Research Article Open Access
Rationale, Component Description and Pilot Evaluation of a Physical Health Promotion Measure for People with Mental Disorders across Europe
Prisca Weiser1, Reinhold Kilian1, David McDaid2, Loretta Berti3, Lorenzo Burti3, Peter Hjorth4, Katarzyna Lech5, Köksal Alptekin6, Elena Bonfioli3, Mojca Zvezdana Dernovsek7, Eva Dragomirecka8, Marion Freidl9, Fabian Friedrich9, Aneta Genova10, Arunas Germanavicius11, Povl Munk-Jørgensen12, Ramona Lucas-Carrasco13, Roxana Marginean14, Maya Mladenova10, A-La Park2, Alexandru Paziuc14, Petronela Paziuc14, Stefan Priebe15, Katarzyna Prot-Klinger16, Halis Ulas6, Carolin von Gottberg1, Johannes Wancata9, Thomas Becker1*1Ulm University, Department of Psychiatry II, BKH Günzburg, Germany
2PSSRU, London School of Economics and Political Science, United Kingdom
3Universitá degli Studi di Verona, Department of Public Health and Community Medicine, Italy
4Regionspsykiatrien Randers, Randers, Denmark
5Community Care Department, Wolski Hospital, Poland
6Dokuz Eylül Üniversitesi Tip Fakültesi Psykiyatri Anabilim Dali, Turkey
7Psychiatric Hospital, Slovenia
8Social Work Department Faculty of Arts, Charles University, Czech Republic
9Medical University of Vienna, Department of Psychiatry and Psychotherapy, Austria
10Fondatzia za Choveshki Otnoshenia, Bulgaria
11Clinic of Psychiatry, Faculty of Medicine, Vilnius University, Lithuania
12Aarhus University Hospital, Department M, Denmark
13Department of Methodology and Behavioral Sciences, University of Barcelona, Spain
14Psychiatric Hospital Campulung Moldovenesc, Campulung Moldovenesc, Romania
15The London School of Medicine & Dentistry Queen, Mary University of London, United Kingdom
16Faculty of Applied Social Sciences, Maria Grzegorzewska Academy of Special Education, Poland
- *Corresponding Author:
- Professor Thomas Becker
Department of Psychiatry II
Ulm University BKH Günzburg
Ludwig-Heilmeyer-Strasse 2
D-89312 Günzburg, Germany
Tel: ++49 8221 96 2001
Fax: ++49 8221 96 28160
E-mail: t.becker@uni-ulm.de
Received date: May 16, 2014; Accepted date: July 11, 2014; Published date: July 15, 2014
Citation: Weiser P, Kilian R, McDaid D, Berti L, Burti L, et al. (2014) Rationale, Component Description and Pilot Evaluation of a Physical Health Promotion Measure for People with Mental Disorders across Europe. J Community Med Health Educ 4:298. doi: 10.4172/2161-0711.1000298
Copyright: © 2014 Weiser P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Introduction: The HELPS project aimed at developing a toolkit for the promotion of physical health in people with mental disorders to reduce the substantial excess morbidity and mortality in the target group. Methods: The HELPS toolkit was developed by means of national and international literature reviews, Delphi rounds with mental health experts and focus groups with mental health experts and patients/ residents in 14 European countries. The toolkit was translated into the languages of all participating countries, and usability of toolkit modules was tested. Results: The toolkit consists of several modules addressing diverse somatic health problems, lifestyle, environment issues, patient goals and motivation for health-promotion measures. It aims at empowering people with mental illness and staff to identify physical health risks in their specific contexts and to select the most appropriate modules from a range of health promotion tools. Discussion: The HELPS project used an integrative approach to the development of simple tools for the target population and is available online in 14 European languages. Preliminary evidence suggests that the toolkit can be used in routine care settings and should be put to test in controlled trials to reveal its potential impact.
Keywords
Health promotion; Pilot/feasibility study; Motivational Interviewing; Physical health
Introduction
There is abundant evidence of excess morbidity and mortality from physical illness among people with mental disorders [1-8]. In addition to adverse effects of medication, living conditions, the higher risk of poverty and social deprivation, a lack of physical health monitoring and unhealthy lifestyles can contribute to somatic co-morbidity [2,9,10]. In particular, low levels of physical activity, poor dietary habits and excess nicotine and alcohol use are likely to contribute to poor physical health and early death [4,7,9,11,12]. However, the awareness of somatic risk factors does not automatically translate to healthy behaviour [13]. Behavioural risk factors can be modified [14-20], and the risk of physical illness decreases stepwise as positive health behaviour increases [21]. Also, there is evidence suggesting that health promotion can be effective and cost effective in the general population, although many health promotion activities require sustained behaviour change. In a systematic review of studies evaluating interventions aimed at changing health behaviour in one or more of the areas of nutrition, physical exercise, smoking, alcohol misuse, sexual risk taking and illicit drug use, Jepson et al. [22] have gathered a large body of evidence which illustrates that there are many interventions that have achieved change across a range of health behaviours.
Less attention has been focused on whether health promoting interventions are effective in people with mental health problems and whether they require adaptation for this target group [23]. In a systematic review article Verhaeghe et al. [24] identified 14 studies evaluating the effects of lifestyle interventions on body weight and subjective quality of life in people with severe mental disorders. Results of eight studies indicated significant effects of lifestyle interventions on body weight. However, a weight reduction of 5% or more as considered by the UK Department of Health to significantly reduce the risk of physical health problems was not found in any of these studies. In a more recent systematic review, van Hasselt et al. [25] identified 22 studies evaluating four types of intervention, health education (n=9), exercise (n=6), smoking cessation (n=5) and changes in health care organisation (n=2). In six studies an intervention effect on weight loss was reported, and in four studies the intervention had an effect on smoking cessation. However, in most of the studies a high drop-out rate was reported. The authors concluded that indirect interventions targeting health care practice could be more effective than interventions focusing on lifestyle change. In a systematic review of interventions for smoking cessation in patients with schizophrenia Tsoi et al. [26] found evidence of the effectiveness of a pharmacological intervention (with bupropion) but no evidence of the effectiveness of non-pharmacological interventions. Since the number of studies included in the review was small, the authors suspect that negative side-effects of buproprion might not have been identified due to the lack of power. In a systematic review of the cost-effectiveness of interventions for physical health promotion in care systems for people with severe mental illness (SMI), Park et al. [27] identified 11 studies. Only four studies that included patients with anxiety and depression evaluated the economic consequences of lifestyle interventions. The authors concluded that there is only very modest evidence for the cost-effectiveness of lifestyle interventions in people with SMI.
