
The biomechanics of the foot influence the alignment and function of more proximal joints [11–14], and even the whole locomotor apparatus [12,14–17]. Excessive foot pronation has been associated with running injuries and knee pain [18–21]. Foot pronation is a complex movement that occurs in the three planes of motion, combining dorsiflexion, abduction and eversion [22]. It causes internal rotation of the tibia and also the femur [11,18,23–25], leading to excessive strain at the knee [26]. Repeated internal rotation of the knee could lengthen certain structures around the knee, including the ITB [27]. Moreover, recent studies have shown that foot pronation can influence hip kinematics [13,14,28], which in turn can strain the ITB through its proximal attachment. Surprisingly, no studies have evaluated the effect of foot kinematics on ITBS. Foot pronation is generally determined using static postural tests such as the navicular drop and foot posture index. However, recent studies indicate that static analysis does not provide an indication of foot kinematics during dynamic activities such as running [29]. This may explain why the relationship between foot overpronation and knee injuries such as ITBS has been little studied.
Based on the mechanisms described above, we hypothesized that overpronation may be a cause of ITBS in some runners. The aim of this case series was therefore to carry out a dynamic assessment of the effect of anti-pronation orthotic insoles on knee pain and the kinematics of the hip and knee in runners with overpronation and ITBS, at successive time points over three weeks.
Description of cases
Three male runners with ITBS, aged between 20 and 29 years and referred to our podiatry centre for treatment of knee pain were recruited (Table 1). To be considered for the study, subjects had to run at least 15 km per week prior to the onset of the pain, have had pain over the lateral femoral epicondyle for at least one month, rated as 10 on a visual analogue scale (VAS) (i.e., maximal pain) and that caused them to stop running, and no other lower limb injuries or surgery within the previous six months [30–33]. Subjects were screened by a podiatrist and a doctor who excluded ligament, meniscus, tendon or other soft tissue lesions and diagnosed ITBS using the Ober test [34]. The final inclusion criterion was excessive foot pronation during running, assessed using plantar pressure analysis (described below). Prior to consulting our podiatry clinic, none of the runners had undergone any treatment for their knee pain.
| Characteristics | Runner 1 | Runner 2 | Runner 3 |
|---|---|---|---|
| Age (years) | 22 | 20 | 29 |
| Height (m) | 1.8 | 1.67 | 1.77 |
| Mass (kg) | 70 | 63 | 71 |
| BMI (Kg.m-2) | 21.6 | 21.9 | 22.7 |
| Running experience (years) | 3 | 2 | 5 |
| Distance per week (km) | 30 | 25 | 30 |
| Number of training sessions per week | 3 | 2 | 4 |
| BMI: Body Mass Index | |||
Table 1: Characteristics of participants.
Plantar pressure analysis was carried out on an instrumented 6-m runway (Zebris, Medical GmbH, Allgau, Germany). Potentially eligible subjects were asked to run along the runway at a minimum of 10 km/h-1 wearing their usual running shoes. All subjects included had a rear foot strike pattern during running and greater medial than lateral pressure of the foot during stance phase, demonstrating overpronation according to Brund et al. [35].
The experimental procedures were approved by the University of Rouen ethical committee and were carried out according to the Declaration of Helsinki and French legislation (Decree n° 2017-884 of May 9th, 2017).
Orthotic insoles (OI)
Customized bilateral OI were made for each runner after the first 3D gait analysis (see below). Several materials were used (Ethylene Vinyl Acetate, resin and PR sport material) and different pads were used (high-density, low elasticity) for comfort, absorption and correction. The anti-pronation wedge was shaped from the medial calcaneus to the hallux. The runners were instructed to wear the OI only when training, and to perform two training sessions of a maximum of 10 km each per week.
