Readmission and Penalty- Saving Analysis for Rural Areas Hospitals through Remote Patient Monitoring. A Case Study of St Peters Hospital, St Vincent, and Benefis Hospitals
Received: 01-Mar-2023 / Manuscript No. omha-23-90329 / Editor assigned: 04-Mar-2023 / PreQC No. omha-23-90329 / Reviewed: 17-Mar-2023 / QC No. omha-23-90329 / Revised: 24-Mar-2023 / Manuscript No. omha-23-90329 / Published Date: 30-Mar-2023 DOI: 10.4172/2329-6879.1000459
Abstract
According to Association of American Medical Colleges, Rural American make up at least 15 to 20% of the U.S. population face inequities that result in worse health care than that of urban and suburban residents. Most of the rural healthcare facilities can now switch to RPM for them to be saved from CMS penalties if hospitals provide free broad band internet service. GPA will convince the hospitals to invest on broad band internet to be able to connect with patients living in rural areas more efficiently and have better access to healthcare through remote patient monitoring. GPA has reached out to an accountable care organization that have provided enough data showing the effectiveness of RPM on Heart failure patient’s readmission rates in rural areas hospitals. GPA aim to use remote patient monitoring based on modern technology to collect data and help heart failure patients manage their health without visiting the healthcare setting in rural areas.
Keywords
RPM; CMS Penalties; GPA; Rural Healthcare programs
Definition of Terms
GPA- (Griffin Population Analytic)
RPM- (remote patient monitoring)
CMS- Center for Medicare and Medicaid
FCC-Federal Communications Commission
Chapter One: Introduction
Background of the study
The need to improve health outcomes and improve the quality of healthcare has called hospitals to turn to using telecommunication technologies. We are in the era where healthcare services are delivered through videoconferencing, remote monitoring, electronic consults, and wireless communication. One of the widely used technologies in the healthcare sector is the Remote Patient Monitoring. According to Klein, remote patient monitoring entails the use of technological devices such as wearable heart monitors, Bluetooth enabled scales, glucose monitors, and maternity care trackers to diagnose and monitor patients. Remote patient monitoring has become of the most used programs to deliver quality healthcare even in the remote areas. Remote patient monitoring present numerous benefits to healthcare providers and the patients including; improving the quality of healthcare, reducing the cost of healthcare, it gives the patients the peace of mind and daily assurance, and it enables physicians to provide more support to the patients and give constant feedback to the patients about their conditions. Additionally, RPM saves time of the patients as the patients do not have to visit the hospitals every time for diagnosis and examination.
The use of technology to connect with the patients remotely is gaining momentum in the US report that over 50% of U.S hospitals examine patients through the use of video conferencing or other technology tools. However, many patients cannot take the advantage of RPM due to lack of internet connectivity. Tuckson et al. report that 40% of the American population lives in the rural areas and a significant percentage of the criticized are not connected to the broadband internet. There has been high prevalence of chronic conditions in the United States and the cases are predicted to increase by 2020. Klein, reports that, 51% of US adult population is living with at least one chronic condition and 27% have multiple chronic conditions such as chronic obstructive pulmonary disease (COPD), cancer, and stroke and this number is expected to grow by half by 2030.
The chronic conditions have been among the leading causes of readmissions to hospitals and Heart Failure (HF) has been one of the leading causes of readmissions in hospitals. Many hospitals have reduced the HF readmissions significantly by the use of remote patient monitoring. Almost every other Medicaid program has some form of coverage for telehealth services and the private payers are enjoying the coverage for many telehealth services. However, other hospitals especially those in the remote areas cannot monitor heart failure patients through RPM because most of the patients are not connected to the broadband internet.
It is a major challenge for most of the rural hospitals to do constant follow-up for all discharged HF patients since the patients do not have internet connection at home. This limits the implementation of remote patient monitoring to which can yield good results in reducing readmission rates and save hospitals from CMS penalties. It is disheartening to note that many hospitals are registering high rates of readmissions within thirty days of discharge and hence are penalized heavily by CMS. The failure by rural hospitals to use technology to monitor the HF patients has increased the cases of readmissions within thirty days of discharge. The increased HF readmissions have increased the penalties charged by Centre for Medicaid & Medicare to the hospitals for the failure to keep the readmissions down. According to Federal Communication Commission, the US wants to increase the internet coverage to at least 80% of the population by 2030. However, this may take longer and many hospitals will be continue to penalized heavily by CMS for failure to use appropriate programs such as RPM to chronic patients readmissions that occur within 30 days of discharge. One of the most brilliant ideas which can be utilized by rural hospitals to increase the use of RPM is by paying the broadband internet for the discharged patients to help reduce readmissions. The challenge is whether the hospitals can make enough savings from the reduced readmissions to pay for satellite internet for the discharged rural patients.
Statement of the problem
Technology is changing the way healthcare is delivered. Remote patient monitoring is becoming an option for many hospitals to do value-based care for their patients. This is made possible by technology since connecting with patients and sharing information is quite very efficient. Nevertheless, there is huge gap in broadband access in most of the rural areas in the United States. According to Association of American Medical Colleges, at least 20% of the U.S. population live in rural areas and face inequities that result in worse health care than that of urban and suburban residents and the one of the inequalities is the digital divide whereby most the rural citizens are not connected to the broadband internet. The FCC’s Rural Health Care Program supports broadband adoption, but it is administratively burdensome and provides an insufficient level of subsidy for remote health care providers. This limits them from implementing effective RPM programs.
The failure to use digital technologies makes it difficult for rural hospitals to do effective follow up for all patients discharged from the hospitals and this results to high readmission rate within 30 days of discharge a situation that is highly penalized by CMS. Under programs set up by the Affordable Care Act, the federal penalizes hospitals that have high rates of readmissions and those with the highest numbers of infections and patient injuries. Medicare penalizes hospitals up to three percent for each patient readmitted within 30 days of discharge.
