Case Report Open Access
Recurrent Psoas Abscess associated with Retrocecal Appendicitis in an Adolescent Female
Hsun-Chin Chao1*, Yung-Ching Ming2 and Chih-Cheng Luo31Division of Pediatric Gastroenterology, Department of Pediatrics, Chang Gung Children√ʬ?¬?s Medical Center, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, 5 Fu-Hsin Street, Gueishan District, 33305, Taoyuan City, Taiwan
2Divison of Pediatric Surgery, Department of Pediatrics, Chang Gung Children√ʬ?¬?s Medical Center, Chang Gung Memorial Hospital, Chang Gung University College of Medicine, 5 Fu-Hsin Street, Gueishan District, 33305, Taoyuan City, Taiwan
3Division of Pediatric Surgery, Department of Surgery, Wan Fang Hospital, Taipei Medical University, Taipei City, Taiwan
- *Corresponding Author:
- Hsun-Chin Chao
Associate Professor
Division of Pediatric Gastroenterology
Department of Pediatrics
Chang Gung Children√ʬ?¬?s Medical Center
Chang Gung Memorial Hospital
Chang Gung University College of Medicine
5 Fu-Hsin Street, Gueishan District
33305, Taoyuan City, Taiwan
Fax: 886-3-3288957
E-mail: chahero@yahoo.com
Received: November 18, 2015; Accepted: December 01, 2015; Published: December 07, 2015
Citation: Chao HC, Ming YC, Luo CC (2015) Recurrent Psoas Abscess associated with Retrocecal Appendicitis in an Adolescent Female. Neonat Pediatr Med 1: 101. doi:10.4172/2572-4983.1000101
Copyright: © 2015 Chao HC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
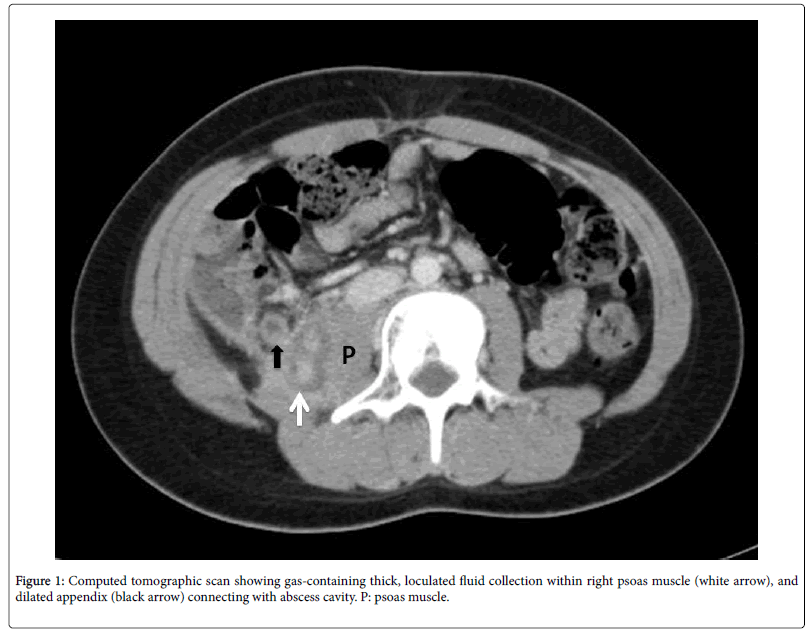
Psoas abscess (PA) is encountered infrequently in children. Pyogenic psoas abscess is most commonly a primary process associated with Staphylococcus aureus in children. Herein we present a female adolescent of secondary psoas abscess associated with ruptured retrocecal appendicitis, and it was successfully treated by broadspectrum antibiotics and prompt surgical intervention. The patient was a case of ruptured appendicitis with successful conservative treatment. The patient missed the follow-up schedule for elective interval appendectomy. Two years later, she presented with fever, limping gait, and right flank pain. Ultrasound revealed fixed dilated bowel loops, a fecalith and a heterogeneous hypoechoic lesion (3.7×3.6×3.3 cm) at right psoas muscle, suspecting PA. The patient received intravenous antibiotics for 2 weeks and made an excellent recovery. A follow-up ultrasound showed complete resolution of the abscess. The patient missed the schedule for interval appendectomy again, and same symptoms recurred 4 months later. Laboratory data indicated leukocytosis and marked elevation of serum Creactive protein. Computed tomography scan of the abdomen showed a gas-containing fluid collection within the right psoas muscle, and connecting with a dilated appendix. Laparotomy with appendectomy and tube drainage of the abscess was done, and the patient had uneventful recovery. The bacterial culture of pus grew Enterobacter cloacae. The patient discharged eight days after surgery. Neither abdominal symptoms nor evidence of recurrent PA on follow-up ultrasound was observed in the later years.