Evaluation
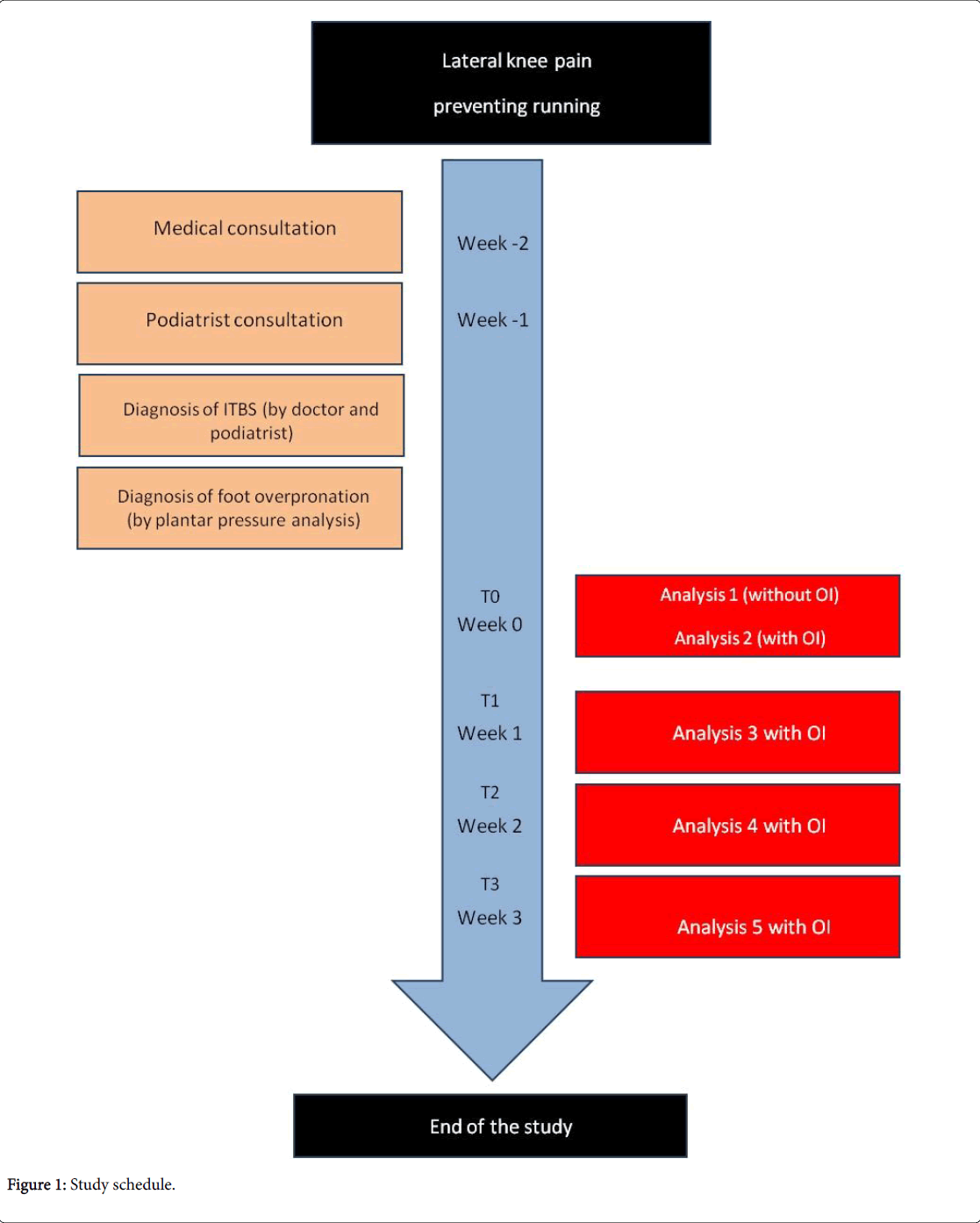
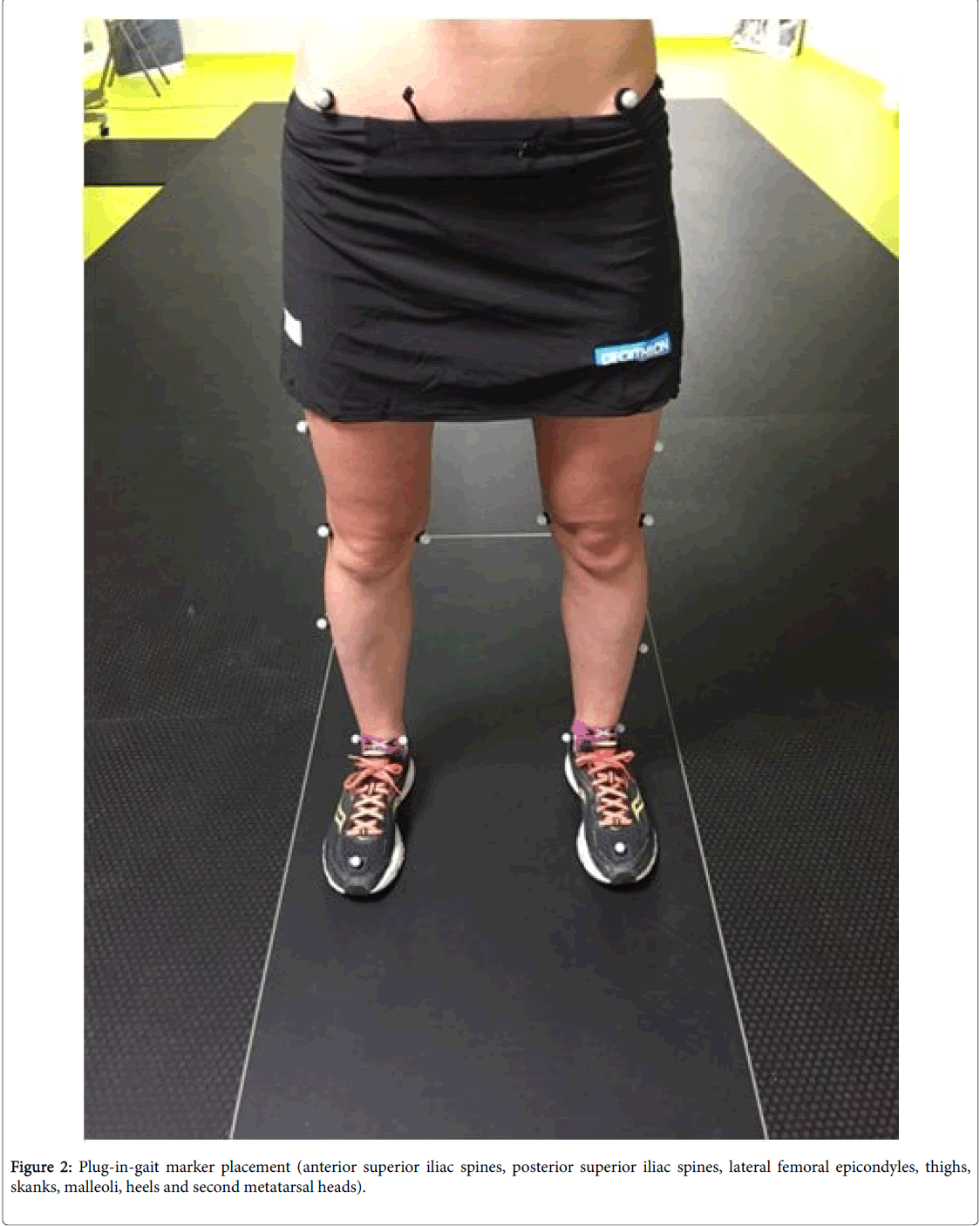
Five 3D gait analyses were carried out in our laboratory. During the first analysis, no OI were worn. The second analysis was carried out on the same day as the first, but with the OI, which were also worn for each subsequent analysis, 1, 2 and 3 weeks later. The study schedule is shown in Figure 1. The runners did not receive any other treatment or rehabilitation throughout the duration of the study. The five 3D analyses were carried out according to an identical protocol. First, each runner performed a 10-minute warm-up on a treadmill at his own chosen velocity (Care, Crosser II, Bobigny, France). This also allowed time to become familiar with the treadmill. Then, 20 passive retroreflective markers were positioned over anatomical landmarks on the lower limbs and pelvis (Figure 2), following the plug-in-gait model recommendations for use with the Vicon system (Oxford Metrics LTD, Oxford, United Kingdom). The same examiner positioned the markers on the runners at each session to limit errors and tape was used to ensure the markers remained in position if the runner sweated. Calibration was then carried out with the runner in a standing position. Subjects were asked to run for five minutes on the treadmill, which was set to a speed of 10 km/h-1, and three acquisitions, each including ten strides, were carried out during the fourth and fifth minutes using the Vicon system. Each runner wore his own running shoes, with the OI for the second to fifth analyses.
