Recovery of Biopsychosocial Functions Following 15 Years after Spinal Cord Injury
Received: 26-Aug-2017 / Accepted Date: 12-Sep-2017 / Published Date: 22-Sep-2017 DOI: 10.4172/2329-6879.1000264
Abstract
Background: Spinal cord injury (SCI) causes the loss of biopsychosocial functions, body dysfunctions, decreased functional independence level, limitations in activities, and participation restriction. For recovery of functioning, comprehensive inpatient rehabilitation programs are necessary, which are more focused on recovery of physical status, capacity, functional independence level, maintenance of existing skills, and improvement of activities in daily life. In the long-term context, functioning improves naturally by engaging in various activities of everyday life. The aim of this study was to evaluate the changes in functioning and functional independence following 15 years after SCI.
Material and Methods: A total of 109 people with SCI were enrolled in the study during 2007-2015. The study was carried out during inpatient rehabilitation in the Centre of Rehabilitation, Physical and Sports Medicine. The second assessment was performed after 1-15 years. For evaluation functional independence, the Functional Independence Measure (FIM) was used. Functional problems were assessed by the Comprehensive ICF Core Set for SCI.
Results: Rehabilitation mostly increased the functional independence level and significantly decreased the severity of body dysfunctions and participation restriction in daily life. In the long-term context, the reached functional independence level of persons with SCI did not change significantly and remained stable, but dysfunctions of muscle strength, physical endurance, moving around, and participation in household and leisure activities significantly decreased. In the long-term context, the percentage of employed subjects and having higher education increased.
Conclusion: Rehabilitation after SCI effectively improves patients’ severe functional problems, but in the following periods, functioning increases each year after SCI by naturally engaging in daily living activities.
Keywords: Longitudinal studies; Spinal cord injuries; Rehabilitation
19260Background
During recent years, intensively changing people’s living habits, associated with changes in the country’s social, economic, and demographic situation, are increasing the risk of traumatism; therefore, spinal cord injury (SCI) are more common especially among young people. The incidence of SCI in developed European countries is increasing: an average of 25.5 new SCI cases per million population per year (95% CI: 21.7 to 29.4), with frequency in different countries ranging from 2.1 to 130.7 new SCI cases each year [1,2]. The incidence of SCI in Lithuania is 24 new SCI cases per million per year [3-5]. Many studies [6-8] have confirmed that SCI more often occurs among young and physically active men aged from 29.7 to 35.2 years on average (from 72.1% to 85.3%). In Lithuania, two-thirds of people with SCI are younger than 30 years, and the ratio of men to women is 3.2:1.0 [9]. The prevalence of traumatic SCI ranges from 74.4% to 82.0% of all SCI cases, and of them, 49.4% to 62.1% are caused by motor transport accidents; 26.7% to 43.1%, by falls or jumps into water; and 16.8% to 22.3%, sports injuries [10].
SCI causes a loss of biopsychosocial functions: altered body functions, decreased physical capacity and disrupted mobility, functional independence in daily life and social activities [1]. After SCI for recovery of biopsychosocial functions, comprehensive multidisciplinary rehabilitation as a biopsychosocial model is necessary, which is more focused on improving the physical status and physical capacity as well as developing functional independence and mobility skills. During re-rehabilitation inpatient programs (1-3 years after SCI), efforts are made to maintain the existing skills and to improve functioning, physical activity, participation in daily living activities, and successful social integration [11,12]. However, during this period, psychological and social problems and obstacles emerge as people with SCI often distance themselves from society [13]. In the long-term period, physical strength, endurance, and functional skills of people with SCI slightly improve, and functioning and socialization processes improving each year after SCI by naturally engaging and participating in everyday life show capabilities to adapt to the environment, greater involvement in different activities and better outcomes although it often depends on the surrounding environment [14,15].
Other authors [16,17] discuss about associations between functioning in daily life of this population and social interactions as well as relationships with loved ones (friends, family, acquaintances), community support by ensuring training of independent living skills and adjustment to a new life, continuity and integration of selfrealization in the community [18]. It should be noted that depending on successfully solved problems, favorable social conditions, social support, and state policy during the primary rehabilitation program in the postacute period after SCI, an employment and socialization process of these people develops in the long-term period [19,20].
Recently, it has been reported that changes in daily activity of people with SCI are more associated with the ability to use their skills [21] and opportunities to maintain a physically active lifestyle [22,23]. People with better physical capacity indicators are more active in daily and community life, better manage self-control mechanisms, and feel more emotionally stable [24,25]. According to authors [26,27], it is important during the inpatient rehabilitation program to promote physically active lifestyle and activities in daily life as well as to increase motivation to engage in vigorous physical activity not only during exercise, training or active leisure, but also during household activities.
In scientific literature, there is a lack of data on changes in biopsychosocial functions (body functions, activities and participation in daily life) of persons who sustained SCI, and the data available are ambiguous. Moreover, longitudinal studies that would evaluate the extent of the problems experienced in the context of time, i.e. during comprehensive multidisciplinary inpatient rehabilitation in acute, postacute, and long-term periods (1–15 and more years) after SCI, are scarce. In our longitudinal study, relevant and insufficiently investigated changes in functioning during different periods after SCI, in order to determine exact time during which the highest recovery of body functions was achieved, the highest level of functional independence was reached, and subjects were mostly physically and socially active in daily living activities, were investigated. The latter knowledge would allow us to understand the problems of this population during rehabilitation and after discharge in order to plan and maintain the strategy of necessary support and means for improvement of the rehabilitation system and successful social integration after SCI.
