Rectal Prolapse in Children: How Effective is Non-Operative Treatment?
Received: 05-Jun-2022 / Manuscript No. jpms-22-66323 / Editor assigned: 07-Jun-2022 / PreQC No. jpms-22-66323 / Reviewed: 21-Jun-2022 / QC No. jpms-22-66323 / Revised: 23-Jun-2022 / Manuscript No. jpms-22-66323 / Accepted Date: 29-Jun-2022 / Published Date: 30-Jun-2022 DOI: 10.4172/jpms.1000181
Abstract
Background: Children with rectal prolapse present frequently to the pediatric surgeon through the outpatient clinic and children emergency units. The predisposing factors leading to rectal prolapse could be congenital or acquired. The aim of this study was to evaluate our experience with regards to the management of rectal prolapse in children.
Materials and Methods: This was a retrospective study of children aged 15 years and younger who were managed for rectal prolapse in a teaching hospital in Enugu, Nigeria. This study covered a 5-year period. Only children with clinically obvious rectal prolapse as at the time of presentation were recruited into the study. Diagnosis of rectal prolapse was clinical.
Results: A total of 112 cases of rectal prolapse were seen during the study period. There were 82 (73.2%) males, 30 (26.8%) females and the median age of the patients was 16 months with a range of 5 months to 5 years. Forty-three (38.4%) patients had a preceding history of constipation while 28 (25%) patients had diarrheal diseases before the rectal prolapse occurred. All the patients were managed non-operatively. Almost all the patients recovered following non-operative treatment of the rectal prolapse except for those that were lost to follow up.
Conclusion: Rectal prolapse in children is not an uncommon clinical entity. Non-operative (conservative) treatment may take a long time but it is an effective modality of treatment of pediatric rectal prolapse.
Keywords
Children; Effective; Non-operative; Rectal prolapse;Treatment.
Introduction
Complete rectal prolapse is the circumferential descent of all the layers of the rectum through the anal sphincter. This is in contrast to partial/mucosal rectal prolapse where only the mucosal layer or part of the rectal wall protrudes out of the anal verge [1]. The latter is more common in children. Rectal prolapse may lead to bleeding, obstructed defecation or fecal incontinence. The exact prevalence of rectal prolapse is not known and its etiopathogenesis is a subject of debate [2]. The peak age of pediatric rectal prolapse has been quoted as 1-4 years and there is male gender predominance [3]. Certain factors are known to predispose to rectal prolapse. The anatomical factors include vertical configuration of the sacrum, greater mobility of the sigmoid colon, loose attachment of the rectal mucosa to the underlying muscles and poorly developed Houston’s valves [4]. Other factors may include chronic constipation, chronic cough, pertussis, malnutrition, rectal polyp, urinary obstruction and surgical procedure near the anus [5, 6]. Rectal prolapse in children reduces spontaneously or may require manual pressure for its reduction. Complete resolution of rectal prolapse can happen spontaneously or within 12 months of nonoperative management if the underlying conditions and precipitating factors are addressed adequately [2]. There are chances of recurrence or persistence of rectal prolapse but this is very low. About 10% of rectal prolapse may not respond to non-operative treatment after 12 months and this group of patients will benefit from operative treatment [5]. The aim of this study was to evaluate our experience with regards to the management of rectal prolapse in children.
Materials and Methods
This was a retrospective study of children aged 15 years and below who were managed for rectal prolapse between January 2016 and December 2020 at the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) Enugu, Nigeria. Only children with clinically obvious rectal prolapse as at the time of presentation were recruited into the study. Diagnosis of rectal prolapse was clinical.Patients who have had an intervention for rectal prolapse at a peripheral hospital before referral to ESUTH for further treatment were not included into this study. Patients older than 15 years of age were also excluded. ESUTH is a tertiary hospital located in Enugu, South East Nigeria. The hospital serves the whole of Enugu State, which according to the 2016 estimates of the National Population Commission and Nigerian National Bureau of Statistics, has a population of about 4 million people and a population density of 616.0/km2. The hospital also receives referrals from its neighboring states. Information was extracted from the case notes, operation notes,operation register and admission-discharge records. The information extracted included the age of the patient at presentation, gender, duration of the rectal prolapse before presentation to the hospital, any preceding illness, procedure (intervention) performed, duration of hospital stay and outcome of treatment. The follow-up period was 12 months. Ethical approval was obtained from the ethics and research committee of ESUTH and informed consent was not obtained from the patients’ caregivers due to retrospective nature of the study. Statistical Package for Social Science (SPSS) version 21 (manufactured by IBM Corporation Chicago Illinois) was used for data entry and analysis. Data were expressed as percentages, median, mean, and range.