Heart Failure is among the leading causes of readmissions for the hospitals and using RPM can help the hospitals to reduce the readmissions significantly [1]. GPA seeks to study on whether hospitals can register significant reductions in readmissions enough cater for internet expenses if the hospitals pay for broadband internet for the remote HF patients in RPM program. The study will focus on three rural hospitals in Montana which usually register high levels of readmissions within thirty days of discharge of chronic hence ending up being penalized by CMS. The three hospitals include; St Peters Hospitals, St Vincent Hospital, and Benefis Hospital.
Research Hypothesis
The hypothesis is of this study is that if the hospitals pay for internet connection to support RPM in homes of rural HF patients, the hospitals will register enough readmission reduction enabling the hospitals to make significant savings on CMS penalties be enough to pay cater for the cost of internet services [2].
Research Questions
This research seeks to answer the following questions. Can hospitals reduce HF readmissions by implementing RPM?
Can hospitals reduce CMS penalties by paying satellite broadband internet for rural HF patients on RPM?
Is it financially viable for hospitals to pay for broadband internet for rural HF patients on RPM?
Scope of the study
The study will focus on rural hospitals that register high CMS penalties every year due to high levels of readmissions on HF patients that occur within 30 days of discharge [3]. The main agenda of the study will be to show the hospitals how to save through reduction of HF patient’s readmission rate through paying for broadband internet in HF patients’ homes to facilitate the remote patient monitoring program. Paying for the broadband internet for the HF patients will enable the hospitals to follow up and monitor the discharged patients closely through RPM program hence enabling the hospitals to reduce the rate of readmissions. The reduction in readmissions will enable the hospitals to make enough savings to pay for the broadband internet [4].
Significance of the study
GPA penalty-saving analysis model will demonstrate how paying for broadband by hospitals in rural areas can lead to reduction of readmission rate and yield in decreased Medicare penalization for Heart failure in hospitals located in rural areas in the United States.
Limitation of the Study
The data analysis will be based on unpublished work due to lack of enough literature in the topic of the study.
Chapter Two: Literature Review
Introduction
The use of digital technologies to collect medical and other forms of data from individuals from one location and transmit the data electronically to healthcare professionals in other locations for assessment and recommendations is a growing field that has been widely accepted [5]. According to Klein, 60% of the patients feel RPM is safe and are ready to be monitored remotely from their homes. However, some patients still have the notion that being examined through telecommunication devices is not as effective as an examination on one-one basis. Other patients believe that RPM services increases the healthcare costs. However, this myth has been disqualified by the several studies that have been conducted to determine the benefits of using Remote Patient Monitoring program. According to Meyer (2011), RPM improves patient engagement and health outcomes hence thereby reducing readmissions and lowering healthcare cost. Meyer reports that Remote patient monitoring can improve the health outcomes of six in every ten patients and therefore it is a program worth to invest in.
Malasinghe et al. argue that the RPM technologies are user friendly and cost effective and hospitals should implement them to improve the patients’ outcomes and to save significant costs. Many hospitals are turning to RPM to reduce the high rates of hospital readmissions and reduce the high CMS penalties that arise as a result of high hospitals readmissions that occur within 30 days of discharge. According to Hjelm CMS readmission penalties and length of stay are the key contributors to the high increased hospital bills. Healthcare spending has increased by 4.2% between 2016 and 2017 to $ 3.5 trillion or what is termed as $ 10,730 per person. In 2016, there were over 35 million hospitals stays which amounted to 104.2 stays per 100, 000 population. Nevertheless, the average cost per hospital stay was $ 11,700 making hospitalization one of the most expensive types of healthcare utilization. In 2017, the aggregate hospital costs for 35.8 million hospital stays totaled $ 434.2 billion [6]. The reported statistics are discouraging but the spending by hospitals can be brought down significant if hospitals embrace remote patient monitoring.
Interestingly, the new healthcare legislation allows physicians to bill for the service. CMS covers the RPM services under the following CPT codes; 99453, 99454, 99457 and 99458. The CPT code 99453 covers initial set of RPM services and patient education, and CPT code 99454 covers supply of devices and collection, transmission, and summary the services. On the other hand, the CPT code 99457 covers the first 20 minutes of remote physiologic monitoring by clinical staff whereas CPT codes 99458 covers additional 20 minutes of remote physiologic monitoring by clinical staff above the 20 minutes covered by CPT 99457 (CMS, 2020). Importance of RPM after Discharge of HF Patients
Many scholars have researched to determine whether monitoring heart failure patients through remote monitoring program that can have any significant impacts on discharged patients. One of the studies which sought to determine the effectiveness of RPM after discharge of hospitalized HF patients was conducted by Ong et al. The authors monitored 737 patients out sample size of 1437 HF patients for 180 days on RPM after the patient were discharged from different hospitals. The other 700 patients were not put under any RPM program. The patients under the RPM program were monitored through mobile phones were the physicians collected data weekly on the progress of the patients and advised the patients according on to manage the situation. Readmissions were reported on the patient in the RPM programs and those not in the RPM and therefore the scholars concluded that RPM do not have significant impact in reducing readmissions after discharge for the HF patients [7].
Hale at al. also sought to determine whether monitoring HF patients under the RPM can help to reduce hospitals readmissions. The scholars compared Med Sentry remote patient monitoring and usual in older HF patients. The scholars found that the use of RPM reduced the all risks including lack of medical adherence that caused hospitalizations after discharges. Hale et al. concluded that, Med sentry hospital monitoring system was effective in reducing readmissions and recommended the use of RPM programs to improve health outcomes and to ensure quality care to the HF patients.