The HELPS project aimed to establish health behaviour interventions which might be effective and feasible in people with SMI living in health and social care facilities in Europe. The starting point of this project was the impression of a lack of effective and feasible intervention strategies to reduce physical health risk behaviour in people with SMI. The overarching aim of the HELPS project was to develop a toolkit that would empower adults with SMI to manage their physical health and encourage their participation in health promotion activities. The toolkit should be perceived by both people with SMI and mental health professionals to be acceptable, feasible and likely to help improve health lifestyles among residents of mental health care facilities across Europe. In contrast to a single intervention strategy the idea behind the development of the HELPS toolkit was to assemble a number of instruments and tools which would allow staff in different mental health care settings to assess the specific needs of the target group in the particular setting and select parts of the toolkit that best match these needs. Furthermore, the intervention was to develop a toolkit covering physical co-morbidity in mental health settings in different countries with differences in health care systems and policies and to promote service user autonomy and empowerment. This article describes the development of the toolkit and the results of a pilot study of its feasibility in mental health care facilities across Europe [28].
Methods
Building a European expert network
A European expert network was initiated with the intention to gather information on the scope of the problem and intervention strategies available in a range of European countries. The task of the expert group was to collect country-specific information and search for data and documents not published in international journals. Focus groups with patients and experts were conducted.
Focus groups
A qualitative exploratory approach consisting of focus groups was used to collect information. Qualitative methods are most productive when the research addresses the needs and abilities of the target population [29], and focus groups are an established methodology for qualitative data collection from particular target groups (e.g., professional or patient groups) that can be used to explore issues in this way [30,31]. Unlike single person interviews, the focus group technique is built on the notion that group communication encourages participants to explore and clarify individual and shared perspectives [32] and to work with group interaction processes to uncover hidden attitudes [33]. Between May 2008 and September 2009, a total of 52 focus groups (27 focus groups with people with mental illness and 25 focus groups with health professionals) were conducted. Each focus group had 3-16 participants, and a total of 372 persons (191 patients, 181 professionals, i.e. nursing staff, social workers, domestic assistants, psychologists and psychiatrists) took part.
Participants were recruited from psychiatric and social health care facilities. Focus groups were fully transcribed, and computer aided content analysis was conducted in all centres. Results of the content analyses were translated into English and sent to the co-ordinating centre. The co-ordinating centre revised the sub-code analyses where necessary, conducted further analyses to identify primary categories and compiled the results. Research questions were: (1) Which physical health problems do you/ do people with mental illness experience? (2) In your view, what are the conditions and causes that lead to these physical health problems? (3) What do you think could be done to promote the physical health of people with mental illness?
Toolkit development
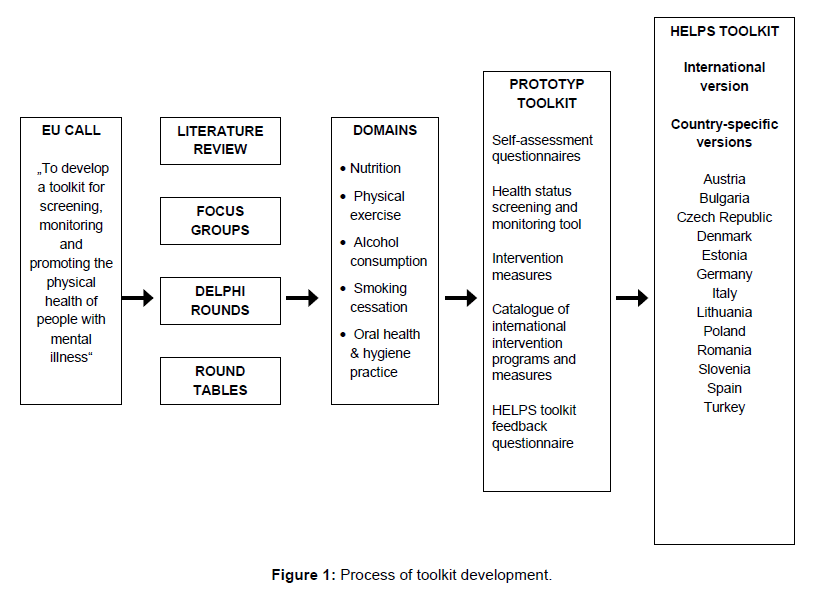
Based on the results of the focus groups the members of the expert network decided which behavioral health risks should be covered by the toolkit and which type of assessment instruments and which type of interventions should be included (Figure 1). The principal criterion for the selection of intervention programs was intervention feasibility in a broad range of mental health care facilities across participating countries.
An international version of the toolkit was produced in English and then translated into the 13 other languages represented by the network.
HELPS toolkit training workshops
A training workshop for the application of the HELPS project was developed. A manual for the use of the toolkit was developed and translated into national languages. Training workshops for toolkit use were conducted in all participating countries.
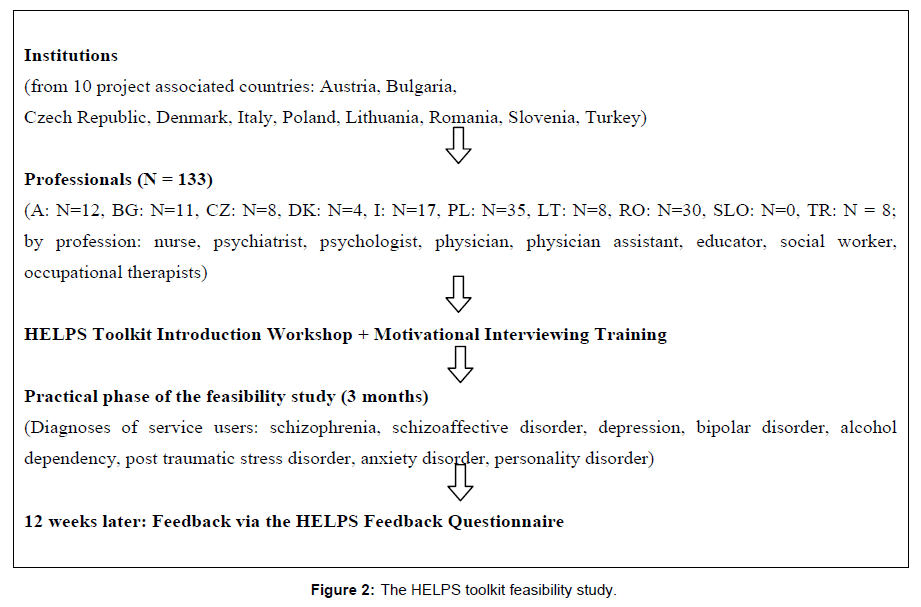
Feasibility study
Feasibility of the HELPS toolkit was examined three months after the training workshops by means of a feedback questionnaire in ten project-associated countries1. The HELPS toolkit feedback questionnaire included standardized questions on the general evaluation, acceptability, content, practical use, source material and the effectiveness of the toolkit. In addition, participants were asked to answer several open questions regarding toolkit use, satisfaction with the toolkit and suggestions for toolkit improvement (Figure 2).
Ethics approval
The study protocol was approved by the ethics committee of Ulm University (co-ordinating centre). Participating centres obtained ethics approval from their institutional ethics committees if required, and patients were asked to sign a consent form.
Results
Results of the focus groups
Service user and staff focus groups identified service user expectations and the level of commitment among service users and staff to support interventions. The physical health problems most often mentioned by patients and witnessed by staff were weight problems (e.g. increased weight, obesity), diabetes, hypertension, problems of the circulatory system, cardiovascular problems, gastrointestinal problems, and general aches and pains.
