Rare Primary Sub-Mucosal Rectal Squamous Cell Carcinoma Diagnosed with Endoscopic Ultrasound: Case Report and Literature Review
Received: 28-Oct-2017 / Accepted Date: 08-Nov-2017 / Published Date: 15-Nov-2017 DOI: 10.4172/2161-069X.1000535
Abstract
Primary rectal Squamous Cell Carcinoma (SCC) is a distinct and extremely rare form of colorectal malignancy and submucosal rectal SCC is rarer. The etiology and pathogenesis of rectal SCC is poorly understood. Given the rare occurrence of this type of malignancy, there are a number of diagnostic and therapeutic dilemmas. We are reporting a case of a 56-year-old female, who presented with abdominal pain and found to have rectal mass which was subsequently biopsied under endoscopic ultrasound guidance. Histopathology showed primary submucosal squamous cell carcinoma. She was treated with radiotherapy and systemic chemotherapy. Now she is undergoing regular malignancy surveillance.
Keywords: Rectal squamous cell carcinoma; Lymphoma; Endoscopic ultrasound; Chemotherapy
Introduction
Squamous cell rectal carcinoma is a distinct and extremely rare form of colorectal malignancy which has been primarily reported as case reports. The etiology and pathogenesis remain unclear, although, various mechanisms have been postulated.
Squamous cell rectal carcinoma is a distinct and extremely rare form of colorectal malignancy which has been primarily reported as case reports. The etiology and pathogenesis remain unclear, although, various mechanisms have been postulated.
Case Report
A 56-year-old female with a past medical history of colonic diverticulosis and bowel obstruction, presented with abdominal discomfort for two weeks. Her physical exam was unremarkable except for mild abdominal tenderness.
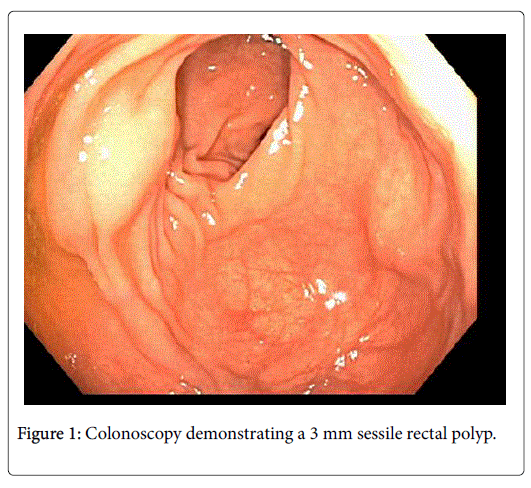
Computerized tomography (CT) of abdomen and pelvis revealed a soft tissue mass at the left lateral wall of the rectum, mild perirectal nodularity on the left lateral wall, and small lymph node on right side. Subsequently, she underwent colonoscopy for better visualization which demonstrated a 3 mm rectal sessile polyp (Figure 1) which was excised.
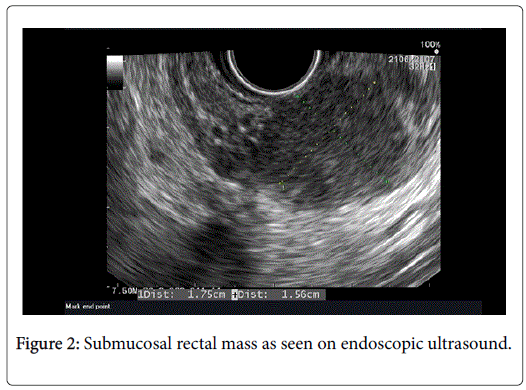
Also, there were multiple extraluminal rectal masses 10 cm from the anal verge on digital exam. Subsequently, an Endoscopic Ultrasound (EUS) guided Fine Needle Aspiration (FNA) was obtained from the submucosal masses which measured about 2 cm on ultrasound (Figure 2).
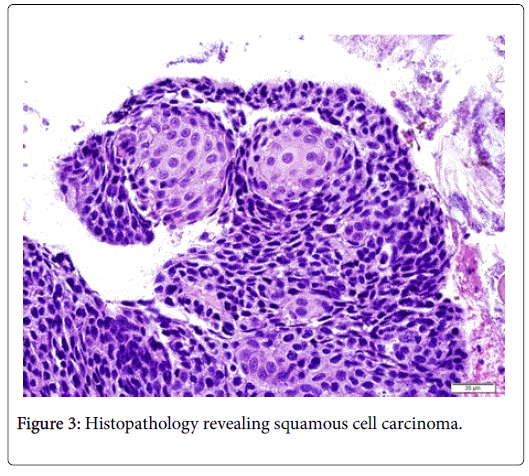
Histopathology revealed the mass to be squamous cell carcinoma (Figure 3) and the polyp to be hyperplastic polyp. Her Positron Emission Tomography (PET)/CT showed a hypermetabolic rectal lesion consistent with a known malignancy with additional foci of hypermetabolism in the perirectal fat which appeared to represent nodal disease without distant metastases. Pap smear was obtained and a primary gynecological malignancy was ruled out.