Another study to show the effectiveness of RPM was conducted by Mount Sinai Hospital. The hospital put 380 patients on specialized care from September 2015 to June 2018 to compare their rates of readmissions. Among these patients, 28 HF patients were put on RPM program. The hospital noted that the 30-day readmissions for the HF patients reduced from 22% to 9%, which represent a 40% reduction [8]. This shows the monitoring HF patients through RPM program cam help to lower the readmissions rate after hospitals significant hence avoiding the CMS penalties that can arise due to high rates of readmissions after 30 days of discharges (CMS, 2020).
The Digital Divide in United States
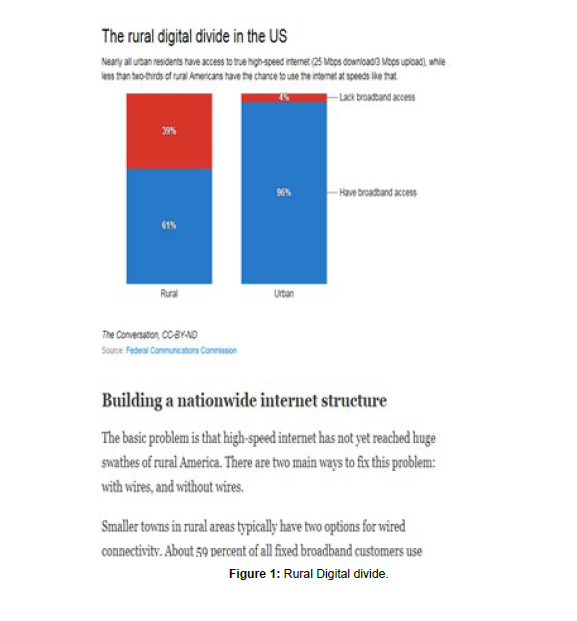
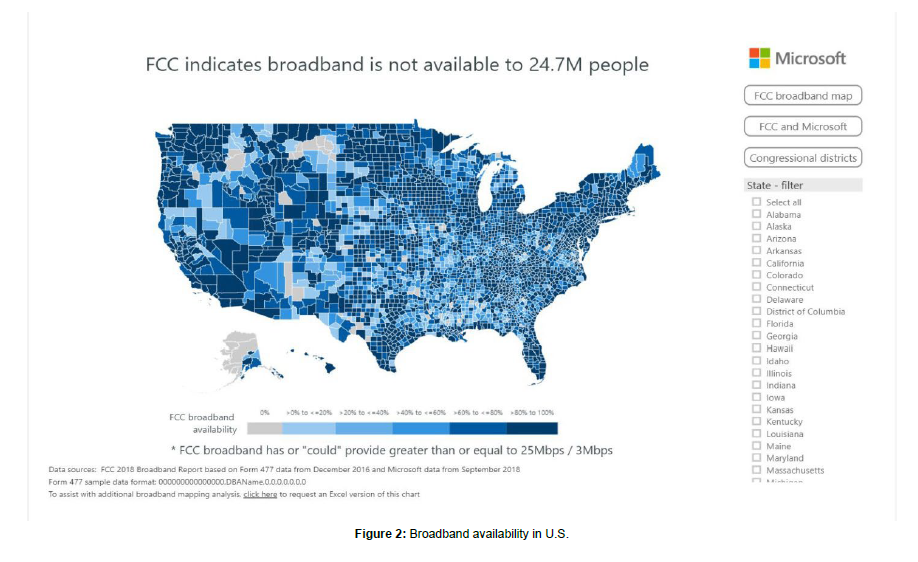
United States strangles to reduce the big digital divide across the country. There is a large population who has no broadband internet connectivity which Federal Communication Commission estimates to be more than by 20 million people. According to FCC, 39% of rural dwellers lack broadband access which is relatively an extremely high number compared to 4% of urban Americans The rural areas account for the largest percentage of the areas that are not connected to the broadband internet and this is devastating since the rural populations are denied to enjoy the fruits of internet connectivity and modern technology. For instance, the rural population cannot receive healthcare services remotely through technological devices due to lack of internet connectivity to facilitate the process. Rural residents have few choices of internet services providers or none. Those internet providers available charge higher prices for very lower quality services. This explains why only few rural Americans use internet to get services online or do their activities remotely compared to urban residents (FCC, 2020) [9].
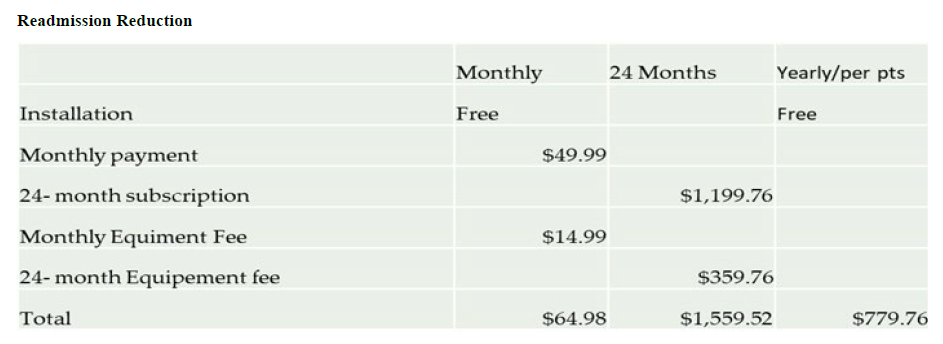
The increasing use of remote patient monitoring and other types of telehealth services is increasing the urgent to have internet connectivity in the rural areas. However, due to lack of broadband internet connectivity in the rural areas, the hospitals and patients are turning to private internet providers to get internet connectivity. The Satellite broadband is one of the most widely available type of internet delivery in the U.S. Satellite broadband is one way to get to get internet delivery anywhere in the rural areas. The most widely satellite provider recognized by Federal communications commission is HughestNet whose download speed 150% faster than the other providers and upload speed is about 200% better than the other satellite broadband internet providers. Nevertheless, the installation and the monthly subscriptions can cost the rural hospitals and the patients significant amount money. Comparatively, HughestNet is averagely cheaper and efficient as the installation is free and the monthly subscription is $ 4.99 per month. Figure one shows the rural digital divide in the US whereas figure 2 shows the broadband internet connectivity in all US states [figure 1,2].