Marker trajectories were recorded at a sampling frequency of 250 Hz with a 12-camera Vicon system. Data were processed using Polygon software (Biometrics, Paris, France). The marker trajectories were filtered with a Butterworth filter at a cut-off frequency of 12 Hz as described by Loudon and Reiman [36]. Events (initial contact and toeoff) were determined from the kinematic data. Initial contact was determined as the point when the marker on the lateral malleolus changed direction from forwards to backwards. Toe-off was determined as the point when the second metatarsal marker moved from a consistent horizontal position to a more vertical position.
Pain
The runners were asked to rate the pain experienced during their own running training sessions while wearing the OI on a VAS, and to record the score on a follow up sheet after each training session.
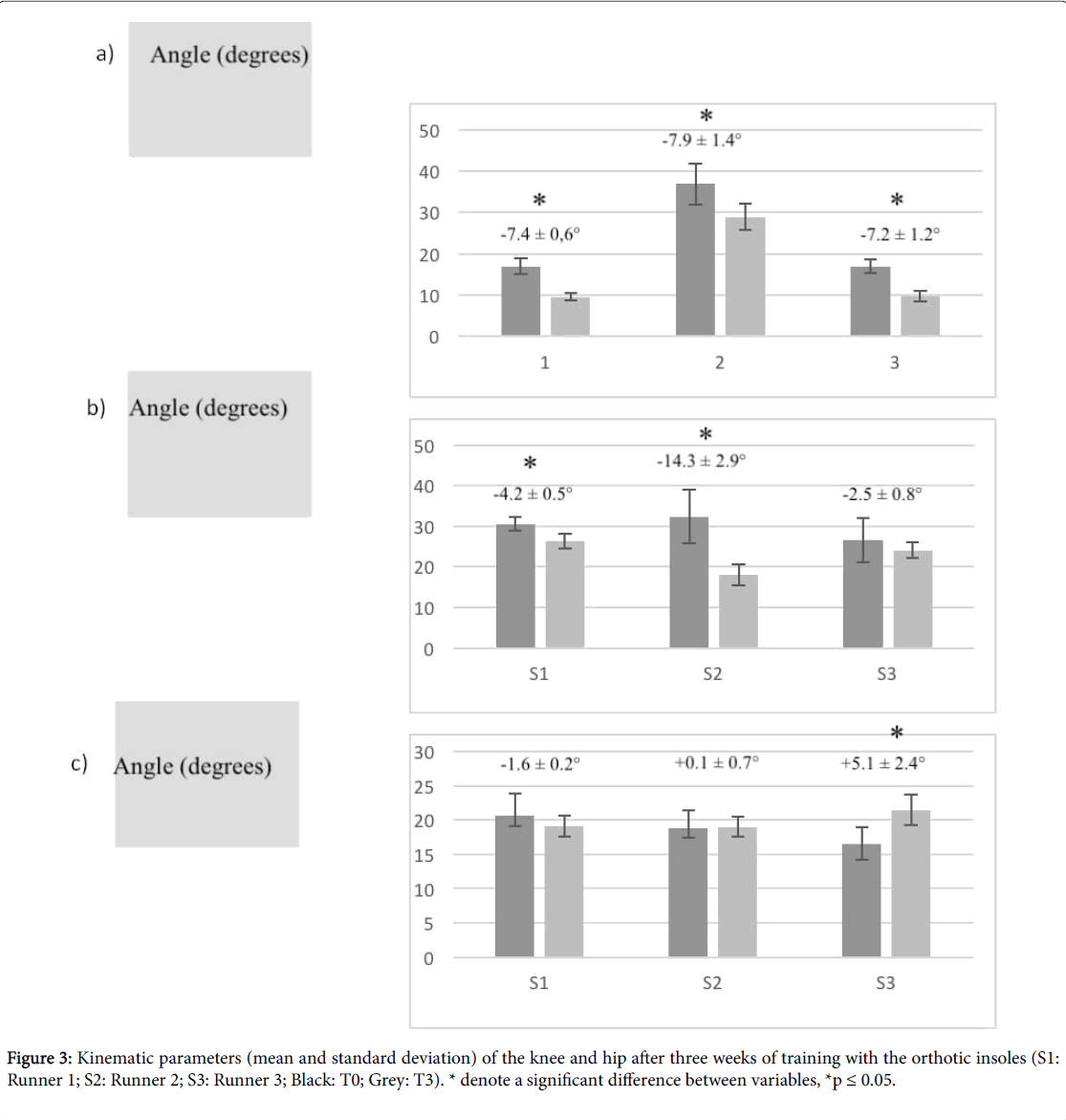
Analysed data
Peak internal hip and knee rotation and peak hip adduction were calculated for the thirty strides recorded for each runner, then the means and standard deviations were calculated for each runner (Figure 3). Statistical analysis was performed using SPPS 21.0. The data were analyzed with respect to their normality of distribution using the Shapiro-Wilk W test. Levene’s test was used to test variance homogeneity of the kinematic data. The compound symmetry or sphericity was checked with the Mauchly’s test. A repeated measure of ANOVA was used to determine difference between each analysis. Statistical significance was assumed with p ≤ 0.05.