Material and Methods
Study population
A total of 109 people with SCI were enrolled in a 3-period longitudinal study: during the primary inpatient rehabilitation program, re-rehabilitation inpatient program, and in long-term period. Patients after SCI onset participated in the primary inpatient rehabilitation program (post-acute period after SCI onset) at the Centre of Rehabilitation, Physical and Sports Medicine, Vilnius University Hospital Santaros Clinics (2007-2015) were involved in our research. During inpatient re-rehabilitation (1–3 years after SCI), these patients were involved in our research for the second time. In the long-term period (3–15 years after SCI), these patients were involved in our study for the third time during independent life skills and recreation camps in the Landscape Therapy and Recreation Centre. It is important to note, that 35 participants (of 109 participants) in long-term period have experienced SCI 7-15 years ago, and in primary and re-rehabilitation inpatient programs participated in the Centre of Rehabilitation, Physical and Sports Medicine, Vilnius University Hospital Santaros clinics over 7 years ago, therefore a retrospective analysis of medical documentation was carried out. The participants in long-term period were divided into 3 groups according the time after SCI: 1) 3–5 years (n=38); 2) 5-10 years (n=38); and 3) 10-15 years (n=33).
The inclusion criteria were as follows: age of 18-59 years, traumatic or non-traumatic SCI AIS A, B and C level, stable health status, and voluntary participation (confirmed by a signature in the informed consent).
The exclusion criteria were as follows: age of more than 60 years, SCI at the high level (cervical C1-C4 level and/or above it), SCI level AIS D and E (patients were excluded in this research because they recovered quickly and they do not experience such severe functional problems), oncological diseases, and unstable health status.
Ethical issues
Ethical approval was obtained from the Lithuanian Bioethics Committee (protocol No. 1.17/3/2011). All the participants provided written informed consent at initial assessment. Participants were required to consent to complete the questionnaire and undergo a brief examination of physical and functional status as well as evaluation of functional problems and functioning level in activities of daily living.
Instruments
In order to assess the changes in biopsychosocial functions and to determine the most frequent functional problems during different periods, biopsychosocial functions were evaluated on admission to and at the end of inpatient primary/re-rehabilitation programs, and in the long-term context during independent life skills camps, the subjects were evaluated once.
Sociodemographic and SCI-related characteristics
In order to analyse the changes in socio-demographic characteristics, employment status, activities in everyday life and with SCI related information (SCI level, grade and time after SCI onset), each person had to complete a questionnaire during a direct interview.
Functional Independence Measure (FIM)
In order to analyse the efficiency of rehabilitation after SCI, experienced health problems, changes in everyday skills and functional status, the Functional Independence Measure (FIM) was applied. This test is a very sensitive tool that allows the evaluation of changes in functional status and capacity of subjects of different age, sex, and SCI level during rehabilitation and after discharge and allows the accurate determination of need for assistance in physical activities in everyday life. In order to analyze a functional independence level in more detail, we also examined the changes in 13 physical items of the FIM score (physical FIM), defining disability in motor function (self-care, sphincter control, and mobility).
Comprehensive ICF Core Set for SCI
In order to assess the changes in subjects’ functioning and to determine dysfunctions, the Comprehensive International Classification of Functioning (ICF) Core set for SCI was used. General mental functions, sensory functions and pain, neuromusculoskeletal and movement-related functions, physical endurance, weight maintenance functions, activities and participation in different life situations were evaluated. According to whether subjects had or did not have functional problems, they were divided into the groups (Table 1).
| Body functions | |
| Functional problems (having/not having) | Assessment classification |
| Unidentified dysfunction–body dysfunction is absent or very slight | 0 – no dysfunction (0%–4%) |
| 1 – slight dysfunction (5%–24%) | |
| Identified dysfunction–severe (moderate, high and complete) body dysfunction | 2 – moderate dysfunction (25%–49%) |
| 3 – high dysfunction (50%–95%) | |
| 4 – complete dysfunction (96%–100%) | |
| Activity and Participation | |
| Unidentified limitation of activity – the difficulty of participating in activities is absent or very slight | 0 – no difficulty (0%–4%) |
| 1 – slight difficulty (5%–24%) | |
| Identified limitation of activity – severe (moderate, high and complete) difficulty of participating in activities | 2 – moderate difficulty (25%–49%) |
| 3 – high difficulty (50%–95%) | |
| 4 – complete difficulty (96%–100%) |
Table 1: The distribution of subjects according to functional problems.
Statistical analysis
Statistical analysis was performed using SPSS 19.0 computer software statistical package. Descriptive statistics was used for the calculation of the numerical characteristics of a variety of demographic, medical and sociodemographic indicators. The chi-square (χ2) criterion was used for the comparison of qualitative variable frequency, expressed as a percentage. The student t test for independent/dependent samples was applied to compare the means of independent/dependent variables. For the comparison of dichotomous variables in different moments of rehabilitation, McNemar criteria were used; for the comparison of dependent samples when variables were measured on an ordinal scale, the Wilcoxon criterion, and to compare the means of variables of different groups, univariate ANOVA. In order to determine which groups significantly differed, we applied a post-hoc multiplecomparison procedure and Tukey HSD. The differences between the comparison groups were considered statistically significant when P<0.05.
Results
Sociodemographic and SCI-related characteristics
SCI occurred significantly frequently in men than women (n=82, 75.2% and n=27, 24.8%, respectively). The mean age of the subjects when they experienced SCI was 29.75 years (SD, 9.51 years; range, 18–59 years; 95% CI, 28.57 to 31.45 years). Men and women were agematched (p=0.599). Nearly 70% of the subjects belonged to the 18-34 year age group: 32.1% were aged <24 years; 37.6%, 25-34 years; 23.9%, 35-49 years; and 6.4%, 50 and more years.
Traumatic SCI was more frequent than nontraumatic SCI (n=96, 88.1% vs. n=13, 11.9%) and its frequency was similar in both men and women (p>0.05). Motor accidents (42.2%), sports or diving into water (22.0%), and domestic accidents and falls from height (20.2%) were the most common causes of traumatic SCI. Even 43.1% of the subjects who sustained SCI consumed alcohol within 6 hours before SCI. The causes of nontraumatic SCI (11.9% of subjects) were related to medical and surgical interventions or complications and other specific causes (suicide attempts, abscesses, and infections). SCI most frequently occurred at the thoracic level (n=62, 56.9%); the prevalence of SCI at the cervical and lumbar levels was 35.8% (n=39) and 7.3% (n=8), respectively. SCI classified as AIS A level predominated (74.3%), AIS B (15.4%), and AIS C (10.2%).