Keywords
Psoas abscess; Retrocecal appendicitis; Complication; Children
Abbreviations
PA: psoas abscess
Introduction
Pyogenic psoas abscess (PA) is rare in childhood. PA is caused by primary hematogenous spread or secondary adjacent infectious sources. 75% of psoas abscesses in adults have been reported to originate from secondary causes [1]; Crohn’s disease is the most common cause of secondary PA, other conditions implicated are diverticulitis, appendicitis, osteomyelitis of adjacent ribs or vertebrae, colonic carcinoma and pancreatitis [2-8]. In contrast with the adult population, primary PA accounts for the vast majority of pediatric cases, with Staphylococcus aureus the pathogen most frequently isolated [9-12]. Secondary PA is unusual in children, but surprisingly, acute appendicitis, although among the most common surgical emergencies in children, has rarely been discussed with such unusual presentation, especially in the pediatric age group.
We report a case of secondary PA after ruptured retrocecal appendicitis in a child and discuss the diagnosis and treatment of this disorder. Our case had been treated with antibiotics alone and made an eventful recovery. Surgical drainage of psoas abscess was required in our patient because of its frequent recurrences.
Case Presentation
A 13 year-old girl is a patient who had been admitted and treated successfully by non-operative management with antibiotics for suspecting perforated appendicitis with intraabdominal abscess three years ago. The patient complained of abdominal pain at right lower quadrant (RLQ) of abdomen for 4 days and fever for 3 days. Physical examination indicated tenderness and rebounding pain at RLQ of the abdomen. Abdominal radiography demonstrated a fecalith and small bowel dilatation. Ultrasound revealed fixed dilated bowel loops, a fecalith and a heterogenous hypoechoic lesion (4.6 ×3.5×3.3 cm) in RLQ of the abdomen, suspecting ruptured appendicitis with retroperitoneal abscess. The patient received intravenous broadspectrum antibiotics (cefamezine and gentamycin and metronidazole) for 2 weeks during hospitalization. She had been free of abdominal symptoms since the second week of admission and had uneventful course on the following month. Elective interval appendectomy was scheduled, but the patient missed the follow-up schedule. Two years later, she presented with fever, limping gait, and right flank pain for 3 days. An abdominal ultrasound showed a heterogenous hypoechoic lesion (3.7×3.6×3.3 cm) at right psoas muscle, suspecting PA. Previous appendicitis-related PA formation was highly suspected. The patient’s parents refuse to do laparotomy surgery for possible post-operative complications, while accepted the future interval laparoscopic surgery for appendectomy. She was treated with intravenous antibiotics (ceftriaxone and metronidazole) for 2 weeks and made an excellent recovery. She continued to receive antibiotics with oral augmentin and clindamycin for one week after she was discharged, and a follow-up abdominal ultrasound showed complete resolution of the abscess. The patient was arranged laparoscopic surgery for interval appendectomy in the next month.
She had missed the surgical schedule again due to an episode of upper respiratory infection. Unfortunately, 4 months later, she was readmitted with a 2-day history of fever, limping gait and pain in the right groin. Laboratory data showed leukocytosis with a white blood cell count of 13,800/mm3 (82% neutrophils), and elevated C-reactive protein level, 175.2 mg/dL. Computed tomography (CT) scan of the abdomen showed a gas-containing fluid collection within the right psoas muscle, and connecting with a suspecting dilated appendix (Figure 1). Frequent complicated recurrence and percutaneous CTguided drainage is improper because of multi-loculated cavity with thick pus revealing by CT scan. The patient was transferred to our pediatric surgical department for further management. Laparoscopic surgical drainage of the psoas abscess was performed on the second day of admission by transperitoneal approach. Conversion to open laparotomy during operation was made because of a fragmented appendix where the appendiceal base and psoas abscess cavity could not be identified well and a dense inflammatory mass which seemed to be creating a pseudotumor around the cecum and psoas muscle. Appendectomy with tube drainage of the abscess cavity was done, and the patient had uneventful recovery. The psoas fascia was incised, and the muscle was split open. About 3 ml of pus with turbid granulation tissue was drained and scooped from the cavity and sent for culture sensitivity and pathologic examination. The cavity was irrigated and drained. Appendectomy with tube drainage of the abscess cavity was performed. The fever subsided 2 days after surgery. The postoperative course was uneventful. The bacterial culture of pus grew Enterobacter cloacae . Pathology of the granulation tissue showed marked acute and chronic inflammation, and the transected appendix showed fibrosis of the appendiceal wall and serosa.