Results
After 3 weeks of training with the OI, the pain rating decreased considerably for all three runners (Table 2): mean rating of 10 ± 0 before the OI and of 1.6 ± 1.5 (EVA reduction: S1: -10; S2: -8; S3: -7) after three weeks of training with the OI.
| Pain (score on VAS) | S1 | S2 | S3 |
|---|---|---|---|
| T0 | 10 | 10 | 10 |
| T3 | 0 (-10) | 2 (-8) | 3 (-7) |
| VAS: Visual Analogue Scale | |||
Table 2: Pain after 3 weeks of wearing the orthotic insoles.
The results for the kinematic analysis are reported for weeks 0 and 3 because no real change occurred between T0 and T1 or T0 and T2. There was a decrease in peak internal rotation of both the knee and the hip in the injured limb between the first and final analyses (Figure 3). Peak internal knee rotation reduced significantly by -7.4 ± 0.6 degree, -7.9 ± 1.4 and -7.2 ± 1.2 degree and peak internal hip rotation reduced significantly for the runner 1 and 2 by -4.2 ± 0.5 degree, -14.3 ± 2.9 degree and -2.5 ± 0.8 degree for the runner 3. The results for hip adduction were less consistent with a decrease of -1.6 ± 0.2 degree in runner 1, a significantly increase of +5.1 ± 2.4 degree in runner 3 and no change for runner 2 (+0.1 ± 0.7 degree).
Discussion
The aim of this study was to examine the effects of wearing OI on knee pain and hip and knee kinematics in runners with ITBS. This small case series provides preliminary findings for certain kinematic factors that may influence ITBS. After three weeks of training with the OI, pain during running reduced considerably in all three runners (EVA reduction: S1: -10; S2: -8; S3: -7), as did peak hip (S1=-4.2 ± 0.5 degree; S2=-14.3 ± 2.9 degree; S3=-2.5 ± 0.8 degree) and knee internal rotation (S1=-7.4 ± 0.6 degree; S2=-7.9 ± 1.4 degree; S3=-7.2 ± 1.2 degree) on the painful side. Changes in peak hip adduction were less consistent (S1=of -1.6 ± 0.2 degree; S2=+0.1 ± 0.7 degree; S3=+5.1 ± 2.4 degree).
Many biomechanical studies have shown that kinematic parameters of the hip, knee and foot are abnormal in ITBS, although the specific kinematic anomalies related to ITBS remain debated, in particular those relating to the hip. Some studies have found peak hip adduction to be increased during stance in ITBS [37,38] while others have found it to be decreased [33,39,40] or normal [41]. Similarly, external hip rotation has been shown to be increased in some studies [33,38], while others have found an increase in internal hip rotation[32]. Results appear more consistent regarding internal knee rotation, which seems to be commonly increased in ITBS [37,38,40]. Several studies have shown that foot eversion is reduced in ITBS [40,38]. In contrast with these previous studies, a study on the effect of gender on kinematics in ITBS found no differences in hip and knee kinematics between males with ITBS and a male control group [33]. These contrasting results may be due to differences in the methodologies used in each study such as differences in the samples included, barefoot running or shod running, treadmill or overground running etc.