Given the locally advanced disease (stage III-A, T2N1M0), the patient was started on radiation therapy followed by chemotherapy with 5 fluorouracil and mitomycin. The patient responded well to the treatment and now being monitored with EUS.
Discussion
Colorectal cancer is a relatively common entity with 97% comprised of adenocarcinomas and rest 3% comprised of less common forms including lymphoma, squamous cell carcinoma, neuroendocrine tumor, and sarcoma. Rectal squamous carcinoma is an extremely rare entity with incidence of 0.1 to 0.3% and the sub-mucosal variety with intact mucosa being less common [1].
The etiopathogenesis is not well understood. Some theories regarding its pathogenesis include the following:
• Chronic injury from various stressors may lead to squamous metaplasia (Reversible change) which inturn may lead to dysplasia and consequentially SCC [2].
• HPV infection may lead to inactivation of Rb gene (tumor suppressor) which may inturn lead to SCC. This is also consistent with pathogenesis in Anal SCC [3].
• Embryonic ectopic nest of ectodermal cells (from cloacal remnant at the ano-recal transition zone; anal duct) in rectum which transform into squamous carcinoma [4] and finally
• Differentiation of pre-existing adenomas to squamous component [5].
Some risk factors have been associated with the rectal SCC. Case reports described rectal SCC in patients with chronic ulcerative colitis [1,6], Human Papilloma Virus (HPV) infection [3,7], Human Immunodeficiency Virus (HIV) [3,7,8], diffuse large B cell lymphoma [8] and Common Variable Immune Deficiency (CVID) [9]. However, in most instances associations are limited to single case report.
Like any large intestinal malignancy, endoscopy is the mainstay best modality for evaluation and diagnosis of rectal tumors. In addition to conventional endoscopic approach, EUS provides the ability to stage the tumor by evaluation for depth of tumor, local spread and lymph node involvement with possibility of tissue sampling [10]. With the advent of imaging modalities: CT, MRI and PET of chest, abdomen, and pelvis; patients can be evaluated for local as well as distant spread [10,11]. Both primary and metastatic diseases have shown Fluorodeoxyglucose (FDG) avidity for detection by PET [11]. There is no diagnostic role for HPV testing, immuno-phenotyping or genetic testing for this disorder. With the advancement in targeted therapies, as for some other malignancies, these types of testing may play a greater role in the future.
In 1979, a pre-requisite criterion for the diagnosis of Rectal SCC was formulated; it remains relevant and is follows [5]:
• Absence of other sites SCC to rule out possibility of metastasis.
• Absence of fistula lined by squamous epithelium.
• Exclusion of extension to rectum from anal canal SCC.
Multiple approaches have been employed for treatment of rectal SCC in the past. The approach most often employed included use of chemotherapy, radiotherapy, surgery. Each of these modalities has been tried individually and in conjunction with others in combination treatment with different temporal relationships [12]. Success has been documented with almost all possible combinations of above modalities [12-17]. Surgery was traditionally used in concordance with treating anal canal SCC.
However, recently there has been a shift in the standard of care for anal canal SCC to chemo-radiation. There has also been similar shift in preference towards definitive chemo-radiation for Rectal SCC [15,16,18,19]. A systematic review comparing chemo-radiation with traditional surgical approach demonstrated an overall survival of 86% in the chemoradiation group vs. 48% in surgery group. But the study also demonstrated local recurrence in 25% vs. 10% and metastatic rate in 30% vs. 13% in chemo-radiation compared with the traditional surgery group [16]. Recurrent and metachronous rectal SCC lesions have also been documented in the past [13,20]. This leads to a question of the recommended surveillance protocol following the initial management.
In summary, rectal squamous cell carcinoma continues to be a rare but distinct entity described in multiple individual case reports. Due to its rare occurrence, the literature lacks extensive information on risk factors, pathogenesis, and management. The literature to date is minimal but indicates that the treatment plan should be individualized according to the patient’s presentation. There is much to be explored by means of research into this narrow field of malignancy including for role of targeted management.