After SCI, 58 (53.2%) subjects were single; 32 (29.4%), married; 10 (10.9%), divorced; 2 (1.83%), widowed; and 7 (6.4%), living with a girlfriend / boyfriend. During the long-term period, unmarried persons still accounted for the largest proportion (n=48, 44.0%), but the percentage of living with a girlfriend/boyfriend increased to 11.9% (n=13).
The results showed that subjects studied and actively sought to gain better education level: at the time when SCI occurred, 33.9% of the subjects had college education; 31.2%, special/advanced vocational education; and 18.3%, higher education. During the long-term period, the percentage of the subjects with higher education accounted to 25.7% subjects. It should be noted that the greatest subjects’ enrollment in studies was observed during the first 5 years after SCI.
During the long-term period, the percentage of employed subjects 2 doubled as compared with the first 3 years after SCI (Table 2). In the first year after discharge from primary rehabilitation, 8.3% of the subjects were employed, and of them, 66.7% returned to the workplace where they worked before SCI onset. In the long-term period, dominated permanent job and jobs at home (Table 2).
| Employment status | <1 year after SCI | 1–3 years after SCI | 3–15 years after SCI |
| Unemployed | 100 (91.7) | 90 (82.6) | 61 (56.0) |
| Employed | 9 (8.3) | 19 (17.4) | 48 (44.0) |
| P* | 0.001 | ||
| P* | <0.001 | ||
| Permanent job | 6 (66.7) | 7 (36.8) | 12 (25.0) |
| Private business | 3 (33.3) | 3 (15.8) | 7 (14.6) |
| Short-term jobs | – | – | 6 (12.5) |
| Work to order | – | 2 (10.6) | 6 (12.5) |
| Job at home | – | 7 (36.8) | 17 (35.4) |
Table 2: Distribution of the subjects by employment status in a 1–15 years after SCI.
Full-time jobs of mild or very mild intensity dominated, though the percentage of people having jobs of average intensity increased in the long-term period (p<0.001) (Table 3).
| Duration of working day | <1 years after SCI | 1–3 years after SCI | 3–15 years after SCI |
| Full-time (6–7 h/day) | 4 (44.4) | 10 (52.6) | 15 (31.3) |
| Half-time (3–4 h/day) | 2 (22.2) | 5 (26.3) | 13 (27.1) |
| Few hours a day | 3 (33.4) | 2 (10.5) | 12 (25.0) |
| According to the need | – | 2 (10.5) | 8 (16.7) |
| P* | 0.001 | ||
| <0.001 | |||
Table 3: Distribution of the subjects by duration of working day.
The changes of functional independence
To determine the changes of functional independence during inpatient rehabilitation programs and in long-term period taking into account age, gender, level and type of SCI, we analyzed the changes of FIM score means. Participation in primary inpatient rehabilitation program statistically improved independence level and was found the largest increase in average FIM score (change of 31.85 ± 11.78 score, p<0.001). At the beginning of re-rehabilitation inpatient program, comparing with the end of primary rehabilitation program, FIM score mean decreased (negative change –2.50 ± 5.70, p<0.001). However, the FIM score during the re-rehabilitation inpatient program significantly increased (change 12.54 ± 4.41; p<0.001) and in the long-term period, subjects reached the highest independence level (change of 6.42 ± 4.94 score, p<0.001) (Table 4).
| rowspan="2">Period | Total FIM score | ||
| mean±SD | 95% CI | ||
| Primary rehabilitation program (n=109) | on admission | 53.83±9.62 | 61.28–74.89 |
| at discharge | 85.68±12.21 | 80.95–92.57 | |
| Re-rehabilitation program (n=109) | on admission | 83.18±10.30 | 79.42–86.62 |
| at discharge | 95.72±9.87 | 88.8–101.69 | |
| Long-term period (n=109) | 102.15±9.79 | 101.12–106.47 | |
| P* | <0.001 | ||
| Long-term period (n=109) | |||
| 3–5 years after SCI (n=38) | 99.87±11.09 | 97.78–107.94 | |
| 5–10 years after SCI (n=38) | 103.98±8.71 | 99.54–111.25 | |
| 10–15 years after SCI (n=33) | 103.19±6.82 | 101.25–111.71 | |
| P* | 0.179 | ||
Table 4: The total FIM score in different periods after SCI.
Analysis of changes in functional independence from the beginning of primary inpatient rehabilitation to different long-term periods (3-5 years, 5-10 years and 10-15 years after SCI) revealed that at the beginning of the primary inpatient rehabilitation program the subjects’ independence level was similar (f=1.196, p=0.306). In the long-term period, there was a significant difference in the FIM changes between the groups (level of significance of Tukey HSD criteria, p<0.05): subjects had a significantly lower FIM score at <5 years than at 5-10 years after SCI (p=0.036), but there was no significant difference when compared to 10-15 years after SCI (p=0.087) (Table 5).
| FIM score in different periods after SCI (mean±SD) | P* | ||
| The beginning of primary rehabilitation (n=109) | 53.83±9.62 | 0.001 | 0.179 |
| <5 years after SCI (n=38) | 99.87±11.09 | ||
| 5–10 years after SCI (n=38) | 103.98±8.71 | ||
| 10–15 years after SCI (n=33) | 103.19±6.82 | ||
| FIM score changes from the beginning of primary rehabilitation to different long-term periods (mean of changes±SD) | |||
| The beginning of primary rehabilitation (n=109) | |||
| <5 years after SCI (n=38) | 44.94±11.65 | 0.036 | 0.087 |
| 5–10 years after SCI (n=38) | 51.01±8.79 | ||
Table 5: The comparison of FIM score changes in the different periods after SCI.
