Rapidly Progressive Dementia (RPD) in the Setting of Therapeutic Lithium Levels
Received: 27-Feb-2023 / Manuscript No. JADP-23-87658 / Editor assigned: 01-Mar-2023 / PreQC No. JADP-23-87658 (PQ) / Reviewed: 15-Mar-2023 / QC No. JADP-23-87658 / Revised: 22-Mar-2023 / Manuscript No. JADP-23-87658 (R) / Published Date: 30-Mar-2023 DOI: 10.4172/2161-0460.1000566.
Abstract
Rapidly Progressive Dementias are characterized by a subacute or acute decline in neurologic function and causes run the gamut from easily reversible to universally fatal. The sudden onset and abrupt decline are distressing for patients and caregivers and present a unique challenge for clinicians. In the absence of readily apparent cause, many will move to a presumptive diagnosis of prion diseases is a diagnosis which can only be confirmed after death. In patients taking neurotoxic medications, to include such routine medications as lithium, tricyclic antidepressants, or even bismuth-based antacids, a ‘medication vacation’ should be considered to rule out an iatrogenic cause. Based on numerous case reports, a ‘vacation’ is still recommended in the setting of therapeutic serum medication levels.
Keywords: Stockton-Brown M (2023) Rapidly Progressive Dementia (RPD) in the Setting of Therapeutic Lithium. J Alzheimers Dis Parkinsonism. 13:566.
Introduction
Lithium salts, while highly effective in the treatments of psychiatric disorders, have an extremely tight therapeutic index. When serum lithium levels rise too high patients risk lithium toxicity and life changing or threatening complications. In some patients, however, evidence of lithium toxicity can be seen even with therapeutic serum levels. Here we discuss the case of a patient with bipolar disorder presenting with rapidly progressive dementia in the setting of recent inpatient psychiatric admission and initiation of lithium therapy. The initial clinical impression was consistent with prion disease and remained such after the patient’s labs (to include serum lithium levels) returned within normal limits. Therapeutic-level lithium toxicity was only considered only after a literature review showed several strikingly similar case reports.
Case Description
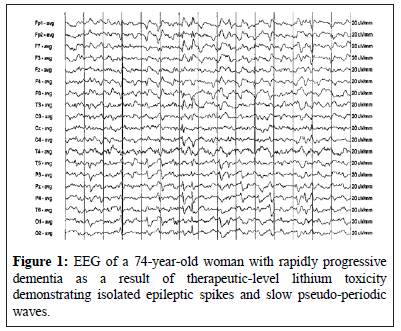
A 68-year old man with several months of waning cognition presents to the ED for acute worsening of his symptoms. His medical history was significant for a seven-year history of bipolar disorder (type 1) and an inpatient psychiatric stay six months prior for a manic episode. At that time carbamazepine was discontinued in favor of lithium and quetiapine (seroquel). The patient is a Caucasian male with a 10th grade education. He is a retired fisherman with a history of chronic back pain (status post lumbar fusion) with a childhood history of dyslexia. Patient’s partner reports he is very active, rising every morning at 0530 to care for the property and pets. He very occasionally smokes marijuana and drinks alcohol though not in the last six months. He has no history of suicide attempts or violent behavior. Since returning home from his psychiatric admission the patient experienced severe lethargy. Quetiapine was discontinued without significant improvement. The patient’s symptoms continued to worsen, including forgetfulness, increasingly unsteady gait, and purposeless movements. Donezepil (aricept) and benztropine (cogentin) were prescribed without improvement. Shortly prior to presentation the patient experienced a precipitous decline including apraxia, hypersomnia, 15-pound weight loss, and new inappropriate behaviors, such as defecating in laundry baskets at home. On presentation, a neurological exam showed disorientation, dysarthria, myoclonus, asterixis, and palmomental reflex. Strength and reflexes were grossly intact. No evidence of nystagmus. Patient only intermittently followed commands. Initial labs were normal and lithium levels within therapeutic range (0.6 mEq/L). Imaging was unremarkable and Electroencephalogram (EEG) showed diffuse slowing with periodic sharp wave complexes (Figure 1). A lumbar puncture could not be obtained due to the patient’s history of lumbar fusion and resistance to the procedure. The patient was admitted for rapidly progressive dementia highly suspicious for Creutzfeldt-Jacob Disease (CJD), a fatal neurodegenerative prion disease. All home medications were discontinued. Medical decision making was deferred to the nextof- kin due to lack of capacity. Shortly after admission the patient tested positive for COVID-19 and was quarantined. Lumbar puncture with fluoroscopy was cancelled. The patient received regular diet and serial neurologic exams were performed. Over several days the patient’s mental status and disco ordination spontaneously improved. The patient regained capacity and left against medical advice. At one month the patient reported a complete resolution of symptoms. Neurology advised close follow-up and avoidance of lithium.