Results
Patients’ demographics
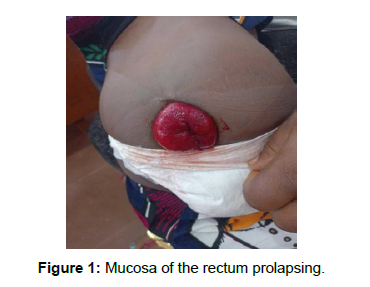
A total of 112 cases of rectal prolapse were seen during the study period and form the basis of this report. There were 82 (73.2%) males, 30 (26.8%) females and the median age of the patients was 16 months with a range of 5 months to 5 years. The median duration the rectal prolapse has stayed before presentation to the hospital was 3 days, range 2 to 4 days. The mean duration of hospital stay was 5 days, range 4 days to 12 days. Clinical pictures of some of the patients are shown in (Figures 1 and 2).
Preceding illness and type of rectal prolapse
Forty-three (38.4%) patients had a preceding history of constipation while 28 (25%) patients had diarrheal diseases before the rectal prolapse occurred. A history of preceding illness could not be obtained in 41 (36.6%) patients. All the patients had mucosal (partial) prolapse.
Intervention performed
All the patients were managed non-operatively. This non-operative treatment consists of manual reduction of the prolapsed rectum and plastering of both gluteal muscles together for 48 to 72 hours (Figure 3). A hole is created at the middle of the plaster for the passage of fecal matter when the child defecates. Digital physiotherapy is started when the rectal prolapse is reduced. Digital physiotherapy consists of insertion of a finger into the anal canal and the finger left in the anal canal for 5-10 minutes. This digital physiotherapy is performed daily for 6 weeks at home by either of the parents.
Treatment outcome
One hundred and six (94.6%) patients did not experience any recurrence of the rectal prolapse during the follow up period. Six (5.4%) patients were lost to follow up. None of the patients had operative treatment of the rectal prolapse.
Discussion
Historically, rectal prolapse was recognized as early as 1500 BC. In 1831, Frederick Salmon, published a paper titled “Practical Observation on Prolapsus of the Rectum” where he discussed the treatment of rectal anomalies [7]. Hippocrates described treatment of rectal prolapse by hanging the patients upside in a tree and applying sodium hydroxide to the mucosa [8]. In medieval periods, rectal prolapse was prevented by causing scar formation. These scars were obtained by burning the anus or by use of a stick [8]. In 1912, Moschcowitz described the etiology of rectal prolapse. Lockhart and Mummery, in 1939, attributed rectal prolapse to malnutrition, careless nursing, diarrheal and wasting illnesses [9]. The natural history of rectal prolapse is as follows: Initially, the rectum protrudes from the anus only after a bowel movement and usually retracts spontaneously when the patient stands up. As the days go by, the disease progresses, the rectum protrudes more often particularly on straining but again reduces spontaneously. With time, the rectum can no longer reduce spontaneously and requires manual reduction. At the later stages of the rectal prolapse, the rectum stays outside the anal opening and is prone to desiccation, ulceration, thrombosis and gangrene. There may be associated problems of fecal incontinence. In the present study, more males were affected. Other series also documented this male predominance [10, 11]. However, another study reported equal distribution of rectal prolapse between males and females [12]. The reason for the gender disparity/equality of rectal prolapse in children remains a subject of further research. The mean age of our patient was 16 months. Rentea et el reported that rectal prolapse is a common and self-limiting condition in infancy and early childhood [13]. It is worthy to note that rectal prolapse can occur at any age including neonates and older children [2, 14]. The presentation of the patients to the hospital was delayed; this is demonstrated in the mean interval of 2 days before presentation to the hospital. None of the patients presented within 24 hours of onset of the prolapse. Poverty, ignorance and lack of parental awareness may explain the delayed presentation. The mean duration of hospitalization of 5 days was the time required for the reduced rectal mucosa to adhere to the rectal submucosa and the rectal prolapse resolved. Majority of the patients in the current series (onethird) had a preceding history of constipation prior to the onset of the rectal prolapse. This is consistent with the report of other reports on pediatric rectal prolapse [6, 15, 16]. Even in adult patients, constipation has been documented as a risk factor for rectal prolapse [17]. Other risk/predisposing factors for rectal prolapse include diarrhea, chronic cough, cystic fibrosis, straining during defecation. In children, mucosal prolapse is more common than complete prolapse. The increased incidence of mucosal prolapse in children is possibly explained by the poor fixation of the submucosa to mucosal layer of the bowel. All our patients had mucosal prolapse. Complete rectal prolapse can be differentiated from the mucosal prolapse by the presence of multiple circular folds on the prolapsed mucosa of the complete rectal prolapse and multiple thickness layer of the prolapsed rectum on palpation.