The analysis of the FIM score in different periods after SCI showed that functional independence level more increasing significantly during first 5 years after SCI onset (p<0.05) and in 5-10 and 10-15 years after SCI onset periods significantly not changed and FIM level remains stability (p>0.05).
The FIM score of subjects with a different SCI level was significantly increased from the beginning of inpatient rehabilitation at different periods: subjects with SCI at the cervical level achieved an independence level lower by a score of 14.97±5.83 than subjects with SCI at the thoracic and lumbar levels (p<0.05) (Table 6).
| Period | Functional Independence level, score | |||||||||||
| Cervical level (n=39) | Thoracic level (n=62) | Lumbar level (n=8) | ||||||||||
| mean±SD | 95% CI | mean±SD | 95% CI | mean±SD | 95% CI | |||||||
| Primary rehabilitation program (n=109) | on admission | 49.28±7.98 | 41.12–52.87 | 56.08±9.57 | 54.12–61.25 | 58.50±10.1 | 51.21–69.45 | |||||
| at discharge | 72.30±16.74 | 65.45–78.54 | 96.36±16.59 | 92.7–104.63 | 93.13±5.89 | 86.57–97.54 | ||||||
| Re-rehabilitation program (n=109) | on admission | 70.77±8.91 | 64.36–76.79 | 88.18±6.32 | 86.14–104.7 | 93.38±9.21 | 88.31–102.25 | |||||
| at discharge | 86.71±15.09 | 80.45–89.12 | 106.65±8.14 | 102.1–107.9 | 101.63±10.3 | 98.56–109.27 | ||||||
| Long-term period (n=109) | 93.10±8.00 | 90.12–95.17 | 107.39±6.26 | 105.6–109.2 | 105.63±8.7 | 99.87–111.36 | ||||||
| P* | <0.001 | <0.001 | <0.001 | |||||||||
| Long-term period | ||||||||||||
| 3–5 years after SCI (n=38) | 87.19±14.44 | 82.65–93.87 | 103.21± 8.87 | 98.2–104.36 | 108.96±12.78 | 101.2–109.87 | ||||||
| 5–10 years after SCI (n=38) | 89.80±15.70 | 83.45–95.74 | 105.96±12.78 | 102.7–107.17 | 111.0±12.53 | 106.2–112.43 | ||||||
| 10–15 years after SCI (n=33) | 95.24±8.75 | 91.24–98.13 | 104.91± 2.14 | 103.3–108.49 | 113.39±6.21 | 108.54–113.52 | ||||||
| P* | 0.097 | - | 0.123 | - | 0.083 | - | ||||||
Table 6: The comparison of total FIM score between subjects with different SCI level.
Comparison of the functional independence level between the subjects of different age showed that men and women did not differ significantly (p>0.05).
Changes in functioning
Body functions: In order to identify the most common problems of functioning during different periods after SCI, the component Body Functions was analysed. Analysis of general mental functions showed that the majority of subjects had only slight emotional (b152), sleep (b134) and energy and drive (b130) disorders, except for an increase in self-confidence problems during the first 3 years after SCI (P>0.05), although in the long-term period, these problems significantly decreased (P=0.041) (Table 7).
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | |||
| on admission | at discharge | on admission | at discharge | |||
| b1266 Self-confidence | 21 (19.3) | 24 (22.3) | 29 (26.6) | 27 (24.8) | 20 (18.5) | |
| 1 | 0.289 | |||||
| P* | 0.157 | 0.041 | ||||
| b130 Energy and drive functions | 16 (14.6) | 17 (15.3) | 16 (14.6) | 13 (12.3) | 14 (11.6) | |
| 0.658 | 0.245 | |||||
| P* | 0.365 | 0.089 | ||||
| b134 Sleep functions | 53 (48.3) | 37 (33.7) | 40 (36.8) | 38 (35.1) | 29 (26.5) | |
| 0.018 | 0.459 | |||||
| P* | 0.123 | 0.056 | ||||
| b152 Emotional functions | 26 (24.2) | 22 (20.5) | 24 (22.3) | 23 (21.5) | 20 (18.5) | |
| 0.157 | 0.100 | |||||
| P* | 0.248 | 0.527 | ||||
Table 7: Distribution of the subjects according to general mental dysfunctions.
During different periods after SCI, subjects’ sensory intensity of pain (b280) significantly reduced (P<0.001): after SCI the majority of patients experienced severe (complete, high, or moderate) pain in head and neck, back, and upper extremities, which significantly decreased during inpatient rehabilitation programs and in the long-term period only slight pain of these localizations persisted (p<0.05). However, the percentage of the subjects experiencing pain in upper extremities and joints significantly increased in the long-term period (p<0.001) (Table 8).