Further symptoms mentioned were poor dental health, stroke, tremors (of the fingers or legs), lethargy and weakness, high cholesterol, urinary problems and arthritis. Cancer, dehydration, thyroid problems, and arthritis
were also mentioned by several individuals. Over all, patients stressed weight and nutritional problems, gastrointestinal problems and pain while professionals emphasized lung problems (COPD), poor dental health status, infections (e.g. hepatitis), and the metabolic syndrome.
Many general and some specific causes of physical health problems and risk factors were mentioned. During the course of the discussions a number of (a) behaviour patterns and lifestyle aspects, (b) environmental circumstances, system-related factors, (c) treatment-related factors and (d) illness itself and person-related aspects were repeatedly raised.
The broad topic area discussed in the focus groups included the participants’ relationship with their social environment and their opinions concerning mental health service provision in their respective areas. During the course of the discussions a number of key issues were repeatedly raised. These were: side-effects from medications, lack of education and relevant information, and lack of resources (e.g. time for medical support and consultation, money, medical equipment).
Both participant groups’ repeatedly emphasized side-effects from medication as a main cause of the physical symptoms which participants claimed contributed to increased weight and obesity, dry mouth which could be linked with further oral-health problems such as caries, constipation, hypertension, tremor, weakness, tiredness, and feeling tired.
Poor diet was generally mentioned as a cause of physical health problems; however several participants stated that this should be viewed with respect to an individual’s right to choose what they eat. Eating behaviour patterns and conditions such as ordering fast food on inpatient wards and patient’s shopping for their own food to be cooked in social residential care services were discussed. The same applied to other lifestyle behaviours such as smoking and alcohol consumption.
Patients and staff emphasized that education is important for illness management and health promotion, and also for physical health-related issues. The provision of information on healthy nutrition, smoking cessation, sports activities/exercises, and the effects of psychiatric medication on physical health were cited as particularly important. Providing patients with the means to live a healthier lifestyle was also discussed, including the provision of healthier food in psychiatric and social health care facilities and more sporty activities for patients such as exercise and access to a gym or sport studio. Increasing co-operation between staff of mental health care facilities and general practitioners was also repeatedly cited as important. The need to spend more time with patients in order to boost their motivation was also discussed. Two main categories of motivators emerged from these discussions: “initiating motivation” was deemed relevant in initiating change in health behaviour, and “sustaining motivation” was considered important to help maintain the behaviour change. When asked about what behaviours should best be changed to reduce physical illness, participants cited changing diet, exercising, and quitting smoking. Examples of interventions were cited, with patients and residents of mental health care facilities preferring active learning (hands-on experiences) coupled with group classes for education where group members would help motivate and support each other. They also mentioned the need for skill-building interventions. “Passive learning” with self-help books or DVDs and information via the Internet was viewed as helpful by the staff, but this learning strategy was assessed rather negatively by patients.
Findings on prevention showed the highest level of variation across countries and participants, particularly with regard to implementation and realization of interventions: Professionals focused on illness-related barriers and limited institutional resources whereas service users asked for group classes on education and social support coupled with active learning experiences (skills training with hands-on experience), particularly in the fields of illness management, weight management and living skills.
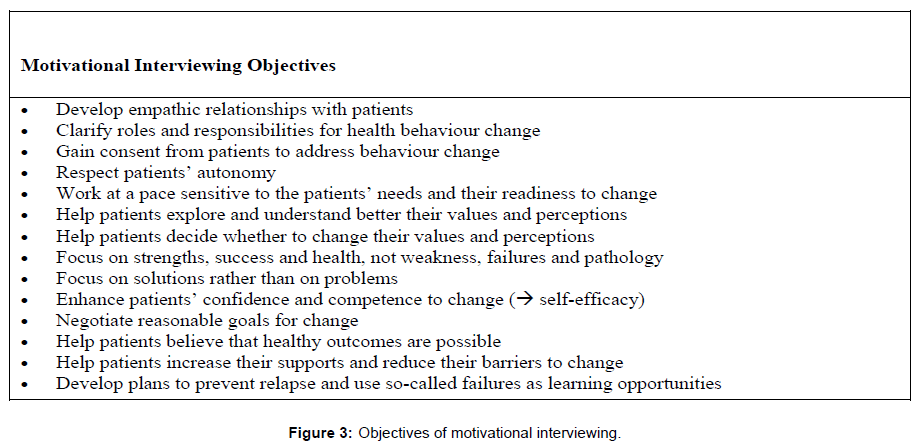
The selection of Motivational Interviewing as a general approach for health promoting interventions
Results of the focus groups indicated that physical health problems of people with severe mental disorder are related to complicated interactions between motivational and environmental factors. The main problem in selecting suitable interventions for physical health promotion is that these factors vary largely at the regional and the individual level. As a consequence, the HELPS expert network came to the conclusion that the selection of a fixed set of interventions would not meet the specific needs of a member of the target group. It was agreed that a health promoting toolkit should provide general techniques which could be flexibly adapted to a great variety of individual and situational needs (Figure 3).
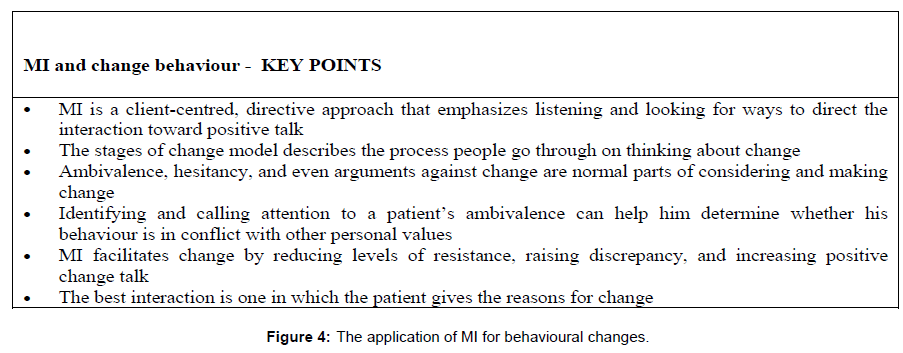
The technique of Motivational Interviewing (MI) was agreed to be well suited to address this requirement. The MI approach posits that responsibility and capability for change lie within the patient. The MI therapist’s task is to create a set of conditions that will enhance patients’ motivation to change. Rather than relying upon therapy sessions as the primary locus of change, the therapist seeks to mobilize the patient’s inner resources. Thus, MI seeks to support intrinsic motivation for change leading to sustained behaviour change. Dunn et al. [34] performed a systematic review of 29 randomized trials and showed that MI effects did not appear to diminish over time. Moreover, it has been argued that the non-confrontational style of MI is more suited to people with psychosomatic mental disorders than more confrontational methods traditionally favoured in substance use care settings. MI is well-grounded in theory and research. It draws on motivational principles derived from both experimental and clinical research. The efficacy of MI in the treatment of addiction, particularly to alcohol and tobacco, has been examined and proven in numerous studies [34-37]. MI is now also used in several clinical trials to enhance positive health behaviours including diet and exercise [38,39]. MI overall effectiveness compares favourably with other treatment approaches, and when cost-effectiveness is considered, MI performs well compared with other approaches [40]. MI in group settings has also been shown to be effective [41]. Overall, MI could be proven as cost-effective, efficient and minimally intrusive in improving physical lifestyles, e.g. through healthy diet and increased physical activity [35,38,39]. Nevertheless, there is a lack of research and studies in outpatient settings. Although there is wide evidence of MI effectiveness in inpatient facilities, there is no effort to examine MI in outpatient settings with people with enduring mental illness.