The entire patients in the current series were treated non-operatively (conservatively). Sialakas et el reported that treatment of rectal prolapse is mainly conservative and is directed at the underlying condition [4]. This non-operative treatment of rectal prolapse in children was also emphasized by other researchers by addressing the associated and precipitating factors such as constipation, dietary manipulation, and treatment of infective diarrhea, parasitic infestations, better toilet training methods and biofeedfeed training [2, 18]. Operative treatment of rectal prolapse is reserved for intractable cases. This operative treatment of rectal prolapse could be accomplished either transanally (perineal approach) or trans abdominally. However, no single surgical procedure is appropriate for all patients with rectal prolapse [19]. The overall management outcome of rectal prolapse in the index study is good. More than fourth-fifth of the patients achieved sound recovery and had no recurrence of the rectal prolapse. Meshram et al. also reported successful non-operative treatment of rectal prolapse [2].
Conclusion
Rectal prolapse in children is not an uncommon clinical entity. Non-operative (conservative) management may take a long time but it is an effective modality of treatment of pediatric rectal prolapse. Future studies will be tailored to determine the predictive factors that influence the success of this non-operative treatment of rectal prolapse.
References
- Goligher JC (1964) Prolapse of the rectum. Postgrad Med J 40: 125-129.
- Meshram GG, Kaur N, Hura KS (2018) Complete rectal prolapse in children: Case report, review of literature, and latest trends in management. Open Access Maced J Med Sci 6: 1694-1696.
- El-Chammas KI, Rumman N, Doh VL, Quintero D, Goday PS, et al. (2015) Rectal prolapse and cystic fibrosis. J pediatr Gastroenterol 60: 110-112.
- Sialakas C, Vottler TP, Anderson JM (1999) Rectal prolapse in pediatrics. Clin Pediatr 38: 63-72.
- Antao B, Bradley V, Roberts JP, Shawis R (2005)Management of rectal prolapse in children. Dis Colon Rectum 48: 1620-1625.
- Cares K, El-Baba M (2016) Rectal prolapse in children: Significance and Management. Curr Gastroenterol Rep 18: 22.
- Ballantyne GH (1991) The historical evolution of anatomic concepts of rectal prolapse. Semin Colon Rectal Surg 2: 170-179.
- Shin EJ (2011) Surgical treatment of rectal prolapse. J Korean Soc Coloproctol 27: 5-12.
- Lockhart-Mummery JP (1939) surgical procedures in general practice. Br Med J 1345-1347.
- Sarmast MH, Askarpour S, Peyvasteh M, Javaherizadeh H, Mooghehi-Nezhad M, et al. (2015) Rectal prolapse in children: a study of 71 cases. Prz Gastroenterol 10: 105-107.
- Bahador A, Foroutan HR, Hosseini SM, Davani SZ (2008) Effect of submucosal alcohol injection on prolonged rectal prolapse in infants and children. J Indian Assoc Pediatr Surg 12: 11-13.
- Safar B, Vernava AM (2008) Abdominal approaches for rectal prolapse. Clin Colon Rectal Surg.21: 94-99.
- Rentea RM, St Peter SD (2018) Pediatric rectal prolapse. Clin Colon Rectal Surg 31: 108-116.
- Traisman E, Conlon D, Sherman JO (1983) Rectal prolapse in two neonates with Hirschsprung’s disease. Am J Dis Child 137: 1126-1127.
- Aoki Y, Kitazawa K (2017) A case of pediatric rectal prolapse without spontaneous reduction on arrival. BMJ Case Rep 220608
- Zempsky WT, Rosenstein BJ (1988) The cause of rectal prolapse in children. Am J Dis Child 142: 338-339.
- Tuncer A, Akbulut S, Ogut Z, Sahin TT (2021) Management of irreducible giant rectal prolapse. Int J Surg Case Rep 88: 106485.
- Zganjer M, Cizmic A, Cigit I, Kljenak A (2008) Treatment of rectal prolapsein children with cow milk injection sclerotherapy: 30-year experience. World J Gastroenterol 14: 737-740.
- Brown AJ, Anderson JH, McKee RF, Finlay IG (2004) Strategy for selection of type of operation for rectal prolapse based on clinical criteria. Dis Colon Rectum. 47: 103-107.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Emeka CK, Patrick AL, Chikaodili ET (2022) Rectal Prolapse in Children: How Effective is Non-Operative Treatment? J Paediatr Med Sur 6: 181. DOI: 10.4172/jpms.1000181
Copyright: © 2022 Emeka CK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.