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | ||
| on admission | at discharge | on admission | at discharge | ||
| b28010 Pain in head and neck | 51 (46.8) | 45 (41.3) | 49 (45.0) | 46 (42.2) | 39 (35.8) |
| 0.008 | 0.014 | ||||
| P* | 0,845 | 0.011 | |||
| b28013 Pain in back | 96 (88.0) | 92 (84.3) | 87 (79.8) | 78 (71.6) | 93 (84.6) |
| 0.001 | 0.001 | ||||
| P* | 0.147 | 0.054 | |||
| b28014 Pain in upper extremities | 53 (48.7) | 52 (47.6) | 58 (52.6) | 44 (40.4) | 68 (61.8) |
| 0.001 | <0.001 | ||||
| P* | 0.583 | <0.001 | |||
| b28015 Pain in lower extremities | 18 (17.4) | 17 (15.8) | 12 (10.9) | 9 (7.3) | 10 (9.2) |
| 1 | 0.162 | ||||
| P* | 0.102 | 0.617 | |||
| b28016 Pain in joints | 4 (3.9) | 3 (2.8) | 5 (4.7) | 5 (4.7) | 11 (9.8) |
| 0.157 | 0.564 | ||||
| P* | 0.317 | 0.008 | |||
Table 8: Distribution of the subjects according sensory of pain dysfunctions
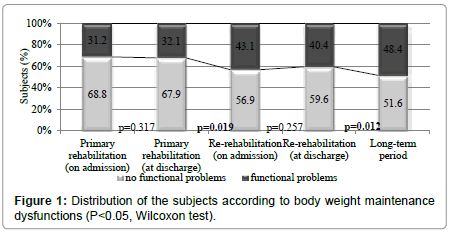
Table 9 shows that after SCI for the majority of subjects’ the physical endurance (b455) was completely impaired and prevailed severe (complete, high or moderate) dysfunctions of muscle strength (b730): whole body muscles (48.5% of subjects), upper limbs muscles (44.1%) and muscle endurance (86.2%). During inpatient rehabilitation program statistically improved the muscle functions (p<0.001), but physical endurance statistically not have improved (p>0.05). The greatest improvement of physical endurance and supporting muscle functions was observed in long-term period (p<0.05). Muscle tone dysfunctions significantly increased during the primary inpatient rehabilitation program (p=0.025) and decreased during the long-term period (p=0.015). Body weight maintenance (b530) dysfunctions significantly increased in the period between inpatient rehabilitation programs and long-term period (p<0.001).
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | ||
| on admission | at discharge | on admission | at discharge | ||
| b455 Exercise tolerance functions | 72 (66.1) | 65 (60.2) | 62 (56.9) | 57 (52.3) | 31 (28.4) |
| 0.157 | 0.059 | ||||
| P* | 0.228 | <0.001 | |||
| b7300 Upper limbs muscles power functions | 51 (46.6) | 48 (44.1) | 45 (41.1) | 45 (41.1) | 44 (40.4) |
| 0.046 | 0.873 | ||||
| P* | 0.059 | 0.055 | |||
| b7305 Whole body muscles | 53 (49.2) | 49 (44.9) | 47 (43.2) | 41 (38.2) | 36 (32.9) |
| 0.046 | 0.004 | ||||
| P* | 0.56 | 0.003 | |||
| b7603 Supporting muscle functions | 52 (47.7) | 45 (41.3) | 43 (39.4) | 38 (34.8) | 27 (24.6) |
| 0.035 | 0.002 | ||||
| P* | 0.593 | <0.001 | |||
| b735 Muscle tone functions | 22 (20.3) | 28 (25.7) | 23 (20.9) | 21 (19.1) | 16 (14.6) |
| 0.025 | 0.159 | ||||
| P* | 0.037 | 0.015 | |||
| b740 Muscle endurance functions | 107 (99.1) | 97 (89.0) | 102 (94.4) | 96 (88.1) | 82 (75.4) |
| <0.001 | <0.001 | ||||
| P* | 0.039 | <0.001 | |||
Table 9: Distribution of the subjects according problems in muscle functions.
The percentage of the subjects with body weight maintenance (b530) dysfunctions significantly increased on admission to the rerehabilitation program and rehabilitation in the long-term period (Figure 1).
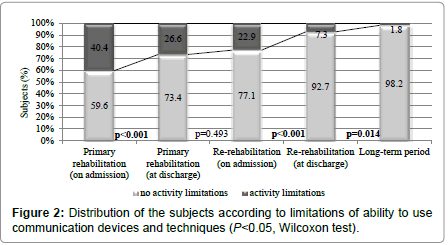
Activities and participation: The positive impact of participation in primary and re-rehabilitation programs on subjects’ mobility skills can be seen in Tables 10 and 11. On admission to the inpatient rehabilitation program, 98.2% to 100% of the subjects had complete mobility limitations: ability to change the sitting position and to lie down (d4103), to bend down/sideways (d4105), to move the body’s center of gravity while sitting (d4106), to maintain a body position for required time (d415) and to move (d420); subjects had complete limitations in moving around in wheelchair at home (d4600) other buildings (d4601) outside the houses and other buildings (d4602) moving around using equipment (d465); and difficulties in ability to use communication devices and techniques (d360). The positive impact of participation in inpatient rehabilitation programs was assessed for these actions: the greatest improvement in mobility (p<0.001) and significantly decreased limitations in moving around (p<0.001) were documented. In the longterm period, subjects experienced least limitations in mobility and moving in different locations, although many subjects (48.4%) still had difficulties moving in buildings and outside.
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | ||
| on admission | at discharge | on admission | at discharge | ||
| d4103 Sitting | 109 (100) | 52 (47.7) | 56 (51.4) | 21 (19.3) | 14 (12.8) |
| <0.001 | <0.001 | ||||
| P* | 0.527 | 0.009 | |||
| d4105 Bending | 109 (100) | 80 (73.4) | 73 (67.0) | 54 (49.5) | 29 (26.6) |
| <0.001 | 0.001 | ||||
| P* | 0.262 | <0.001 | |||
| d4106 Shifting the body’s center of gravity | 109 (100) | 91 (83.5) | 82 (75.2) | 64 (58.7) | 40 (36.7) |
| <0.001 | 0.001 | ||||
| P* | 0.072 | <0.001 | |||
| d415 Maintaining a body position | 109 (100) | 48 (44.0) | 30 (27.5) | 23 (21.1) | 11 (10.1) |
| <0.001 | 0.001 | ||||
| P* | <0.001 | 0.003 | |||
| d420 Transferring oneself | 109 (100) | 71 (65.1) | 85 (78.0) | 61 (56.0) | 55 (50.5) |
| <0.001 | 0.001 | ||||
| P* | 0.004 | 0.18 | |||
Table 10: Distributions of the subjects according to limitations in mobility.