Results And Discussion
RPD is a complex clinical picture with a wide differential, including metabolic, toxic, and iatrogenic causes. The toxic effects of lithium are typically seen at elevated levels, however case reports show ‘paradoxical lithium toxicity’ can occur at <1 mEq/L [1,2]. A patient may become ‘super sensitive’ at any point, though it is more common among the elderly [3]. The literature suggests that serum lithium levels may not accurately reflect brain lithium levels in all patients, leading some to develop neurotoxicity despite normal labs1. One report describes 70-year-old patient with bipolar disorder who was successfully treated with lithium for 40 years before developing symptoms of RPD. It was only once the patient was deemed terminal and all medications were withdrawn that her RPD improved (and lithium was identified as the offending agent) [1]. Another paper reports a similar case in a woman who had been treated with lithium for 15 years [4]. The mechanism by which lithium causes neurotoxicity or by which patients become ‘super sensitive’ (particularly those that are not naïve to lithium) is not understood. Lithium is known to affect neuronal Na+/K+ ATPase pumps (at low levels lithium activates pumps and at higher levels it inhibits them) as well as the balance of other cations [5]. The normal aging process leads to a loss in brain volume by approximately 5% for each decade after 40 [6]. It is possible that this volume loss leads to higher lithium concentrations in the brain versus those reflected in the serum. Decreased intraneuronal fluid volume may leave older brains more sensitive to shifts in intra vs. extracellular ions due to the impacts on resting membrane potential. Age-related volume loss as a mechanism for sensitization would also help to explain why some patients develop neurotoxicity despite years of successful lithium treatment-the medication didn’t change, but the make-up of the patient’s brain did. In patients with lithium-related RPDs the literature reports EEGs with diffuse slowing [7-10] and Positron Emission Tomography (PET) scans with markedly decreased metabolic activity, particularly in the parietal lobes [8]. A theoretical lithium-related disturbance of resting membrane potential would be consistent with these findings. Patients with other medical problems or who take multiple medications (both commonly seen in older adults) are also at higher risk for lithium toxicity [2].
Of the numerous case studies this author read discussing lithiumrelated RPD, all of the patients had a presumptive diagnosis of CJD/ prion disease based on their clinical picture. Given the wide differential for RPD and the low prevalence of CJD/prion disease in the general populations, it seems clinicians’ cognitive biases may play a role here. RPD causes are includes:
Autoimmune
Antibody-mediated dementia/encephalopathy, CNS lupus, Acute disseminated encephalomyelitis (AOEM), Hashimoto encephalopathy (steroid responsive encephalopathy associated with autoimmune thyroiditis (SREATJ)) and Other CNS Vasculitides.
Atrogenic
Medication toxicity (eg. Lithium, methotrexate, chemotherapy) and Illicit drug use.
Metastases/neoplasm related
Paraneoplastic diseases-limbic encephalopathy, Metastases to CNS, Primary CNS lymphoma, lntravascular lymphoma, Gliomatosis cerebri, Metastatic encephalopathy and Carcinomatous meningitis.
Neurodegenerative
Prion disease, Alzheimer disease, Dementia with lewy bodies, Frontotemporal dementia and Corticobasal degeneration.
Vascular/ischemic
Multi infarct, Thalamic or callosum infarct, Cerebral amyloid angiopathy, Dural arteriovenous fistulas, CNS Vasculitis, Venous thrombosis, Cerebroretinal microangiopathy with calcifications and cysts, Posterior reversible encephalopathy syndrome and Subacute diencephalalic angioencephalopathy.
Infectious
Viral encephalitis, including herpes simplex virus, HIV Dementia, Progressive multifocal leukoencephalopathy, Fungal infections (eg. CNS aspergillosis, coccidioidomycosis), Amoebic infection (eg. Balamuthia, mandrillaris), Spirochete infection, Lyme disease (rarely encephalopathy), Whipple disease (rarely rapid), Subacute sclerosing panencephalitis (young adults) and Urinary tract infection. pneumonia in elderly patient or patient with mild dementia.
Toxic metabolites
Electrolyte disturbances (sodium, calcium, magnesium, phosphorus), Endocrine abnormalities (thyroid, parathyroid, adrenal), Extrapontine myelinolysis, Vitamin B12 (cyanocobalamin) deficiency, Vitamin B1 (thiamine) deficiency (Wemicke encephalopathy), Niacin deficiency (not usually rapid), Folate deficiency (dementia rare), Uremic encephalopathy, Portosystemic shunt encephalopathy, Poikilothermia, Hepatic encephalopathy, Acquired hepatocerebral degeneration, Hypoxia/hypercarbia, Hyperglycemia/ hypoglycaemia, Porphia, Metaltoxicity (bismuth, lithium, mercury, manganese Parkinsonism) and Mitochondrial disease (eg. Mitochondrial myopathy, encephalopathy, lactic acidosis and stroke like episode syndrome [MELASJ]) (Figure 1).