HELPS Toolkit development
It was agreed by the members of the expert network that the HELPS toolkit should adapt to different population needs, and that therefore varied formats for interventions were needed. As a starting point a screening tool for the examination of physical health status among people with mental illness was developed under the lead of the centre in Izmir on the basis of international recommendations. To cover the regional differences and the needs of a broad spectrum of patients identified in the focus groups, the literature review health promotion programs were developed on the basis of the Motivational Interviewing technique and on the particular experiences of network members from centres in Verona, Warsaw, Aalborg and Ulm. As a result, the HELPS toolkit is a multi-faceted set of materials including components with a special focus on promoting healthy nutrition, exercise, oral health and oral hygiene as well as decreasing tobacco and harmful alcohol consumption (available at http://www.uni-ulm. de/helps-net/index.htm). It concentrates on negotiating, agreeing on and leading the patient through individualized health promotion plans developed in partnership between individuals with mental health problems and health care staff. Mental health workers thereby support patients to develop strategies for change and manage a healthy lifestyle. One-to-one sessions are easily organised, with more time devoted to specific issues. On the other hand, the group format offers more varied feedback, social support and role models, and group sessions require fewer staff. The HELPS toolkit can be used by members of different professional groups, and it is compatible with individual and/or group-based settings. The frequency, duration and types of activity are adapted to patients’ health status, goals and aspiration levels. The toolkit includes instruments to screen the physical health status of service users and to assess unhealthy behaviour (dietary habits, physical activity, tobacco and alcohol use, oral health and hygiene). It also comprises intervention programmes, booklets for clients, handouts, worksheets and educational materials introducing mental health practitioners to MI (Figures 1 and 4). MI was used to help service users with health behaviour choices, to avoid authoritarian judgment and instructional approaches. Key principles such as expressing empathy, supporting self-efficacy, ‘rolling with resistance’ and assisting the client to examine discrepancies between current and desired behaviour and goals were considered pivotal [42]. In the trans-theoretical stage model [43,44] change is seen as a process involving progress through a series of stages where the patient’s readiness to change is identified in order to match materials and messages delivered to individual patient need.
The international HELPS toolkit (in English) was developed, and HELPS partners used it to develop country-specific tools translated and adapted to national settings. Country-specific toolkits are available for Austria, Bulgaria, Czech Republic, Denmark, Estonia, Germany, Italy, Lithuania, Poland, Romania, Slovenia, Spain and Turkey.
What is provided in the HELPS toolkit?
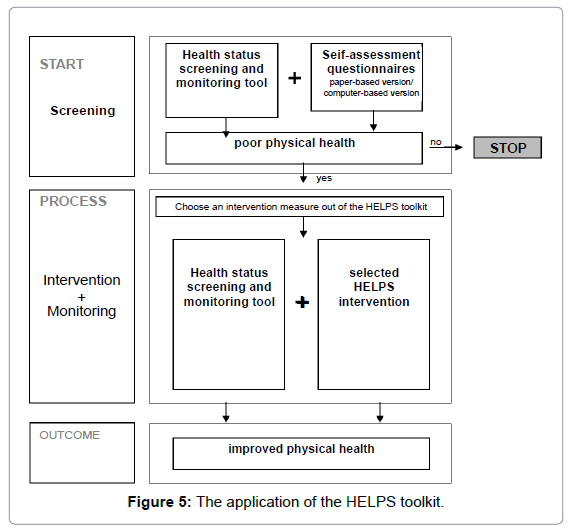
Four different health promotion programs for people with mental illness were developed by the project centres in Denmark, Poland, Italy and Germany for the international version of the HELPS toolkit. A selection of these programs was included in all national versions of the HELPS toolkit. There are five modules on: Nutrition, Physical activity, Smoking, Alcohol consumption and Oral health and oral hygiene. Modules comprise different components (Figure 5)
a) Self-assessment questionnaires
Questionnaires for service user self-assessment contain sections on nutrition, physical activity, smoking, alcohol use and oral health practice. Each section consists of 10 simple yes/no items such as “I am at a stage where I should think about smoking fewer cigarettes” or “have you ever felt that you should become more physically active?” These assessment instruments help to identify motivation for health behaviour change. There are paper and electronic versions of the HELPS assessment questionnaires (in 12 languages1) including analysis, interpretation and a graphical presentation of results.
b) Health status screening and monitoring tool
The screening and monitoring tool helps practitioners plan health promotion activities and monitor the physical health status of service users. A comprehensive assessment includes the patient’s medical history, physical examination (e.g., waist circumference, body mass index, blood pressure) and laboratory parameters (e.g. lipid status). A set of recommendations for further health monitoring is also made.
c) Intervention measures
The toolkit contains several specific interventions that may be considered by health care professionals in different contexts and settings.
There are three health information booklets entitled “How to lower your cholesterol level”; “Hypertension – How to decrease your blood pressure”; and “Sex and living together: Good sex life – even when you’re living with a heart disease”2.The motivational enhancement treatment manual is a clinical research guide for therapists treating individuals with alcohol abuse and dependence [45]. New manuals were developed to provide guidance on the use of MI in people with mental disorders with regard to nutrition, physical activity, smoking cessation, oral health and oral hygiene. These manuals are based on the MI technique [42]. They have been adapted for people with mental health problems with a particular focus on cognitive deficits and social impairment, and they include workbooks with worksheets, handouts, case studies and examples3.