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | ||
| on admission | at discharge | on admission | at discharge | ||
| d4600 Moving within the home | 109 (100) | 97 (89.9) | 75 (68.8) | 59 (54.1) | 21 (19.3) |
| 0.001 | <0.001 | ||||
| P* | <0.001 | <0.001 | |||
| d4601 Moving around within buildings other than home | 109 (100) | 97 (89.0) | 87 (79.9) | 64 (58.7) | 42 (38.5) |
| 0.001 | <0.001 | ||||
| P* | <0.001 | <0.001 | |||
| d4602 Moving around outside the home and other buildings | 109 (100) | 103 (94.5) | 92 (84.4) | 86 (78.0) | 53 (48.4) |
| 0.014 | 0.008 | ||||
| P* | 0.005 | <0.001 | |||
| d465 Moving around using equipment | 109 (100) | 86 (78.9) | 64 (58.7) | 51 (46.8) | 28 (25.7) |
| <0.001 | 0.001 | ||||
| P* | <0.001 | <0.001 | |||
Table 11: The distribution of subjects according to limitations in moving around.
The greatest improvement was documented in subjects’ ability to use communication devices and techniques (d360) and in the longterm period, the overwhelming majority (98.2%) of the subjects did not have limitations in this ability (p<0.001) (Figure 2).
On admission to the primary rehabilitation program, more than 90% of subjects had limitations in self-care, household activities, and participation in recreation and leisure activities. Self-care skills significantly improved during rehabilitation programs (p<0.001) and least limitations were documented in the long-term period (p<0.05). The severe difficulties of household activities and participation in recreation and leisure activities significantly decreased during the primary inpatient rehabilitation program (p<0.001); however, the biggest improvement in these activities was determined during the rehabilitation inpatient program and especially improved in the longterm period (p<0.001) (Table 12).
| ICF category | Primary rehabilitation program (n=109) | Re-rehabilitation program (n=109) | Long-term period (n=109) | ||
| on admission | at discharge | on admission | at discharge | ||
| d510 Washing oneself | 109 (100) | 105 (96.3) | 93 (85.3) | 91 (84.0) | 46 (42.2) |
| 1 | 0.705 | ||||
| P* | 0.213 | 0.012 | |||
| d520 Caring for body parts | 109 (100) | 78 (73.2) | 54 (49.5) | 44 (40.4) | 8 (7.3) |
| <0.001 | 0.058 | ||||
| P* | 0.546 | <0.001 | |||
| d540 Dressing | 109 (100) | 93 (85.3) | 70 (64.2) | 54 (55.1) | 35 (32.1) |
| <0.001 | 0.002 | ||||
| P* | <0.001 | 0.001 | |||
| d550 Eating | 40 (40.4) | 30 (27.5) | 33 (30.3) | 25 (22.9) | 19 (17.4) |
| <0.001 | 0.005 | ||||
| P* | 0.439 | <0.001 | |||
| d620 Shopping | 109 (100) | 105 (96.3) | 91 (83.4) | 84 (77.1) | 58 (53.2) |
| 0.011 | <0.001 | ||||
| P* | 0.001 | <0.001 | |||
| d630 Preparing meals | 109 (100) | 101 (92.6) | 88 (80.7) | 79 (72.5) | 58 (53.2) |
| 0.101 | 0.001 | ||||
| P* | 0.235 | <0.001 | |||
| d640 Doing housework: washing, sweeping the floor | 109 (100) | 107 (98.1) | 94 (86.2) | 83 (76.1) | 65 (59.6) |
| 0.523 | 0.001 | ||||
| P* | 0.045 | <0.001 | |||
| d920 Participation in recreation and leisure activities (sports, arts, culture, etc.) | 105 (96.3) | 92 (84.4) | 72 (66.1) | 61 (56.0) | 27 (24.8) |
| 0.001 | 0.019 | ||||
| P* | 0.001 | <0.001 | |||
Table 12: Distribution of the subjects according to limitations in self-care, household and leisure activities.
Discussion
The results of our study are in line with the findings of other studies showing that SCI most frequently occurs in young, unmarried, male individuals who studied and actively sought to gain better education and participated in labor market. During the first 3 years after SCI, participants of our study actively participated in labor market, and during the long-term period, the portion of employed subjects increased by more than 2 times. In the long-term period, jobs at home dominated, and engagement in short-term jobs under fixed-term and works to order increased. Full-time jobs of mild or very mild intensity dominated, though the percentage of people having jobs of average intensity increased in the long-term period. Analysis of studies conducted in different countries has shown that there is a lack of consistent data about changes in employment status among people with SCI.
Some authors [13,28] state that the employment rate of people with SCI reaches 35%, while other authors report that during 20 years after SCI employment rates increase to 41% or 58%. Regardless of inconsistency in data published by different countries research, we can assume that persons with SCI are actively trying to participate in the labor market. Taking into account the overall situation of Lithuanian people with disabilities in the labor market, other studies conducted in Lithuania [4,29] and the results of our study, we advocate that the possibility to be employed is limited in this population, and due to currently existing socioeconomic situation in the country and relatively low job vacancies for disabled people, short-term, fixed-term, and home-based jobs dominate.
The analysis of changes in the FIM score in our study revealed that participation in the primary inpatient rehabilitation program significantly improved independence level and showed the largest increase in the mean FIM score. At the subsequent periods, the FIM score significantly increased, but in the long-term period, subjects reached the highest independence level (p<0.001). Decreasing functional skills after discharge from inpatient rehabilitation can be explained by decreased physical activity and lack of occupations and home environment adaptation; however, we found only one study by Hall et al. where the reduction of independence during the first year after discharge from medical rehabilitation due to the increased use of technical aids in everyday activities was reported. Comparing the functional independence level between subjects of different age, men and women we did not differ significantly. In addition, the analysis of functional independence in different long-term periods (<5 years, 5-10 years, and 10-15 years after SCI) showed that the more time passed after SCI, the greater was the change of mean FIM score: during<5 years after SCI, the FIM score was significantly lower than in 5-10 and 10-15 years after SCI. There are different opinions in literature, indicating the exact period during which the functional independence increased maximally. Some authors report that the functional independence level more increased only during inpatient rehabilitation and the highest level of independence is achieved in the first 3 years after SCI and in subsequent periods it does not change significantly [11,30]. Other authors who carried out longitudinal studies covering 15, 20, and 25 years after SCI state that independence is improving not only during medical rehabilitation, which is purposefully directed on reconstruction of functional skills, but also improved with every year after SCI naturally engaging in everyday life [13,31].