Since internal rotation of the tibia appears to be associated with ITBS [37,38] and overpronation of the foot is associated with internal rotation of the tibia [17], which represent a biomechanical fact. We hypothesized that OI to reduce overpronation would reduce internal knee rotation and pain. The results of our study confirmed this hypothesis, demonstrated by the concomitant significant decrease in both these parameters with use of the OI, as has been found elsewhere [42–44]. Moreover, internal hip rotation has been shown to be increased by overpronation [14,28] and associated with ITBS [32]. The kinematic analysis showed that after three weeks of training with OI, peak internal hip rotation was reduced in all three runners and significantly reduced for two of them. These results suggest that increased internal hip rotation in stance may contribute to ITBS and reducing this rotation may decrease strain on the ITB. Thus, the anterior-posterior (or medio-lateral) move of the ITB across the knee is reduce and decrease the mechanical causes of the pain.
Noehren et al. [38], reported that an only a few degrees of hip adduction might be sufficient to strain the ITB, inducing inflammation by friction and/or compression [4]. However, as stated above, the role of hip adduction in ITBS is controversial. This is reflected in our results, which were inconsistent for this parameter. Although obviously no conclusions can be drawn from our small case series, it is interesting to note that in the runner with the largest improvement in pain (Runner 1) peak hip adduction decreased, while in the runner with the smallest improvement in pain (Runner 3) it increased significantly. This suggests that hip adduction should be considered in the evaluation and treatment of ITBS.
The ITB has attachments on the femur and the gluteus maximus and tensor fasciae latae muscles [4] as well as on the lumbar spine, ilium and sacrum [45,46]. Power [27] showed that trunk motion in the frontal and transverse planes may contribute to abnormal hip and knee kinematics, and could lead to strain of the structures of the knee, in particular the ITB. Baker et al. [4], discussed the fact that genu valgus (often caused by foot over pronation) causes internal hip rotation, which could strain the collateral ligament [27] or the ITB, which control internal knee rotation [6,47–49]. Over time, this could lead to a lengthening of the ITB. When treating ITBS, the first aim is to reduce any lengthening effect on the ITB [3]. This could explain why the antipronation OI reduced knee pain over a period of three weeks.
This study has several strengths and limitations. Firstly, although the sample was very small, the runners included were homogenous in that they all had foot over pronation. Moreover, in contrast with most studies, the over pronation was verified using a dynamic test. It would have been interesting to carry out a longitudinal evaluation of foot kinematics, including pronation, however this was not possible because of a limitation of the current plug-in gait software that does not evaluate pronation sufficiently accurately. Furthermore, the marker set used for the plug-in gait software is relatively sparse, which could potentially accentuate motion artifacts and decrease the accuracy of the results. However, attempts were made to reduce errors by having the same evaluator position all the markers on each runner. Also, the results for hip and knee rotation were consistent, with small withinsubject standard errors, suggesting that they were not particularly influenced by artifacts. Finally, the running shoes worn by the subjects were not controlled. Different running shoes and their state of wear them could influence lower limb kinematics.
Conclusion
The results of this case series suggest that correcting over pronation of the foot by wearing OI may be an effective treatment for ITBS in runners who over pronate. Pain reduced considerably and consistently in all three runners. Moreover, correction of the pronation reduced significantly peak internal hip rotation for two runners and peak internal knee rotation for all runners. Thus, the anti pronation orthotics insoles modify the biomechanics of the locomotor apparatus including reduction of the peak internal rotation of the hip and knee. These modifications could reduce the friction and the compression of the iliotibial band in the knee, decreasing the mechanical cause of the pain. These results suggest excessive internal knee and hip rotation, caused by over pronation of the foot could contribute to ITBS. We suggest that a biomechanical analysis of the lower limb, including the foot, should be systematically carried out in individuals with ITBS to determine the cause of the injury.
Further, longitudinal studies are necessary to confirm these preliminary results and to evaluate if additional kinematic changes occur over the longer term.
Conflict of interest
We certify that all authors have no affiliation with financial involvement in any organization or entity with a direct financial interest in the subject matter or materials discussed in the manuscript.
Acknowledgement
Authors express their thanks to the "Institut de Recherche Interdisciplinaire Homme Société" for their contribution for the translation of this study.
References
- Van der Worp MP, Van der Horst N, de Wijer A, Backx FJ, Nijhuis-Van der Sanden MW (2012) Iliotibial band syndrome in runners: A systematic review. Sports Med 42: 969–992.
- Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, et al. (2002) A retrospective case-control analysis of 2002 running injuries. Br J Sports Med 36: 95–101.