1. My Health – I care is a health promoting programme for psychiatric patients of inpatient and outpatient facilities developed in Poland. Aims of the programme are (1) to initiate weight loss in obese patients, (2) to modify dietary habits, (3) to encourage daily physical activity, and (4) to increase motivation of individuals to take responsibility of their physical health. The programme comprises individual consultations, weekly group workshops and lectures. Individual consultations last 20 to 45 minutes each, depending on a patient’s individual needs. Weekly group workshops function as support groups in an open form. During each session, activities include 30 minutes of physical exercise (dance in a circle), 30 minutes of relaxing music and 30 minutes of group work on dietary habits and physical xercise.4
2. Physico is a physical health promotion intervention and a health education programme for community mental health services. This intervention builds upon the experience acquired in a project on health education for diet and physical exercise. It has been designed and implemented in Italy. It aims to implement health promotion strategies related to dietary habits and physical exercise in people using psychiatric services. It comprises an evaluation of patient food provided in services; educational sessions on the importance of diet and fitness; regular physical exercise under the supervision of an expert trainer; motivational interviews to foster service adherence among users, to discuss physical health condition, habits and views on diet and fitness, to monitor programme adherence and health behaviour5.
d) Catalogue of international intervention programmes and measures
The catalogue provides an overview of existing interventions to promote physical health. It is a collection of information, publications and contact addresses based on a search using formal and informal sources (literature research, information from professionals, internet search) from 14 European countries with HELPS partners.
e) HELPS toolkit feedback questionnaire
The toolkit includes a questionnaire for feedback. The issues covered include feasibility, acceptability, practicability, content, usefulness of intervention materials (e.g. manuals and worksheets), whether the toolkit can be implemented, and its effectiveness. Respondents give a global score per domain (yes, undecided, no), and they are given the opportunity to suggest modifications (e.g., “Which elements of the toolkit could be improved to make them more appropriate to your needs? Please suggest improvements where possible” or “What factors facilitate or hinder the implementation of the HELPS toolkit?”).
How does the toolkit work?
The toolkit recommends the use of the health risk assessment questionnaire and physical health status screening tool. These are seen as entry points for a health promotion intervention. Service users identified as being at risk for specific somatic health problems are guided to specific intervention measures. The health practitioner and service user establish a relationship and identify the service user’s health goals and aims. They start with one of the HELPS toolkit intervention modules (as a sole measure or in combination with an intervention programme). For example, using MI the health practitioner and service user start by developing an activity plan (worksheet: HELPS Action Plan) which documents clients’ personal goals for behaviour change. Action plans are individually tailored based on patient health status. The plan may address alcohol and tobacco use, nutrition intake, physical exercise or oral health and related health goals, e.g. skills training and cooking healthy meals. Health practitioners support service users in identifying personal objectives and preferred ways to achieve change. This approach is consistent with initiatives at the US National Institute for Mental Health (NIMH) calling for individually tailored interventions [46] .
During subsequent sessions, health practitioners monitor and revise progress towards the objectives identified. Sessions incorporate modelling positive reinforcement strategies to bolster self-efficacy for behaviour change, problem-solving techniques to explore barriers and to help service users modify their objectives to reach their goals. Health practitioners may refer patients for health education (e.g., nutrition consultation) or skills training. Health practitioners use MI approaches to encourage service user involvement.
HELPS toolkit feasibility study and piloting
A total of 133 mental health care workers from 10 countries participated in the feasibility study. Participants included nurses, psychologists, psychiatrists and social workers. The wide range of patient diagnoses that study participants referred to included schizophrenia, depression, alcohol dependency and (severe) personality disorder. Feedback questionnaires were completed by 93 to 95 mental health experts. As shown in Table 1 the overall toolkit was considered as having good average quality with a range from exciting to awful.
| exciting | good | neutral | poor | awful | total | |
|---|---|---|---|---|---|---|
| Interest in the toolkitn (%) | 19 (20.2) | 56 (59.6) | 15(16.0) | 3 (3.2) | 1 (1.1) | 94 (100) |
| Quality ofthe toolkitn (%) | 31 (32.6) | 44 (46.3) | 18 (18.9) | 2 (2.1) | 0 (0) | 95 (100) |
| Usefulness of informationn (%) | 31 (32.9) | 46 (48.9) | 16 (17.0) | 1 (1.1) | 0 (0) | 94 (100) |
| Managebility of information n (%) | 19 (20.0) | 49 (51.6) | 24 (25.3) | 2 (2.1) | 1 (1.1) | 95 (100) |
| Practicability of information n (%) | 26 (27.4) | 40 (42.1) | 26 (27.4) | 3 (3.2) | 0 (0) | 95 (100) |
1)Italy, Bulgaria, Turkey, Austria, Denmark, Czech Republic, Slovenia, Romania, Poland, Lithuania
Table 1: Evaluation of overall characteristics of the HELPS toolkit by mental health care experts from 10 countries1)
Evaluations of the different features of the toolkit are presented in Table 2. The majority of the mental health care workers were satisfied with the toolkit and expressed the intention to use it in daily practice.
| yesn (%) | Undecidedn (%) | Non (%) | Totaln (%) | |
|---|---|---|---|---|
| Acceptability ofthe HELPS toolkit | ||||
| I am satisfied with the toolkit | 75 (79.8) | 16 (17.0) | 3 (3.2) | 94 (100) |
| I have the intention to use the toolkit | 73 (78.5) | 17 (18.3) | 3 (3.2) | 93 (100) |
| The toolkit fits within the organizational culture of the facility | 62 (66.7) | 19 (20.4) | 12 (12.9) | 93 (100) |
| Content of the HELPS toolkit | ||||
| The content of the toolkit is interesting | 87(91.6) | 2 (2.1) | 6 (6.3) | 95 (100) |
| Too much of the content is not useful | 31 (33.3) | 22 (23.7) | 40 (43.1) | 93 (100) |
| The content is relevant forthe facility | 64(67.4) | 25 (26.3) | 6 (6.3) | 95 (100) |
| The content addresses patient needs | 60 (63.2) | 14 (14.7) | 21 (22.1) | 95 (100) |
| The content addresses the aims of the staff | 66 (69.5) | 18 (18.9) | 11 (11.6) | 95 (100) |
| The content addresses the aims of the facility | 60 (63.2) | 23 (24.2) | 12 (12.6) | 95 (100) |
| Applicability ofthe HELPS toolkit | ||||
| I found the toolkit easy to follow | 72 (77.4) | 13 (14.0) | 8 (8.6) | 93 (100) |
| The delivery ofthe program was well organized | 84 (90.3) | 6 (6.4) | 3 (3.2) | 93 (100) |
| There were enough means and resources to carry out the toolkit | 76 (80.9) | 14 (14.9) | 4 (4.3) | 94 (100) |
| The toolkit is suitable for patients with severe mental illness | 69 (73.4) | 19 (20.2) | 6 (6.4) | 94 (100) |
| Source material | ||||
| I found the instructions in the toolkit useful | 90 (95.7) | 2 (2.1) | 2 (2.1) | 94 (100) |
| The information in the toolkit was clearly presented | 86 (91.5) | 6 (6.4) | 2 (2.1) | 94 (100) |
| The paper version ofthe toolkit is usable | 81 (86.2) | 8 (8.5) | 5 (5.3) | 94 (100) |