Analysis of changes of functioning showed that the majority of subjects had an increase in moderate self-confidence problems on admission to inpatient rehabilitation programs, although in the longterm period, these problems significantly decreased (p<0.005). Other authors also described similar tendencies in self-confidence problems during medical rehabilitation and 5 years after discharge [7].
In scientific literature, pain in different locations experienced by subjects with SCI during medical rehabilitation (b280), changes in pain intensity, pain-influencing factors during the sub-acute period after SCI, and health consequences and complications are widely analysed. We found that severity of pain in neck, back, and upper extremities significantly decreased during inpatient rehabilitation programs and in the long-term period only slight pain remained, except for pain in upper extremities and joints that significantly increased due to high physical workload such as moving in wheelchair resulting in pain in muscles, joint aches and tiredness.
In addition, we found that body weight maintenance (b530) dysfunctions significantly increased in the period between primary inpatient and re-rehabilitation programs and especially increased in the long-term period when 48.4% of the subjects had these problems. Tendencies in increasing overweight and obesity after rehabilitation have been noticed by other authors [32] who state that weight disorders interface not only with incorrect diet, but also decrease physical activity among people with SCI.
After SCI, the majority of subjects had severe dysfunctions of muscle functions and physical endurance, which did not improve during the inpatient rehabilitation program significantly, but the greatest improvement in physical endurance was observed in the longterm period. Recovery of muscle functions depends on SCI level and grade as well as health-related factors and is related to physical activity in daily life and maintaining participation in sports and domestic activities [7,9,19].
While analyzing activities and participation of subjects after SCI in various different situations of life, we detected the most frequently experienced difficulties in overcoming stress and other psychological problems (d240) were common at the beginning of inpatient rehabilitation programs, while participation in rehabilitation programs had a positive impact and led to significantly reduced challenges, and in the long-term period, these difficulties almost disappeared. Changes in psycho-emotional status of people with SCI observed during inpatient rehabilitation programs most commonly are associated with changes in health status, functional skills and adaptation to another life.
On admission to the inpatient rehabilitation program, 98.2% to 100.0% of the subjects had complete limitations in mobility, self-care, moving around in wheelchair in different locations, and participation in household and leisure activities. The positive impact of participation in inpatient rehabilitation programs was assessed for these actions: the biggest improvement in mobility and self-care, and significantly decreased limitations in moving around were documented. However, in the long-term period, mobility, self-care skills, and moving around improve by naturally engaging in daily life activities. Based on our results and similar studies conducted by other authors [12,17] we can suggest that during the inpatient rehabilitation program, functional skills and abilities, capacity, mobility and movements of people after SCI have purposefully been trained, and after discharge, the need to move around in various locations, when motor skills and physical capacity are naturally improving, naturally increases at home environment. Participation in domestic activities depends on natural prevailing possibilities to engage in these activities and abilities to use acquired skills; therefore, it is necessary during primary rehabilitation to start to improve household skills of persons with SCI in order to ensure their independence and skills at home. The biggest participation of our subjects in sports and leisure activities was documented in the longterm period when the difficulties in these activities decreased by almost 4 times.
However, some studies [23,27] have shown that participation and engagement in sports and recreational activities increases with every year after SCI, and too low participation in these activities is related to the limited opportunities of persons with disabilities in sports and employment, especially in smaller towns. Therefore, even during inpatient rehabilitation, it is important to encourage people after SCI to participate in sports and leisure activities by engaging in nongovernmental, sports organizations for the disabled.
Conclusions
Our study has shown that SCI most commonly occurred in young, aged about 34 years, men. The main causes of traumatic SCI were motor accidents, sports or diving into water, household injuries and falls from height. Even 43.1% of the subjects consumed alcohol within 6 hours before SCI.
The longitudinal study on changes in functional independence during different periods after SCI shows that participation in primary inpatient rehabilitation significantly improved the independence level and resulted in the greatest increase in the mean FIM score. In subsequent periods, i.e., 1-10 years after SCI, the functional independence level significantly increased, but later did not change significantly and remained stable. Decreasing functional skills after discharge from inpatient rehabilitation can be explained by decreased physical activity or lack of occupations. Comparison of the independence level between subjects of different age and sex showed no significant differences.
Comprehensive inpatient rehabilitation programs are effective and significantly improve patients’ functioning: decrease severe body dysfunctions and participation limitation in daily life. In the longterm period, the highest improvement in muscle function, physical endurance, ability to move around, participation in household, and leisure activities was recorded; however, pain in upper extremities or joints and body weight support dysfunctions significantly increased.
Acknowledgements
The study was founded by the Department of Rehabilitation, Physical and Sports medicine, the Medical Faculty, Vilnius University, and the Center of Rehabilitation, Physical and Sports Medicine, Vilnius University Hospital Santaros Clinics. The data in the long-term period are based on work supported by Lithuania Paraplegic Association, in ‘Landscape Therapy and Recreation Centre’ Palanga, Lithuania.
References
- National Spinal Cord Injury Statistical Centre, Facts and Figures at a Glance (2016) Birmingham AL: University of Alabama at Birmingham.
- World Health Organization (WHO) – Media Centre: Spinal Cord Injury.
- Drigotaite N, Krisciunas A (2006) Complications after spinal cord injuries and their influence on the effectiveness of rehabilitation. Medicina (Kaunas) 42: 877-880.