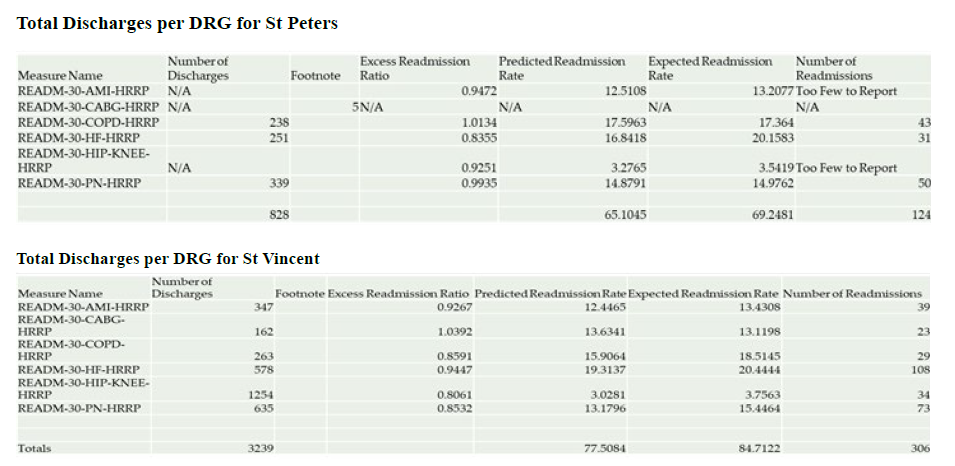
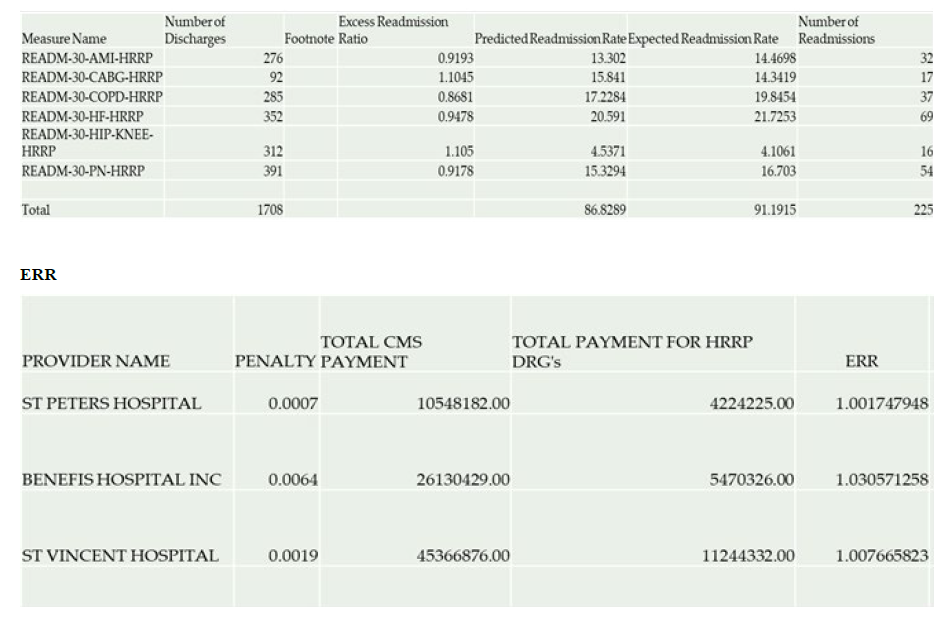
Research design and methodology
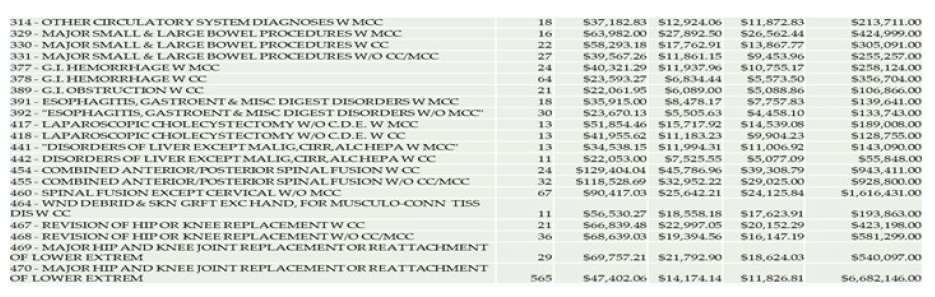
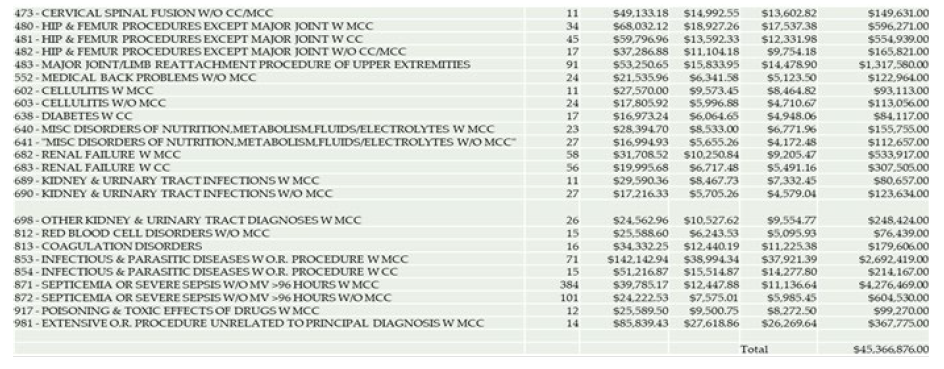
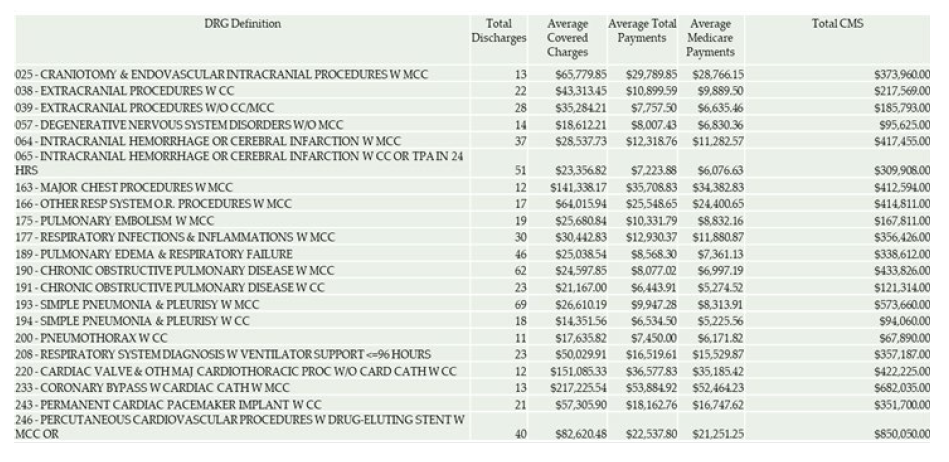
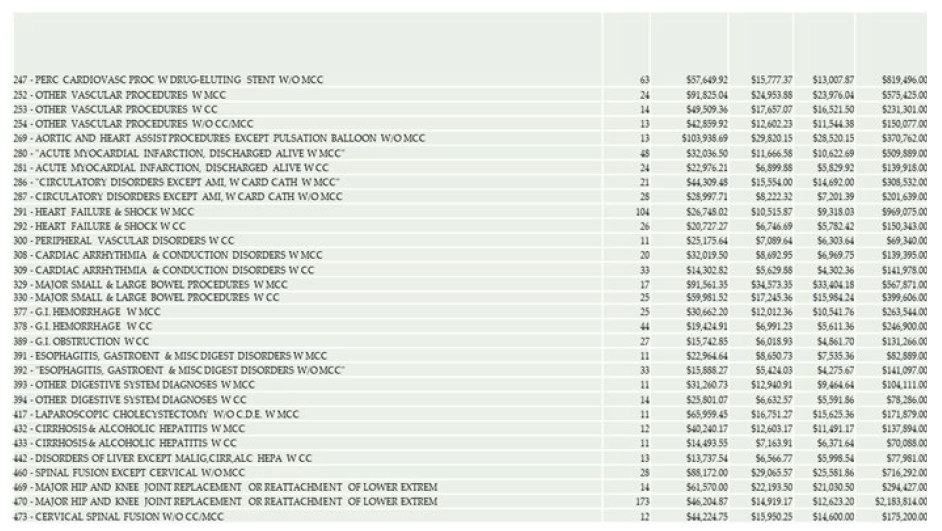
Quantitative data was collected from Center for Medicaid & Medicare services database, Hospital Readmission Reduction Program. These data include the number of discharges and readmissions patients with the 6 DRGs including Heart Failure. Data on penalties on three hospitals was collected and calculated using the payment adjustment factor. Descriptive design was the most appropriate for Saving Cost Analysis. The significance of the descriptive research design made it possible to integrate the quantitative and qualitative methods of data collection.
Data Collection
Hospital readmissions reduction program (HRRP)
• CMS calculates the payment reduction and component results for each hospital based on its performance during a rolling three-year performance period.
• The payment adjustment factor is the form of the payment reduction CMS uses to reduce hospital payments.
• Payment reductions are applied to all Medicare fee-forservice base operating diagnosis-related group payments during the FY (October 1 to September 30).
• The payment reduction is capped at 3 percent (that is, a payment adjustment factor of 0.97).
• All the calculations are based on the unpublished model developed by Zupec J. and Lucado G [10].