| The electronic version ofthe toolkit is usable | 18 (28.6) | 31 (49.2) | 14 (22.2) | 63 (100) |
| Effectiveness of the HELPS toolkit | ||||
| The application of the HELPS toolkit had positive effects on patients’ physical health | 61 (64.9) | 23 (24.5) | 10 (10.6) | 94 (100) |
| The application of the HELPS toolkit had positive effects on patients’ well-being | 68 (72.3) | 20 (21.3) | 6 (6.4) | 94 (100) |
| The application of the HELPS toolkit had positive effects on patients’health behaviour | 61 (64.9) | 27 (28.7) | 6 (6.4) | 94 (100) |
| Adverse effects of the HELPS toolkit | ||||
| The application of the HELPS toolkit had negative effects on patients‘physical health | 3 (3.2) | 25 (26.6) | 66 (70.2) | 94 (100) |
| The application of the HELPS toolkit had negative effects on patients’well-being | 7 (7.4) | 25 (26.6) | 62 (66.0) | 94 (100) |
| The application of the HELPS toolkit had negative effects on patients’ health behavior | 2 (2.1) | 26 (27.7) | 66 (70.2) | 94 (100) |
| 1) Italy, Bulgaria, Turkey, Austria, Denmark, Czech Republic, Slovenia, Romania, Poland, Lithuania | ||||
| yesn (%) | Undecidedn (%) | Non (%) | Totaln (%) | |
| Acceptability ofthe HELPS toolkit | ||||
| I am satisfied with the toolkit | 75 (79.8) | 16 (17.0) | 3 (3.2) | 94 (100) |
| I have the intention to use the toolkit | 73 (78.5) | 17 (18.3) | 3 (3.2) | 93 (100) |
| The toolkit fits within the organizational culture of the facility | 62 (66.7) | 19 (20.4) | 12 (12.9) | 93 (100) |
| Content of the HELPS toolkit | ||||
| The content of the toolkit is interesting | 87(91.6) | 2 (2.1) | 6 (6.3) | 95 (100) |
| Too much of the content is not useful | 31 (33.3) | 22 (23.7) | 40 (43.1) | 93 (100) |
| The content is relevant forthe facility | 64(67.4) | 25 (26.3) | 6 (6.3) | 95 (100) |
| The content addresses patient needs | 60 (63.2) | 14 (14.7) | 21 (22.1) | 95 (100) |
| The content addresses the aims of the staff | 66 (69.5) | 18 (18.9) | 11 (11.6) | 95 (100) |
| The content addresses the aims of the facility | 60 (63.2) | 23 (24.2) | 12 (12.6) | 95 (100) |
| Applicability ofthe HELPS toolkit | ||||
| I found the toolkit easy to follow | 72 (77.4) | 13 (14.0) | 8 (8.6) | 93 (100) |
| The delivery ofthe program was well organized | 84 (90.3) | 6 (6.4) | 3 (3.2) | 93 (100) |
| There were enough means and resources to carry out the toolkit | 76 (80.9) | 14 (14.9) | 4 (4.3) | 94 (100) |
| The toolkit is suitable for patients with severe mental illness | 69 (73.4) | 19 (20.2) | 6 (6.4) | 94 (100) |
| Source material | ||||
| I found the instructions in the toolkit useful | 90 (95.7) | 2 (2.1) | 2 (2.1) | 94 (100) |
| The information in the toolkit was clearly presented | 86 (91.5) | 6 (6.4) | 2 (2.1) | 94 (100) |
| The paper version ofthe toolkit is usable | 81 (86.2) | 8 (8.5) | 5 (5.3) | 94 (100) |
| The electronic version ofthe toolkit is usable | 18 (28.6) | 31 (49.2) | 14 (22.2) | 63 (100) |
| Effectiveness of the HELPS toolkit | ||||
| The application of the HELPS toolkit had positive effects on patients’ physical health | 61 (64.9) | 23 (24.5) | 10 (10.6) | 94 (100) |
| The application of the HELPS toolkit had positive effects on patients’ well-being | 68 (72.3) | 20 (21.3) | 6 (6.4) | 94 (100) |
| The application of the HELPS toolkit had positive effects on patients’health behaviour | 61 (64.9) | 27 (28.7) | 6 (6.4) | 94 (100) |
| Adverse effects of the HELPS toolkit | ||||
| The application of the HELPS toolkit had negative effects on patients‘physical health | 3 (3.2) | 25 (26.6) | 66 (70.2) | 94 (100) |
| The application of the HELPS toolkit had negative effects on patients’well-being | 7 (7.4) | 25 (26.6) | 62 (66.0) | 94 (100) |
| The application of the HELPS toolkit had negative effects on patients’ health behavior | 2 (2.1) | 26 (27.7) | 66 (70.2) | 94 (100) |
1) Italy, Bulgaria, Turkey, Austria, Denmark, Czech Republic, Slovenia, Romania, Poland, Lithuania
Table 2: Evaluation of features of the HELPS toolkit by mental health care experts from 10 countries1).
The toolkit was also assessed to fit in well with the organisational culture of the facilities where participants worked. The content of the toolkit was found to be interesting by the overwhelming majority of the participants. However, a substantial number of about 33% found that too much of the material provided in the toolkit was not very useful in daily practice. Nevertheless, the content of the toolkit was assessed as addressing patient needs and the aims of staff. The instructions and presentation of toolkit material was assessed as positive by the clear majority of participants. However, the electronic version of the toolkit was only tested by a small number of participants, and its usability was rated as being relatively poor. A majority of participants expressed the expectation that the application of the HELPS toolkit would have positive effects on physical health, psychological well-being and health behaviour among persons with SMI. Adverse effects of the toolkit were only expected by very few participants. Nevertheless, about 25% of the participants were not convinced that applying the toolkit would have no adverse effects.
Verbal comments on feasibility and acceptability were generally positive. There were some concerns about correct implementation and use in the absence of health promotion specialists, e.g., dieticians or sports therapists, who may not be available in mental health care facilities, as well as a lack of supervision of MI. Most participants mentioned being unfamiliar with the MI concept and requested more training. Manageability and practicability were rated as fairly good to moderate. There was concern regarding the training time required for MI. The paper-based and electronic versions of the assessment questionnaires were considered feasible, and visual features such as worksheets and handouts (e.g., Readiness scale and Action plan) were thought to be appealing and easy to use.
Mental health workers reported improvements in therapeutic relationship and positive feedback from service users following HELPS toolkit use. MI appeared to be useful in enabling service users to be more confident and self-assertive. Moreover, professionals were rated by users as being allies stimulating their inner drive for healthy behaviour. Service users would communicate and discuss somatic complaints and unhealthy behaviour more openly, and they appeared more dedicated to lifestyle change following toolkit use. People with mental illness enrolled in the HELPS intervention reported health benefits in a variety of domains. They managed to reduce waist circumference and reported improvements in body fitness, overall health status and mental health functioning. Statements by professionals indicate that the toolkit was successful in empowering people with mental health problems to improve self-efficacy (e.g., via social activities such as sport groups, courses for learning healthy cooking and self-help groups). Developing an electronic hyperlinked version of the toolkit was suggested as one way of improving it. The use of visual media and group sessions for families was considered useful. Health care professionals noted a need for coaching.
Discussion
Substantial evidence suggests that people with mental disorders engaging in health promotion interventions such as physical exercise, diet change, smoking cessation, reduction of alcohol consumption and other lifestyle changes can modify health behaviour and improve their physical health (e.g. reduction in risk of diabetes or heart attack) and overall health (e.g. improvements in emotional well-being) across their lifespan [23,24,47]. There is some evidence regarding individual health promotion interventions to reduce physical co-morbidity (e.g. physical activity programmes). HELPS was a project aimed at the promotion of physical health among mental health service users in European countries.