- Fredericson M, Weir A (2006) Practical management of iliotibial band friction syndrome in runners. Clin J Sport Med 16: 261–268.
- Baker RL, Fredericson M (2016) Iliotibial band syndrome in runners: Biomechanical implications and exercise interventions. Phys Med Rehabil Clin N Am 27: 53–77.
- Van Gent RN, Siem D, Van Middelkoop M, Van Os AG, Bierma-Zeinstra SMA, et al. (2007) Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br J Sports Med 41: 469–480.
- Baker RL, Souza RB, Fredericson M (2011) Iliotibial band syndrome: Soft tissue and biomechanical factors in evaluation and treatment. PMR 3: 550–561.
- Fredericson M, Cookingham CL, Chaudhari AM, Dowdell BC, Oestreicher N, et al. (2000) Hip abductor weakness in distance runners with iliotibial band syndrome. Clin J Sport Med 10: 169–175.
- Golightly YM, Allen KD, Helmick CG, Renner JB, Jordan JM (2009) Symptoms of the knee and hip in individuals with and without limb length inequality. Osteoarthritis Cartilage 17: 596–600.
- Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, et al. (2007) Is iliotibial band syndrome really a friction syndrome? J Sci Med Sport 10: 74–76.
- Orchard JW, Fricker PA, Abud AT, Mason BR (1996) Biomechanics of iliotibial band friction syndrome in runners. Am J Sports Med 24: 375–379.
- Dugan SA, Bhat KP (2005) Biomechanics and analysis of running gait. Phys Med Rehabil Clin N Am 16: 603–621.
- Khamis S, Yizhar Z (2007) Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 25: 127–134.
- Lack S, Barton C, Malliaras P, Twycross-Lewis R, Woledge R, et al. (2014) The effect of anti-pronation foot orthoses on hip and knee kinematics and muscle activity during a functional step-up task in healthy individuals: A laboratory study. Clin Biomech 29: 177–182.
- Resende RA, Deluzio KJ, Kirkwood RN, Hassan EA, Fonseca ST (2015) Increased unilateral foot pronation affects lower limbs and pelvic biomechanics during walking. Gait Posture 41: 395–401.
- Fischer KM, Willwacher S, Hamill J, Brüggemann GP (2017) Tibial rotation in running: does rearfoot adduction matter? Gait Posture 51: 188–193.
- Khamis S, Dar G, Peretz C, Yizhar Z (2015) The relationship between foot and pelvic alignment while standing. J Hum Kinet 46: 85–97.
- Pinto RZA, Souza TR, Trede RG, Kirkwood RN, Figueiredo EM, et al. (2008) Bilateral and unilateral increases in calcaneal eversion affect pelvic alignment in standing position. Man Ther 13: 513–519.
- Hintermann B, Nigg BM (1998) Pronation in runners: Implications for injuries. Sports Med Auckl NZ 26: 169–176.
- Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR (1999) The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med 27: 585–593.
- Van Boerum DH, Sangeorzan BJ (2003) Biomechanics and pathophysiology of flat foot. Foot Ankle Clin 8: 419–430.
- Zhang X, Aeles J, Vanwanseele B (2017) Comparison of foot muscle morphology and foot kinematics between recreational runners with normal feet and with asymptomatic over-pronated feet. Gait Posture 54: 290–294.
- Horwood AM, Chockalingam N (2017) Defining excessive, over, or hyper-pronation: A quandary. The Foot 31: 49–55.
- Coplan JA (1989) Rotational motion of the knee: A comparison of normal and pronating subjects. J Orthop Sports Phys Ther 10: 366–369.
- DeLeo AT, Dierks TA, Ferber R, Davis IS (2004) Lower extremity joint coupling during running: a current update. Clin Biomech 19: 983–991.
- Eng JJ, Pierrynowski MR (1993) Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome. Phys Ther 73: 62–68.
- McClay I, Manal K (1998) A comparison of three-dimensional lower extremity kinematics during running between excessive pronators and normals. Clin Biomech Bristol Avon 13: 195–203.
- Powers CM (2010) The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther 40: 42–51.
- Souza TR, Pinto RZ, Trede RG, Kirkwood RN, Pertence AE, et al. (2009) Late rear foot eversion and lower-limb internal rotation caused by changes in the interaction between forefoot and support surface. J Am Podiatr Med Assoc 99: 503–511.