References
- Kang H, O'Connell JB, Leonardi MJ, Maggard MA, McGory ML, et al. (2007) Rare tumors of the colon and rectum: A national review. Int J Colorectal Dis 22: 183-189.
- Woods WG (1987) Squamous cell carcinoma of the rectum arising in an area of squamous metaplasia. Eur J Surg Oncol 13: 455-458.
- Matsuda A, Takahashi K, Yamaguchi T (2009) HPV infection in an HIV-positive patient with primary squamous cell carcinoma of rectum. Int J Clinical Oncol 14: 551-554.
- Grinvalsky HT, Helwig EB (1956) Carcinoma of the anorectal junction. I. Histological considerations. Cancer 9: 480-488.
- Williams GT, Blackshaw AJ, Morson BC (1979) Squamous carcinoma of the colorectum and its genesis. J Pathol 129: 139-147.
- Kulaylat MN, Doerr R, Butler B, Satchidanand SK, Singh A (1995) Squamous cell carcinoma complicating idiopathic inflammatory bowel disease. J Surg Oncol 59: 48-55.
- Konieczny N, Schwarze-Zander C, Hausen A (2013) HPV-related squamous cell carcinoma of the rectum in an HIV-positive patient: A rare differential diagnosis. Zentralblatt fur Chirurgie 138: e131-133.
- Choi H, Lee HW, Ann HW (2014) A case of rectal squamous cell carcinoma with metachronous diffuse large B cell lymphoma in an HIV-infected patient. Infect Chemother 46: 257-260.
- Goldberg A, Rose L, McCue P (2016) Common variable immunodeficiency disease and rectal squamous cell carcinoma: Acase report of a rare syndromic tumor type. J Gastrointest Cancer 47: 470-473.
- Dewhurst C, Rosen MP, Blake MA (2012) ACR appropriateness criteria pretreatment staging of colorectal cancer. J Am Coll Radiol 9: 775-781.
- Wang ML, Heriot A, Leong T, Ngan SY (2011) Chemoradiotherapy in the management of primary squamous-cell carcinoma of the rectum. Colorectal Dis 13: 296-301.
- Nahas CS, Shia J, Joseph R (2007) Squamous-cell carcinoma of the rectum: A rare but curable tumor. Dis Colon Rectum 50: 1393-1400.
- Brammer RD, Taniere P, Radley S (2009) Metachronous squamous-cell carcinoma of the colon and treatment of rectal squamous carcinoma with chemoradiotherapy. Colorectal Dis 11: 219-220.
- Theodosopoulos TK, Marinis AD, Dafnios NA (2006) Aggressive treatment of metastatic squamous cell carcinoma of the rectum to the liver: A case report and a brief review of the literature. World J Surg Oncol 4: 49.
- Peron J, Bylicki O, Laude C, Martel-Lafay I, Carrie C, et al. (2015) Nonoperative management of squamous-cell carcinoma of the rectum. Dis Colon Rectum 58: 60-64.
- Guerra GR, Kong CH, Warrier SK, Lynch AC, Heriot AG (2016) Primary squamous cell carcinoma of the rectum: An update and implications for treatment. World J Gastrointest Surg 8: 252-265.
- Wang JF, Wang ZX, Xu XX, Wang C, Liu JZ (2014)Primary rectal squamous cell carcinoma treated with surgery and radiotherapy. World J Gastroenterol 20: 4106-4109.
- Clark J, Cleator S, Goldin R, Lowdell C, Darzi A, et al. (2008) Treatment of primary rectal squamous cell carcinoma by primary chemoradiotherapy: Should surgery still be considered a standard of care? European J Cancer 44: 2340-2343.
- Musio D, De Felice F, Manfrida S (2015) Squamous cell carcinoma of the rectum: The treatment paradigm. European J Surg Oncol 41: 1054-1058.
- Hogan NM, Leonard G, Sheehan M, Joyce MR (2013) Early recurrence and progression of a rare rectal squamous cell carcinoma after initial response to primary chemoradiotherapy. Tumori 99: e88-90.
Citation: Sethi P, Aloreidi K, Elnair R, Yousif U, Atiq M, et al. (2017) Rare Primary Sub-Mucosal Rectal Squamous Cell Carcinoma Diagnosed with Endoscopic Ultrasound: Case Report and Literature Review. J Gastrointest Dig Syst 7: 535. DOI: 10.4172/2161-069X.1000535
Copyright: © 2017 Sethi P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5198
- [From(publication date): 0-2017 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 4330
- PDF downloads: 868