- Juocevicius A, Butenaite L (2010) Spinal cord injury peculiarities in Lithuanian patients in 1994–2008. Gerontology 11: 95-102.
- SpinalCord.com. Available from: http://www.spinalcord.com/life-after-a-spinal-cord-injury
- Brinkhof MW, Fekete C, Chamberlain JD, Post MW, Gemperli A, et al. (2016) Swiss national community survey on functioning after spinal cord injury: Protocol, characteristics of participants and determinants of non-response. J Rehabil Med 48: 120-130.
- Oliver M, Inaba K, Tang A, Branco BC, Barmparas G, et al. (2012) The changing epidemiology of spinal trauma: A 13-year review from a Level I trauma centre. Injury 43: 1296-1300.
- Butenaite L (2014) The mathematical model of evaluation of functional independence, body functions, activities and participation peculiarities of people with SCI. Vilnius: Vilnius University.
- Rahimi-Movaghar V, Sayyah MK, Akbari H, Khorramirouz R, Rasouli MR, et al. (2013) Epidemiology of traumatic spinal cord injury in developing countries: A systematic review. Neuroepidemiology 41: 65-85.
- Anderson K, Aito S, Atkins M, Biering-Sørensen F, Charlifue S, et al. (2008) Functional recovery measures for spinal cord injury: An evidence-based review for clinical practice and research. J Spinal Cord Med 31: 133-144.
- van Leeuwen CM, Post MW, Westers P, van der Woude LH, de Groot S, et al. (2012) Relationships between activities, participation, personal factors, mental health, and life satisfaction in persons with spinal cord injury. Arch Phys Med Rehabil 93: 82-89.
- Krause JS, Bozard JL (2012) Natural course of life changes after spinal cord injury: A 35-year longitudinal study. Spinal Cord 50: 227-231.
- Carpenter C, Forwell SJ, Jongbloed LE, Backman CL (2007) Community participation after spinal cord injury. Arch Phys Med Rehabil 88: 427-433.
- Lidal IB, Hjeltnes N, Røislien J, Stanghelle JK, Biering-Sørensen F (2009) Employment of persons with spinal cord lesions injured more than 20 years ago. Disabil Rehabil 31: 2174-2184.
- Müller R, Peter C, Cieza A, Geyh S (2012) The role of social support and social skills in people with spinal cord injury-A systematic review of the literature. Spinal Cord 50: 94-106.
- Post MW, Kirchberger I, Scheuringer M, Wollaars MM, Geyh S (2010) Outcome parameters in spinal cord injury research: A systematic review using the International Classification of Functioning, Disability and Health (ICF) as a reference. Spinal Cord 48: 522-528.
- Silver J, Ljungberg I, Libin A, Groah S (2012) Barriers for individuals with spinal cord injury returning to the community: a preliminary classification. Disabil Health J 5: 190-196.
- Haas B, Playford ED, Ahmad AQ, Yildiran T et al. (2016) Rehabilitation goals of people with spinal cord injuries can be classified against the International Classification of Functioning, Disability and Health Core Set for spinal cord injuries. Spinal Cord 54: 324-328.
- Furlan JC, Noonan V, Singh A, Fehlings MG (2011) Assessment of disability in patients with acute traumatic spinal cord injury: A systematic review of the literature. J Neurotrauma 28: 1413-1430.
- de Groot S, van der Woude LH, Niezen A, Smit CA, Post MW (2010) Evaluation of the physical activity scale for individuals with physical disabilities in people with spinal cord injury. Spinal Cord 48: 542-547.
- Skucas K, Mockeviciene D (2009) Factors influencing the quality of life of persons with spinal cord injury. Spec Education 21: 35-42.
- van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, et al. (2008) A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil 89: 2094-2101.
- Sale P, Mazzarella F, Pagliacci MC, Aito S, Agosti M, et al. (2012) Sport, free time and hobbies in people with spinal cord injury. Spinal Cord 50: 452-456.
- Martin Ginis KA, Jetha A, Mack DE, Hetz S (2010) Physical activity and subjective well-being among people with spinal cord injury: A meta-analysis. Spinal Cord 48: 65-72.
- Guest R, Craig A, Tran Y, Middleton J (2015) Factors predicting resilience in people with spinal cord injury during transition from inpatient rehabilitation to the community. Spinal Cord 53: 682-686.
- Kerstin W, Gabriele B, Richard L (2006) What promotes physical activity after spinal cord injury? An interview study from a patient perspective. Disabil Rehabil 28: 481-488.
- Ottomanelli L, Barnett SD, Goetz LL (2014) Effectiveness of supported employment for veterans with spinal cord injury: 2-year results. Arch Phys Med Rehabil 95: 784-790.
- Okuneviciute NL, Kavaliauskaite R, Žemaitaityte G (2012) I do not understand the situation in the labor market. Environmental adaptation for negative needs. Vilnius.
- Amsters DI, Pershouse KJ, Price GL, Kendall MB (2005) Long duration spinal cord injury: Perceptions of functional change over time. Disabil Rehabil 27: 489-497.
- Rehabilitation Measures Database (2015) FIM® instrument (FIM); FIM® is a trademark of the Uniform Data System for Medical Rehabilitation, a division of UB Foundation Activities.
- Crane DA, Little JW, Burns SP (2011) Weight gain following spinal cord injury: A pilot study. J Spinal Cord Med 34: 227-232.
Citation: Adomavičienė A, Šidlauskienė A, Raistenskis J (2017) Recovery of Biopsychosocial Functions Following 15 Years after Spinal Cord Injury. Occup Med Health Aff 5:264. DOI: 10.4172/2329-6879.1000264
Copyright: © 2017 Adomavičienė A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3108
- [From(publication date): 0-2017 - Dec 04, 2024]
- Breakdown by view type
- HTML page views: 2478
- PDF downloads: 630