The general objective of the HELPS project was to provide simple, evidence-driven tools across Europe to promote physical health of people with mental illness. Preliminary pilot data on the implementation of the HELPS toolkit support its feasibility and acceptability in different service contexts in a number of health systems. Users reported that the intervention was useful and respectful, that it would help in dealing with somatic complaints and support people with mental health problems in making progress towards their “healthy goals”. These early feasibility findings are consistent with other reports that people with mental health problems can improve their physical and mental health [48]. Use of one or more components of the HELPS toolkit offers opportunities for individuals to adopt health-promoting lifestyles. Professional toolkit users choose how best to use the toolkit in their work settings (e.g. by adapting it to their health system, service practice, working time, number of contacts with patients, infrastructure and financial resources). The toolkit strengthens empowerment and autonomy. Monitoring of toolkit use and health outcomes will be important. Lack of fidelity in implementation can be a barrier to success. It will be critical to determine what actual impacts there are in terms of sustained health behaviour change and longer term health outcomes.
Limitations and Strengths
Limitations of focus group interviews (with mental health professionals and people with mental illness) and expert consultations (e.g. Delphi rounds) used in developing the toolkit include selection bias and response bias. The HELPS toolkit needs to be tested in a controlled trial. The feasibility study was limited by a brief followup period (3 months) and small number of staff and service users included in feasibility interviews, and there is no data on the retention of service users in the HELPS intervention. There was no control for effects of specific health practitioners and therapeutic relationship. Major physical illnesses are caused by multiple factors associated with health outcomes (e.g., poor nutrition combined with sedentary lifestyle increases the risk for metabolic health problems). Little is known about factors that facilitate or impair success in multiple-component health interventions [49]. A composite index of overall behaviour change including empowerment and quality of life would be helpful. MI is time-consuming and costly, and this may impair implementation of the HELPS toolkit.
Some strength should be noted. The HELPS toolkit adds to existing measures by being feasible across a range of settings in European health care systems, and it is freely available online in 12 languages (http://www.uni-ulm.de/helps-net/helps_toolkit.htm). MI is one of the most promising approaches to facilitating behaviour change in at-risk populations [50]. In the framework of the HELPS toolkit, MI can be used as a stand-alone intervention or in combination with other health promotion interventions. Use of the toolkit can increase healthcare workers’ awareness of their role in the detection of somatic illness in their clients, improve communication and contribute to a health-promoting environment. Skills acquired during the HELPS intervention could place service users on a trajectory of aftercare that reinforces their learning, promotes healthy behaviour and empowers them to improve their physical health.
Conclusion
The HELPS project is unique in its integrative approach to promoting the physical health of people with mental disorders in residential and community settings, and it addresses barriers to health promotion. The HELPS project adds to clinical practice by (1) being individually tailored to address the needs of people with mental disorders, (2) targeting people with all mental disorders, (3) including those living in the community, (4) being adaptable to varied mental health care settings, and (5) being available at no cost in a number of European languages.
Performing controlled trials to evaluate effectiveness is the next step. Outcome assessment should focus on traditional domains of physical health management (e.g. markers of metabolic syndrome or of cardiovascular health) and outcomes related to empowerment and quality of life. Follow-up assessments are needed to determine whether gains are maintained over time. Finally, costs and cost effectiveness of health promotion interventions such as the HELPS toolkit should be evaluated to inform policy and practice.
Addendum note: acknowledgement and HELPS website
The HELPS project was funded by the European Commission (DG SANCO, Contract No.: 2006224). The HELPS toolkit is available via the HELPS website at http://www.uni-ulm.de/helps-net/index.htm. The website provides information on the project, its background and project partners. Information is available in different languages. The direct link to international and country-specific toolkits is http://www.uni-ulm. de/helps-net/helps_toolkit.htm. The international version is available in English. The country-specific versions are available in the following languages: Bulgarian, Czech, Danish, English, Estonian, German, Italian, Lithuanian, Romanian, Slovenian, Spanish and Turkish.
1Bulgarian, Czech, Danish, Dutch, English, German, Italian, Lithuanian, Romania, Slovenian, Spanish, and Turkish
2For more information on these booklets contact Peter Hjorth, Åalborg Psychiatric Hospital, Aarhus University, Åalborg, Denmark. Email: ashanti@mail.dk
3For more information on these manuals contact Prisca Weiser, University Medical Center Mainz, Department of Psychosomatic and Psychotherapy, Langenbeckstr. 1, 55131 Mainz, Germany. Phone: ++49 6131 178424, Email: prisca.weiser@ unimedizin-mainz.de
4For more information contact Katarzyna Lech, Wolski Hospital, Community Care Department, Warsaw, Poland. Email: gabinet@harmony.pl
5For more information contact Lorenzo Burti or Loretta Berti, Universitá degli Studi di Verona, Verona, Italy. E-mail: lorenzo.burti@univr.it or loretta.berti@univr.it
References
- Bushe CJ, Bradley AJ, Wildgust HJ, Hodgson RE (2009) Schizophrenia and breast cancer incidence: a systematic review of clinical studies. Schizophr Res 114: 6-16.
- Felker B, Yazel JJ, Short D (1996) Mortality and medical comorbidity among psychiatric patients: a review. PsychiatrServ 47: 1356-1363.
- Jones DR, Macias C, Barreira PJ, Fisher WH, Hargreaves WA, et al. (2004) Prevalence, severity, and co-occurrence of chronic physical health problems of persons with serious mental illness. PsychiatrServ 55: 1250-1257.
- Kilbourne AM, Rofey DL, McCarthy JF, Post EP, Welsh D, et al. (2007) Nutrition and exercise behavior among patients with bipolar disorder. Bipolar Disord 9: 443-452.
- Leucht S, Burkard T, Henderson J, Maj M, Sartorius N (2007) Physical illness and schizophrenia: a review of the literature. ActaPsychiatrScand 116: 317-333.
- Räsänen S, Meyer-Rochow VB, Moring J, Hakko H (2007) Hospital-treated physical illnesses and mortality: an 11-year follow-up study of long-stay psychiatric patients. Eur Psychiatry 22: 211-218.
- von Hausswolff-Juhlin Y, Bjartveit M, Lindström E, Jones P (2009) Schizophrenia and physical health problems. ActaPsychiatrScandSuppl : 15-21.
- DE Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, et al. (2011) Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 10: 52-77.
- Brown S, Birtwistle J, Roe L, Thompson C (1999) The unhealthy lifestyle of people with schizophrenia. Psychol Med 29: 697-701.
- Colton CW, Manderscheid RW (2006) Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis 3: A42.
- McCreadie RG; Scottish Schizophrenia Lifestyle Group (2003) Diet, smoking and cardiovascular risk in people with schizophrenia: descriptive study. Br J Psychiatry 183: 534-539.
- Osborn DP, Nazareth I, King MB (2007) Physical activity, dietary habits and Coronary Heart Disease risk factor knowledge amongst people with severe mental illness: a cross sectional comparative study in primary care. Soc Psychiatry PsychiatrEpidemiol 42: 787-793.