The drain was removed on the seventh postoperative day, and the child was discharged eight days after surgery in general good condition. Follow-up ultrasound in the later months showed complete resolution of the abscess. She is presently doing well without any abdominal symptoms during a 2-year follow-up.
Discussion
PA is rare and presents a diagnostic challenge with a high index of suspicion [13]. The characteristic triad of limp, fever, and pain described by Mynter in 1881 remains the commonest clinical presentation in childhood [13].
PA formation as a consequence of retrocecal appendicitis in children has been rarely described and it remains one of the most serious but unusual complications of acute appendicitis [14]. The formation of retroperitoneal abscesses involving psoas muscle have been reported mostly in adult patients [15-18].
Retrocecal appendix can be either retroperitoneal or intraperitoneal in position. It is its extraperitoneal position that results in direct contamination of the psoas muscle following inflammation [19]. Retrocecal appendicitis is the commonest location of normal appendix, isolated retroperitoneal abscess formation has commonly been reported in cases with perforated retrocecal appendicitis [20]. The etiopathogenesis of this unusual presentation in our case can be explained by the direct invasion of the right psoas muscle by a perforated retrocecal appendix.
There is no consensus regarding the optimal treatment for children with perforated appendicitis. Much heterogeneity exists among pediatric surgeons regarding choice of antibiotics, duration of treatment, route of administration, and duration of hospitalization. The major goal of non-operative therapy is to limit the inflammatory response and sepsis in these patients [21,22]. Initial non-operative management with antibiotics and /or abscess drainage for some children presenting with perforated appendicitis with abscess has been shown to be safe and effective in these situations [23,24]. Interval appendectomy has been offered because of the perceived risk of recurrent appendicitis. In our institute an elective laparoscopic appendectomy has been a standard practice to carry after 8-12 weeks following conservative treatment of a ruptured appendicitis with abscess. Although the need for further interval appendectomy in children with perforated appendicitis who has been successfully managed non-operatively is controversial [25,26]. Some studies report recurrence rates after non-operative management of appendicitis ranging from 6% to 43%, and all recurrence occurred within 3 years of initial diagnosis with 80% recurrence occurring within 6 months of the initial episode of acute appendicitis [23,24].
Traditionally, psoas abscess has been treated by extraperitoneal operative drainage. A combined treatment of ultrasound or CT-guided percutaneous drainage and systemic antibiotics for psoas abscess has been successfully recently and has become the preferred method for treatment [27]. PA that is smaller than 3 cm in greatest diameter may be managed successfully with antibiotics alone [27]. A percutaneous drainage is improper to manage the psoas abscess in our patient because of its multi-loculated cavity with thick pus revealing by CT scan. Only one report showed that a psoas abscess was effectively drained laparoscopically through an extraperitoneal approach [28].
In conclusion, ruptured retrocecal appendicitis must be considered in pediatric case of secondary PA. Abdominal ultrasound and CT scan are the preferred diagnostic tools for PA. Surgical drainage with antibiotics is mandatory to decrease complicated recurrence of secondary PA caused by ruptured retrocecal appendicitis. Interval appendectomy is recommended after initial non-operative management of complicated appendicitis to prevent the formation of secondary PA.
Acknowledgements
We thank the children and their parents for their participation in the study, and we thank the study interviewers for their diligent efforts.
References
- Baier PK, Arampatzis G, Imdahl A, Hopt UT (2006) The iliopsoas abscess: Aetiology, therapy and outcome. Langenbecks Arch Surg 391: 411-417.
- Bartolo DC, Ebbs SR, Cooper MJ (1987) Psoas abscess in Bristol: A 10-year review. Int J Colorectal Dis 2: 72-76.
- Leu SY, Leonard MB, Beart RW Jr, Dozois RR (1986) Psoas abscess: Changing patterns of diagnosis and etiology. Dis Colon Rectum 29: 694-698.
- Procaccino JA, Lavery IC, Fazio VW, Oakley JR (1991) Psoas abscess: difficulties encountered. Dis Colon Rectum 34: 784-789.