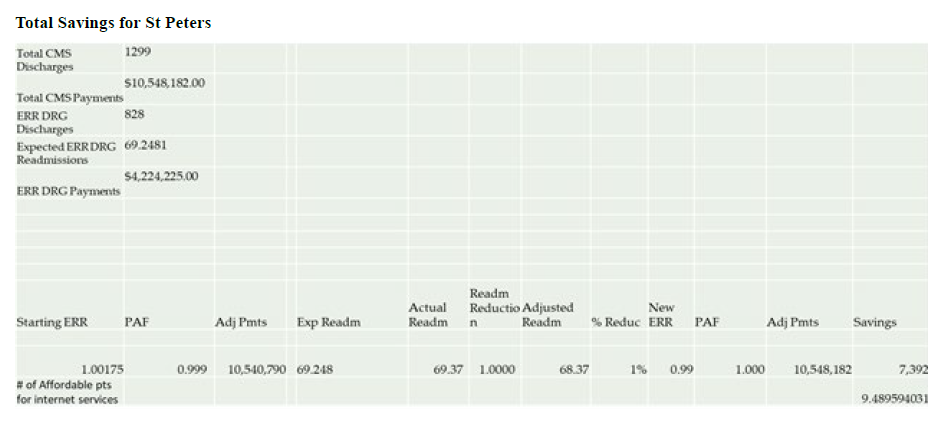
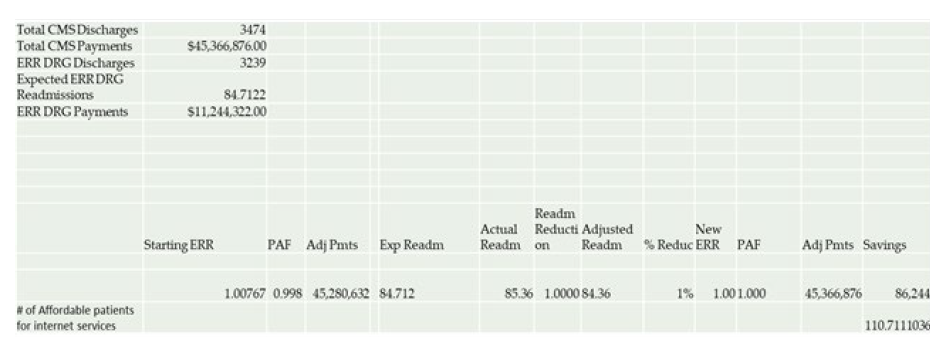
Chapter Four: Data Analysis
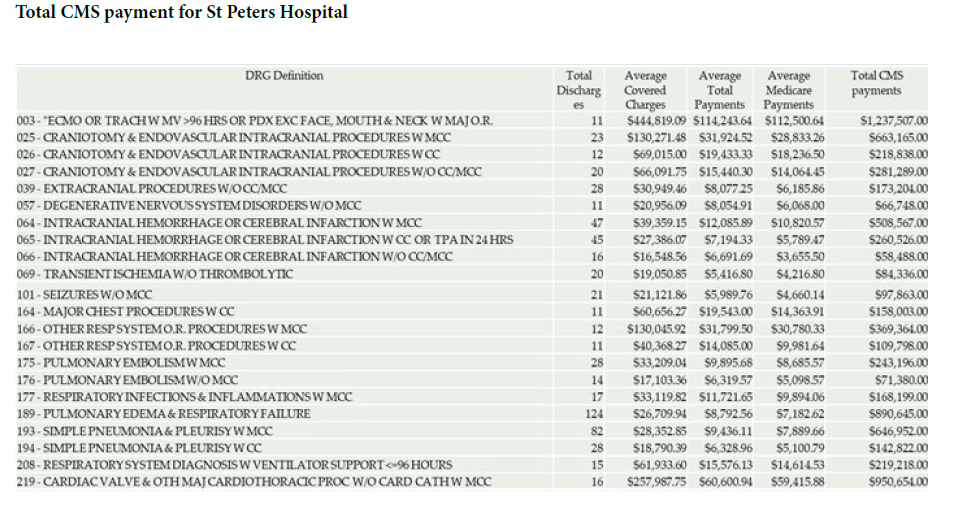
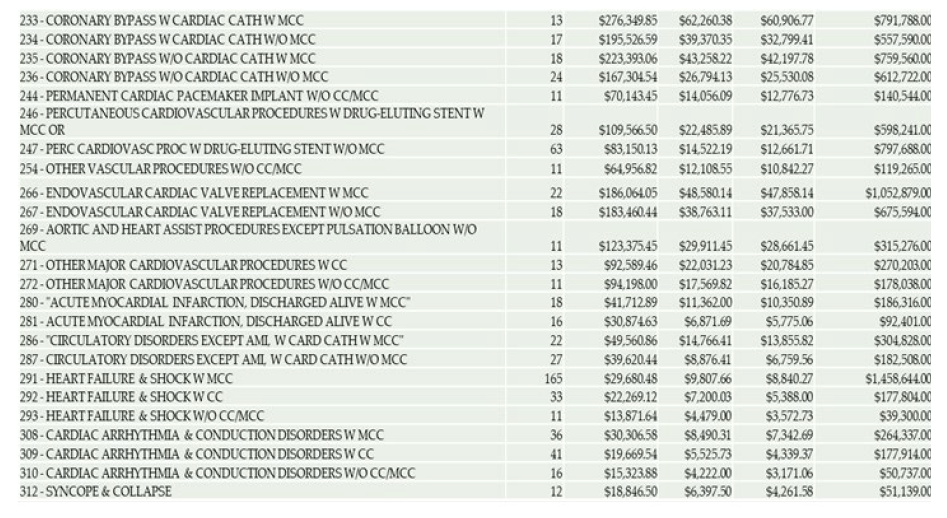
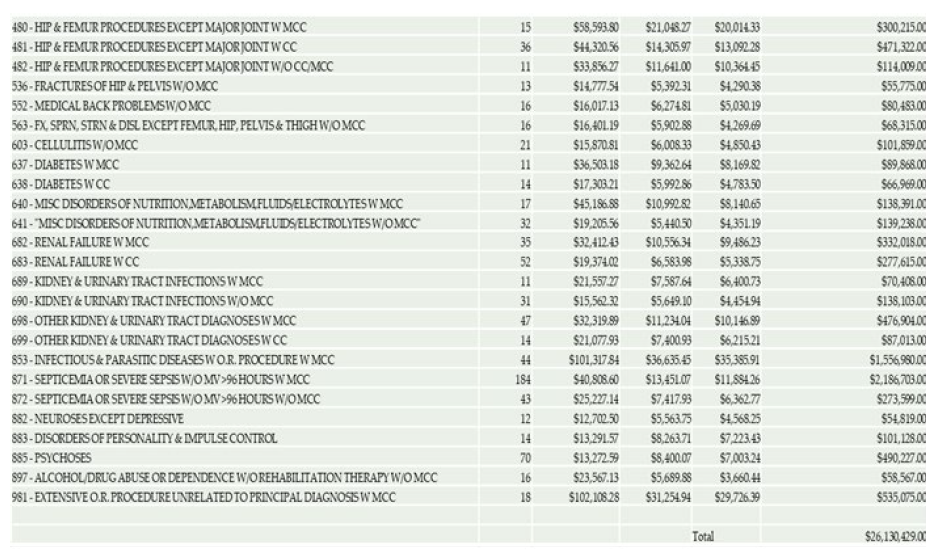
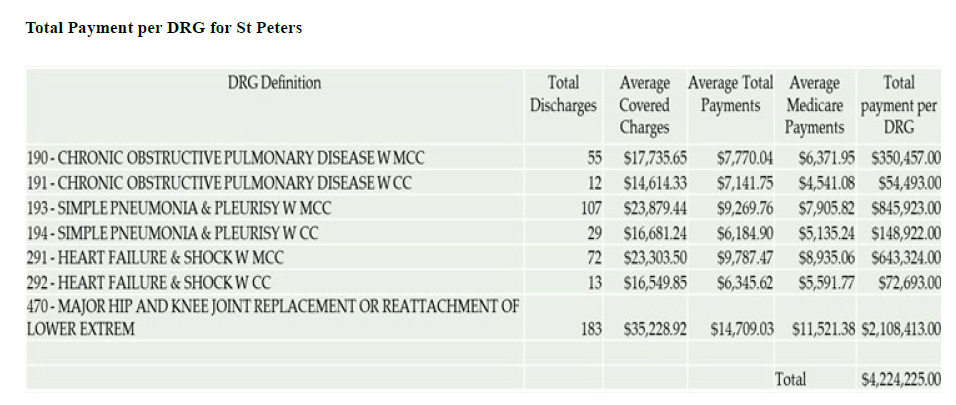
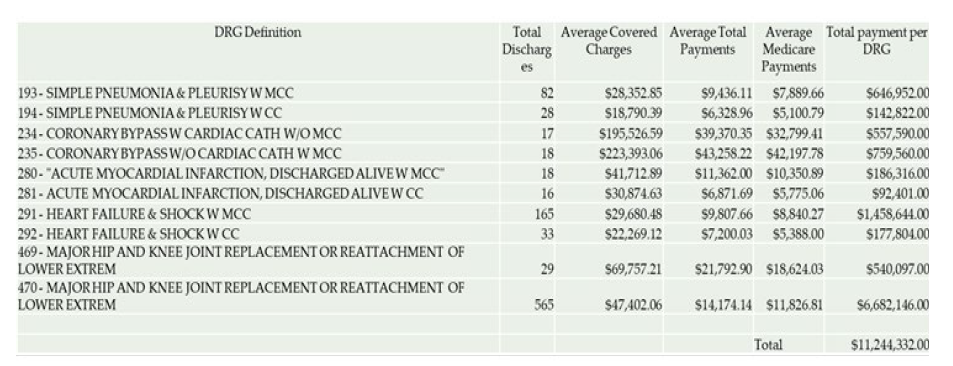
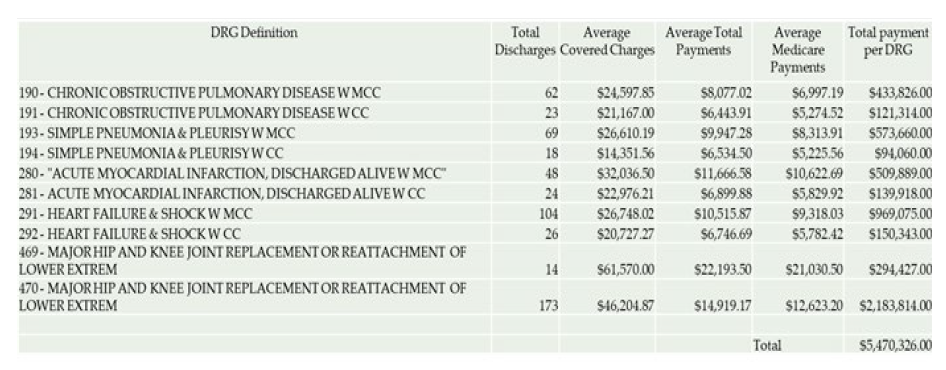
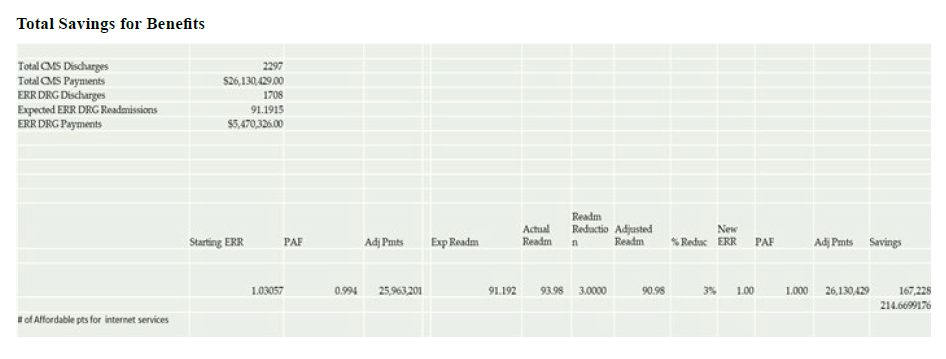
From the model the number of patients the hospitals can afford to pay internet for are as follows. Benefis- 214, St Peters-9, and St Vincent-111. The hospitals will report the following HF readmissions if they do not implement RPM; Benefis-13, St Peters- 1 and St vincent-4 [11-15].The hospitals will report the following readmissions if they put the HF patients on RPM; Benefis- 5, St Peters- 0, and St vincent- 2Therefore, the reduced number of readmissions for the three hospitals is as follows; Benefits- 8 (13-5), and St Vincent- 2 (4-2).