- Roick C, Fritz-Wieacker A, Matschinger H, Heider D, Schindler J, et al. (2007) Health habits of patients with schizophrenia. Soc Psychiatry PsychiatrEpidemiol 42: 268-276.
- Bauman AE (2004) Updating the evidence that physical activity is good for health: an epidemiological review 2000-2003. J Sci Med Sport 7: 6-19.
- Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, et al. (1999) Effects of exercise training on older patients with major depression. Arch Intern Med 159: 2349-2356.
- Bridle C, Riemsma RP, Pattenden J, Sowden AJ, Mather L et al. (2005) Systematic review of the effectiveness of health behavior interventions based on the transtheoretical model. Psychology & Health 20(3): 283-301.
- Craft L, Landers D (1998) The effects of exercise on clinical depression and depression resulting from mental illness: A meta-analysis. J Sport ExercPsychol (Journal of Sport and Exercise Psychology) 20: 339-357.
- Lawrence D, Holman D, Jablensky A (2001) Preventable physical illness in people with mental illness. Centre for Health Services Research, Dept. of Public Health, University of Western Australia, 107-117.
- Littrell KH, Hilligoss NM, Kirshner CD, Petty RG, Johnson CG (2003) The effects of an educational intervention on antipsychotic-induced weight gain. J NursScholarsh 35: 237-241.
- Shiner B, Whitley R, van Citters AD, Pratt SI, Bartels SJ (2008) Learning what matters for patients: qualitative evaluation of a health promotion program for those with serious mental illness. Health Promotion International 23: 275-282.
- Melamed Y, Stein-Reisner O, Gelkopf M, Levi G, Sivan T, et al. (2008) Multi-modal weight control intervention for people with persistent mental disorders. PsychiatrRehabil J 31: 194-200.
- Jepson RG, Harris FM, Platt S, Tannahill C (2010) The effectiveness of interventions to change six health behaviours: a review of reviews. BMC Public Health 10: 538.
- Bartels S, Desilets R (2012) Health promotion programs for persons with serious mental illness: What works? SAMHSA-HRSA Center for Integrated Health Solutions. 1-41.
- Verhaeghe N, De Maeseneer J, Maes L, Van Heeringen C, Annemans L (2011) Effectiveness and cost-effectiveness of lifestyle interventions on physical activity and eating habits in persons with severe mental disorders: a systematic review. Int J BehavNutrPhys Act 8: 28.
- van Hasselt FM, Krabbe PF, van Ittersum DG, Postma MJ, Loonen AJ (2013) Evaluating interventions to improve somatic health in severe mental illness: a systematic review. ActaPsychiatrScand .
- Tsoi DT, Porwal M, Webster AC (2013) Interventions for smoking cessation and reduction in individuals with schizophrenia. Cochrane Database Syst Rev 2: 1-90.
- Park AL, McDaid D, Weiser P, Von Gottberg C, Becker T, et al. (2013) Examining the cost effectiveness of interventions to promote the physical health of people with mental health problems: a systematic review. BMC Public Health 13: 787.
- Weiser P, Becker T, Losert C, Alptekin K, Berti L, et al. (2009) European network for promoting the physical health of residents in psychiatric and social care facilities (HELPS): background, aims and methods. BMC Public Health 9: 315.
- Achterberg CL, Shepherd SK (1992) The components and use of qualitative research. In: Monsen ER (ed) Research. Successful approaches. American Dietetic Association 73-81.
- Leys M (2003) Health technology assessment: the contribution of qualitative research. Int J Technol Assess Health Care 19: 317-329.
- Liamputtong P, Ezzy D (2005) Qualitative research methods
- Morgan DL (1988) Focus groups as qualitative research, Qualitative research methods 16.
- Joos S, Musselmann B, Miksch A, Rosemann T, Szecsenyi J (2008) The role of complementary and alternative medicine (CAM) in Germany - a focus group study of GPs. BMC Health Serv Res 8: 127.
- Dunn C, Deroo L, Rivara FP (2001) The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction 96: 1725-1742.
- Burke BL, Arkowitz H, Menchola M (2003) The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. J Consult ClinPsychol 71: 843-861.
- Baker A, Richmond R, Castle D, Kulkarni J, Kay-Lambkin F, et al. (2009) Coronary heart disease risk reduction intervention among overweight smokers with a psychotic disorder: pilot trial. Aust N Z J Psychiatry 43: 129-135.
- Rollnick S, Miller WR, Butler C (2008) Motivational interviewing in health care. Helping patients change behavior. Applications of motivational interviewing.
- Hecht J, Borrelli B, Breger RK, Defrancesco C, Ernst D, et al. (2005) Motivational interviewing in community-based research: experiences from the field. Ann Behav Med 29 Suppl: 29-34.
- Chanut F, Brown TG, Donguier M (2005) Motivational interviewing and clinical psychiatry. Can J Psychiatry 50: 715-721.
- Carels RA, Darby L, Cacciapaglia HM, Konrad K, Coit C, et al. (2007) Using motivational interviewing as a supplement to obesity treatment: a stepped-care approach. Health Psychol 26: 369-374.
- Santa Ana EJ, Wulfert E, Nietert PJ (2007) Efficacy of group motivational interviewing (GMI) for psychiatric inpatients with chemical dependence. J Consult ClinPsychol 75: 816-822.
- Boardman T, Catley D, Grobe JE, Little TD, Ahluwalia JS (2006) Using motivational interviewing with smokers: do therapist behaviors relate to engagement and therapeutic alliance? J Subst Abuse Treat 31: 329-339.
- Prochaska JO, DiClemente CC (1992) Stages of change in the modification of problem behaviors. ProgBehavModif 28: 183-218.
- Prochaska JO, Velicer WF (1997) Thetranstheoretical model of health behavior change. Am J Health Promot 12: 38-48.
- Miller WR (1994]) Motivational enhancement therapy manual. National Institute of Alcohol Abuse and Alcoholism 2: 1-35.
- NIMH (2008) National Institute of Mental Health Strategic Plan. 1-46.
- Richardson CR, Faulkner G, McDevitt J, Skrinar GS, Hutchinson DS, et al. (2005) Integrating physical activity into mental health services for persons with serious mental illness. PsychiatrServ 56: 324-331.
- Van Citters AD, Pratt SI, Jue K, Williams G, Miller PT, et al. (2010) A pilot evaluation of the In SHAPE individualized health promotion intervention for adults with mental illness. Community Ment Health J 46: 540-552.
- Prochaska JJ, Nigg CR, Spring B, Velicer WF, Prochaska JO (2010) The benefits and challenges of multiple health behavior change in research and in practice. Prev Med 50: 26-29.
- Prochaska JO (2005) Health behavior change research: a consortium approach to collaborative science. Ann Behav Med 29 Suppl: 4-6.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 14887
- [From(publication date):
September-2014 - Apr 17, 2025] - Breakdown by view type
- HTML page views : 10348
- PDF downloads : 4539