- Langley B, Cramp M, Morrison SC (2015) Selected static foot assessments do not predict medial longitudinal arch motion during running. J Foot Ankle Res 8: 56.
- Brown AM, Zifchock RA, Hillstrom HJ, Song J, Tucker CA (2016) The effects of fatigue on lower extremity kinematics, kinetics and joint coupling in symptomatic female runners with iliotibial band syndrome. Clin Biomech Bristol Avon 39: 84–90.
- Davis IS, Bowser BJ, Mullineaux DR (2016) Greater vertical impact loading in female runners with medically diagnosed injuries: A prospective investigation. Br J Sports Med 50: 887–892.
- Noehren B, Schmitz A, Hempel R, Westlake C, Black W (2014) Assessment of strength, flexibility, and running mechanics in men with iliotibial band syndrome. J Orthop Sports Phys Ther 44: 217–222.
- Phinyomark A, Osis S, Hettinga BA, Leigh R, Ferber R (2015) Gender differences in gait kinematics in runners with iliotibial band syndrome. Scand J Med Sci Sports 25: 744–753.
- Gose JC, Schweizer P (1989) Iliotibial band tightness. J Orthop Sports Phys Ther 10: 399–407.
- Brund RBK, Rasmussen S, Nielsen RO, Kersting UG, Laessoe U, et al. (2017) Medial shoe-ground pressure and specific running injuries: a 1-year prospective cohort study. J Sci Med Sport 20: 830–834.
- Loudon JK, Reiman MP (2012) Lower extremity kinematics in running athletes with and without a history of medial shin pain. Int J Sports Phys Ther 7: 356–364.
- Ferber R, Noehren B, Hamill J, Davis IS (2010) Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther 40: 52–58.
- Noehren B, Davis I, Hamill J (2007) ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech Bristol Avon 22: 951–956.
- Foch E, Milner CE (2014) The influence of iliotibial band syndrome history on running biomechanics examined via principal components analysis. J Biomech 47: 81–86.
- Grau S, Maiwald C, Krauss I, Axmann D, Horstmann T (2008) The influence of matching populations on kinematic and kinetic variables in runners with iliotibial band syndrome. Res Q Exerc Sport 79: 450–457.
- Miller RH, Lowry JL, Meardon SA, Gillette JC (2007) Lower extremity mechanics of iliotibial band syndrome during an exhaustive run. Gait Posture 26: 407–413.
- Cornwall MW, McPoil TG (1995) Footwear and foot orthotic effectiveness research: A new approach. J Orthop Sports Phys Ther 21: 337–344.
- MacLean C, Davis IM, Hamill J (2006) Influence of a custom foot orthotic intervention on lower extremity dynamics in healthy runners. Clin Biomech 21: 623–630.
- Nawoczenski DA, Cook TM, Saltzman CL (1995) The effect of foot orthotics on three-dimensional kinematics of the leg and rearfoot during running. J Orthop Sports Phys Ther 21: 317–327.
- Kaplan EB (1958) The iliotibial tract: Clinical and morphological significance. J Bone Joint Surg Am 40: 817–832.
- Stern JT (1972) Anatomical and functional specializations of the human gluteus maximus. Am J Phys Anthropol 36: 315–339.
- Lutz C, Sonnery CB, Niglis L, Freychet B, Clavert P, et al. (2015) Anatomie descriptive des structures antéro-latérales mises en tension au cours de la rotation interne du genou. Rev Chir Orthopédique Traumatol 101:333–339.
- Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43: 669–674.
- Vieira EL, Vieira EA, da Silva RT, Berlfein PA, Abdalla RJ, et al. (2007) An anatomic study of the iliotibial tract. Arthroscopy 23: 269–274.
Citation: Dodelin D, Tourny C, Menez C, Coquart J, L’Hermette M (2018) Reduction of Foot Overpronation to Improve Iliotibial Band Syndrome in Runners: A Case Series. Clin Res Foot Ankle 6: 272. DOI: 10.4172/2329-910X.1000272
Copyright: © 2018 Dodelin D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14695
- [From(publication date): 0-2018 - Jan 26, 2025]
- Breakdown by view type
- HTML page views: 13856
- PDF downloads: 839