- Taiwo B (2001) Psoas abscess: A primer for the internist. South Med J 94: 2-5.
- Zissin R, Gayer G, Kots E, Werner M, Shapiro-Feinberg M, et al. (2001) Iliopsoas abscess: A report of 24 patients diagnosed by CT. Abdom Imaging 26: 533-539.
- Walsh TR, Reilly JR, Hanley E, Webster M, Peitzman A, et al. (1992) Changing etiology of iliopsoas abscess. Am J Surg 163: 413-416.
- Ricci MA, Meyer KK (1985) Psoas abscess complicating Crohn's disease. Am J Gastroenterol 80: 970-977.
- Bresee JS, Edwards MS (1990) Psoas abscess in children. Pediatr Infect Dis J 9: 201-206.
- Kang M, Gupta S, Gulati M, Suri S (1998) Ilio-psoas abscess in the paediatric population: Treatment by US-guided percutaneous drainage. Pediatr Radiol 28: 478-481.
- Kleiner O, Cohen Z, Barki Y, Mares AJ (2001) Unusual presentation of psoas abscess in a child. J Pediatr Surg 36: 1859-1860.
- Katara AN, Shah RS, Bhandarkar DS, Unadkat RJ (2004) Retroperitoneoscopic drainage of a psoas abscess. J Pediatr Surg 39: e4-5.
- Mynter H (1881) Acute psoasitis. Buffalo Med Surg J 21: 202.
- Sharma SB, Gupta V, Sharma SC (2005) Acute appendicitis presenting as thigh abscess in a child: A case report. Pediatr Surg Int 21: 298-300.
- El-Masry NS, Theodorou NA (2002) Retroperitoneal perforation of the appendix presenting as right thigh abscess. Int Surg 87: 61-64.
- Hsieh CH, Wang YC, Yang HR, Chung PK, Jeng LB et al. (2006) Extensive retroperitoneal and right thigh abscess in a patient with ruptured retrocecal appendicitis: an extremely fulminant form of a common disease. World J Gastroenterol 12: 496-499.
- Kao CT, Tsai JD, Lee HC, Wang NL, Shih SL, et al. (2002) Right perinephric abscess: a rare presentation of ruptured retrocecal appendicitis. Pediatr Nephrol 17: 177-180.
- McGahan JP (1982) Perinephric abscess secondary to ruptured retrocecal appendix diagnosed by computerized tomography. Urology 19: 217-219.
- Tomasoa NB, Ultee JM, Vrouenraets BC (2008) Retroperitoneal abscess and extensive subcutaneous emphysema in perforated appendicitis: a case report. Acta Chir Belg 108: 457-459.
- Hsieh CH, Wang YC, Yang HR, Chung PK, Jeng LB, et al. (2007) Retroperitoneal abscess resulting from perforated acute appendicitis: Analysis of its management and outcome. Surg Today 37: 762-767.
- Oliak D, Yamini D, Udani VM, Lewis RJ, Arnell T, et al. (2001) Initial nonoperative management for periappendiceal abscess. Dis Colon Rectum 44: 936-941.
- Brown CV, Abrishami M, Muller M, Velmahos GC (2003) Appendiceal abscess: Immediate operation or percutaneous drainage? Am Surg 69: 829-832.
- Gillick J, Velayudham M, Puri P (2001) Conservative management of appendix mass in children. Br J Surg 88: 1539-1542.
- Janik JS, Ein SH, Shandling B, Simpson JS, Stephens CA (1980) Nonsurgical management of appendiceal mass in late presenting children. J Pediatr Surg 15: 574-576.
- Puapong D, Lee SL, Haigh PI, Kaminski A, Liu IL, et al. (2007) Routine interval appendectomy in children is not indicated. J PediatrSurg 42: 1500-1503.
- Friedell ML, Perez-Izquierdo M (2000) Is there a role for interval appendectomy in the management of acute appendicitis? Am Surg 66: 1158-1162.
- Yacoub WN, Sohn HJ, Chan S, Petrosyan M, Vermaire HM, et al. (2008) Psoas abscess rarely requires surgical intervention. Am J Surg 196: 223-227.
- Gruenwald I, Abrahamson J, Cohen O (1992) Psoas abscess: Case report and review of the literature. J Urol 147: 1624-1626.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 13460
- [From(publication date):
December-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 12436
- PDF downloads : 1024