Short Communication Open Access
Recurrence of Permanent Junctional Re-entry Tachycardia: Indication for Ablation of the Junctional Pathway
Stefan Peters*
Chief Cardiology, St.Elisabeth Hospital gGmbH, Liebenhaller Str. 20, 38259 Salzgitter, Germany
- *Corresponding Author:
- Stefan Peters
Chief Cardiology, St.Elisabeth Hospital gGmbH
Liebenhaller Str. 20, 38259 Salzgitter, Germany
Tel: +49 3411259667
Fax: +49 3411259667
E-mail: H.u.S.Peters@t-online.de
Received date: April 26, 2016; Accepted date: June 16, 2016; Published date: June 21, 2016
Citation: Peters S (2016) Recurrence of Permanent Junctional Re-entry Tachycardia: Indication for Ablation of the Junctional Pathway. Arrhythm Open Access 1:111. doi:10.4172/atoa.1000111
Copyright: © 2016 Peters S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at
Short Communication
Four months ago we treated a 43-year old male patient with a tachycardia-induced cardiomyopathy due to permanent junctional reentry tachycardia who presented with severe dilatation and reduction of left ventricular function. After administration of bisoprolol, the patient resumed sinus rhythm thus ablation of the junctional pathway was not considered necessary [1].
Subsequently, the patient stopped wearing a life vest and stopped taking his prescribed bisoprolol and an ACE inhibitor because of very poor compliance.
The patient was readmitted to hospital because of edema and dyspnoea.
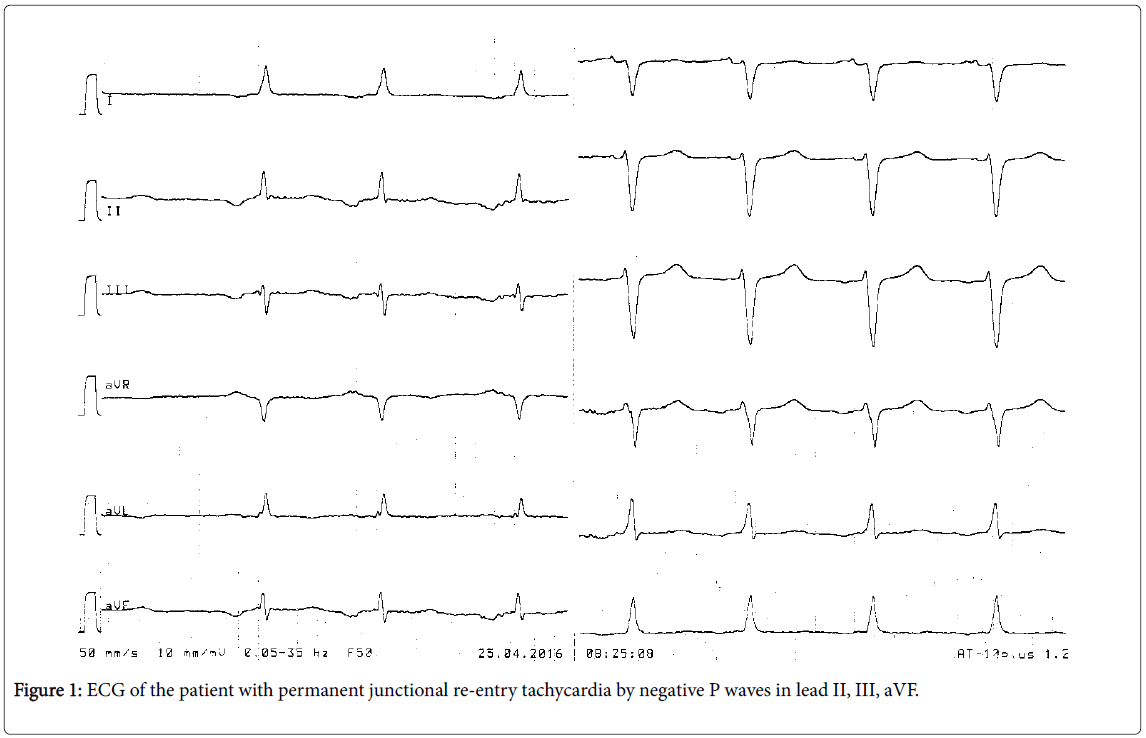
ECG revealed again permanent junctional re-entry tachycardia with negative T-waves in inferior leads (Figure 1).
Echocardiography showed a severe dilatation of the left ventricle of 6.8 cm and a severe reduction of left ventricular function with an ejection fraction of 28%. Furthermore, moderate mitral and tricuspid regurgitation was documented.
After two days resuming of the prior dosage of bisoprolol, the patient still was in incessant permanent junctional re-entry tachycardia, which lead to dramatic deterioration of left ventricular function. This patient was send home and was booked for radiofrequency ablation in an electrophysiological laboratory not far away.
PJRT is a potentially lethal arrhythmia in children and in adolescants with tachycardia induced cardiomyopathy. Although rarely reported, spontaneous resolution is not uncommon. Antiarrhythmic treatment is often effective, especially with amiodarone and verapamil. Radiofrequency ablation should be reserved for older patients and especially in patients with persistent left ventricular dysfunction.
Radiofrequency ablation of this particular accessory pathway remains an intervention at high risk of requiring permanent pacemaker implantation because of its proximity to the septum. The primary ablation success rate is 92%, but the recurrence rate after 9 months is 29% for cryoablation and 8.6% for radiofrequency ablation [2].
In nearly all patients left ventricular function recovers when PJRT is stopped [3]. Despite normalization of left ventricular function, however, a few patients die likely due to structural abnormalities. Experimental data have shown that radiofrequency lesions appear to increase in size with somatic growth, with replacement of normal myocytes with fibrous and elastic tissue forming a potential arrhythmogenic substrate [4].
In adults tachycardia-induced cardiomyopathy is accomplanied by slower tachycardia rates than in children [3]. Radiofrequency catheter ablation is highly effective and should be considered as treatment of first choice in adult patients.
References
- Peters S (2016) Tachycardiomyopathy: A case of dilated cardiomyopathy due to permanent junctionalreentrant tachycardia.Int J Cardiol 207: 233-234.
- Nadji G, Hermida JS, Kubala M, Quenum S, Bakkour H, et al. (2008) Cryoablation of junctional tachycardia at high risk of atrio-ventricular block.Arch Cardiovasc Dis 101: 149-154.
- Meiltz A, Weber R, Halimi F, Defaye P, Boveda S, et al. (2006) Permanent form of junctional reciprocating tachycardia in adults: peculiar features and results of radiofrequency catheter ablation. Europace 8: 21-28
- Vaksmann G1, D'Hoinne C, Lucet V, Guillaumont S, Lupoglazoff JM, et al. (2006) Permanent junctional reciprocating tachycardia in children: a multicentre study on clinical profile and outcome.Heart 92: 101-10 4.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 9789
- [From(publication date):
July-2016 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 8954
- PDF downloads : 835