This means that Benefits and St Vincent will make enough savings from reduced readmissions to pay for the broad band internet for the rural HF patients who cannot take advantage of RPM due to lack of internet connection. This is because the hospital’s reduced readmission is more than the number of readmissions required to generate maximum savings for the hospitals. However, the model cannot work for St. Peters since the hospitals savings on readmissions is too low therefore the hospital cannot only afford to pay internet for a few HF patients which cannot support enough reductions in readmission to generate the cost for internet [16-18] [Table 1].
| HughestNet | Variable | Viasat |
|---|---|---|
| $ 49.99-$ 129.99 | Monthly Price | $ 50-$ 100 |
| 25Mbps | Download speed | 12 Mbps |
| 3mbps | Upload speed | 3Mbps |
| 10 GB-50GB | Data Cap | 12GB-50GB |
| 24-month | Contract requirement | 24-month with a 2 year price lock |
| Free standard installation | Installation | Free standard installation |
| $ 14.99 | Monthly equipment fee | $10/month |
| $ 15/every remaining contract month | Early termination fee | $ 15/every remaining contract month |
| Nationwide | Availability | Nationwide |
Recommendation and Conclusion
The results from the study illustrates that hospitals will register reduced HF readmissions if they pay broad band internet for rural patients who cannot take advantage of RPM due to lack of internet connections. This will make the hospitals to make significant savings from HF readmission penalties which will are enough to pay for the broad band internet. Therefore, paying internet for rural HF patients who cannot afford RPM due to lack of internet connectivity is viable for St Vincent, Benefis.
Declaration
I declare that this study is my original work, and it has not been submitted to any university for any degree or professional qualification.
Acknowledgement
It is a great honor for those who made this study successful. My professor Frederick Lucado, who has gladly shared his expertise, commitment, and guidance during this study. I therefore gratefully appreciate my parents and all family members for their moral and cordial support to ensure success of the project. Also acknowledge our colleagues and friends for their support during my course and the entire university fraternity for resource provision.
References
- Bauer UE, Briss PA, Goodman RA, Bowman BA (2014) Prevention of chronic disease in the 21st century: elimination of the leading preventable causes of premature death and disability in the USA.Lancet 384: 45-52.
- Broderick A, Steinmetz V (2013) Centura Health at Home: Home telehealth as the standard of care.Commonwealth Fund.
- Brown SJ (2012)U.S. Patent No. 8,249,894. Washington, DC: U.S. Patent and Trademark Office.
- Cheng AC, Levy MA (2016) Data driven approach to burden of treatment measurement: A study of patients with breast cancer. InAMIA Annual Symposium Proceedings17-56.
- Data retrieved from GPA throughvivifyhealth.com
- Data retrieved from GPA through Caravanhealth.com
- FCC (2020) Broadband Deployment Report. Retrieved
- Hjelm NM (2005) Benefits and drawbacks of telemedicine.J Telemed Telecare 11:60-70.
- Hale TM, Jethwani K, Kandola MS, Saldana F, Kvedar JC (2016) A remote medication monitoring system for chronic heart failure patients to reduce readmissions: a two-arm randomized pilot study.Journal of medical Internet research 18: 91.
- Klein S (2011) Hospital at home” programs improve outcomes, lower costs but face resistance from providers and payers.Report the Commonwealth Fund. USA
- Malasinghe LP, Ramzan N, Dahal K (2019) Remote patient monitoring: a comprehensive study.Telemed J E Health 10: 57-76.
- Mount Sinai Hospital (2018) Remote Monitoring Improves Readmission Rates for Heart Failure Patients
- Meyer H (2011) At UPMC, improving care processes to serve patients better and cut costs.Health Affairs30: 400-403.
- O'Gorman LD, Hogenbirk JC, Warry W (2016) Clinical telemedicine utilization in Ontario over the Ontario telemedicine network.Telemedicine and e-Health22: 473-479.
- Ong MK, Romano PS, Edgington S, Aronow HU, Auerbach AD (2016) Effectiveness of remote patient monitoring after discharge of hospitalized patients with heart failure: the better effectiveness after transition–heart failure (BEAT-HF) randomized clinical trial.JAMA internal medicine 176: 310-318.
- Peretz D, Arnaert A, Ponzoni NN (2018) Determining the cost of implementing and operating a remote patient monitoring program for the elderly with chronic conditions: A systematic review of economic evaluations.J Telemed Telecare 24:13-21.
- Tuckson RV, Edmunds M, Hodgkins ML (2017) Telehealth.N Engl J Med377: 1585-1592.
- Vegesna A, Tran M, Angelaccio M, Arcona S (2017) Remote patient monitoring via non-invasive digital technologies: a systematic review.Telemed J E Health 23: 3-17.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Lisa L (2023) Readmission and Penalty- Saving Analysis for Rural Areas Hospitals through Remote Patient Monitoring. A Case Study of St Peters Hospital, St Vincent, and Benefis Hospitals. Occup Med Health 11: 456. DOI: 10.4172/2329-6879.1000459
Copyright: © 2023 Lisa L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2271
- [From(publication date): 0-2023 - Sep 23, 2025]
- Breakdown by view type
- HTML page views: 1954
- PDF downloads: 317