As per behavioral economists Kahnemann and Tversky the availability heuristic leads humans to recall things that are more recent, novel, or striking over that which is less interesting, though perhaps more common [8]. But as has been said many times, and should be kept in mind under these circumstances, ‘Common things are common’. In a 2016 article on the subject Dr Michael Geschwind states that as the ‘protoypical RPD’ CJD is the first diagnosis most neurologists consider [9]. In his 1992 article, “Drug-Induced Creudtzfeldt-Jacob like Syndrome” Pasquel Finelli discusses a patient in his care, along with 7 published reports of presumptive CJD. All were later discovered to be medication-induced neurotoxicity (6 lithium, 1 tricyclic antidepressant, and 1 unspecified polypharmacy). In the discussion section, Finelli bemoans the fact that the primary teams had run only limited testing and then quickly jumped to CJD without considering toxic medications [10]. Similar to our patient’s case the offending agent was only discovered after incidental discontinuation of home medications. In a subsequent article penned by Geschwind and colleagues at UCSF of the 825 RPD patients referred to them-most of whom had already received presumptive diagnoses of CJD-only about half confirmed to have a prion disease [11]. The rest were attributable to other causes, many of which were reversible. Prion diseases are dramatic and interesting-and even in the recent memory of the author of this paper-make a much bigger impression on undergraduates and medical trainees than a lengthy, detailed list of different neurotoxic agents/illnesses. As such, it is essential we broaden our differential, lest we overlook the lessmemorable possibilities.
Patients with psychiatric illness, particularly bipolar disorder, are at increased risk of developing dementia and evidence seems to indicate lithium has a neuroprotective effect for patients who tolerate it well [12]. Lithium-related RPD can easily be mistaken for other forms of dementia, as evidenced by this patient’s recent trials of donepezil (Aricept) and benztropine (Cogentin). These factors, combined with other psychosocial and socioeconomic obstacles, make challenging to identify the cause of acute or subacute cognitive decline in this patient population. While the patient in our case was lucky, some do experience irreversible neurologic damage as a result of chronic lithium toxicity, known as Syndrome of Irreversible Lithium Effectuated Neurotoxicity (SILENT). As such, it may be advisable that patients treated with lithium who present with new neurological symptoms promptly discontinue the medication (even with therapeutic serum levels) so that it may be ruled in or out as a potential cause.
Conclusion
Prevalence of RPDs in the general population is extremely low and they are most likely to occur in medically complex older patients. Given the limited number of cases they will encounter in their careers and the extremely wide differential that must be considered, identifying the specific cause of a patient’s RPD can be very challenging, even for experienced neurologists. In this setting, it is important that toxic and iatrogenic causes not be overlooked. The literature shows a number of cases of RPD caused by appropriatelydosed lithium therapy, though other medications and exposures should also be considered as offending agents before diagnosing a terminal illness.
References
- Geschwind MD, Haman A, Miller BL (2007). Rapidly progressive dementia. Neurol Clin 25(3):783-807.
[Crossref][Google Scholar] [PubMed]
- Farina E, Giani L, Lovati C, Mariani C, Nemni R (2017). Lithium in the Normal Therapeutic Range: A Potential Sneaky Danger for the Brain. A Case of Slow Tricking Neurotoxicity and a Brief Overview of Literature. J Alzheimers Dis Parkinsonism 7(407):2161-0460.
- Iorgoveanu C, Zaghloul A, Donisan T, Balanescu DV, Balakumaran K, et al (2019). Atypical arrhythmia associated with lithium therapy: when to expect the unexpected. Acta Cardiologica Sinica 35(2):179-179.
[Crossref][Google Scholar] [PubMed]
- Mignarri A, Chini E, Rufa A, Rocchi R, Federico A, et al (2013). Lithium neurotoxicity mimicking rapidly progressive dementia. J Neurol 260:1152-1154.
[Crossref][Google Scholar] [PubMed]
- Smith SJ, Kocen RS (1988). A Creutzfeldt-Jakob like syndrome due to lithium toxicity. J Neurol Neurosurg Psychiatry 51(1):120-123.
[Crossref][Google Scholar] [PubMed]
- Markov NT, Lindbergh CA, Staffaroni AM, Perez K, Stevens M, et al (2022). Age-related brain atrophy is not a homogenous process: Different functional brain networks associate differentially with aging and blood factors. Proc Natl Acad Sci USA 119(49):2207181119-2207181119.
[Crossref][Google Scholar] [PubMed]
- Mecê AM, Abreu VC, Lamas GM, Tacla RD, Minekawa TB, et al (2022). Lithium Intoxication as a cause of reversible dementia mimicking FDG PET features of Alzheimer’s disease. Dement Neuropsychol 16:249-252.
[Crossref][Google Scholar] [PubMed]
- Tversky A, Kahneman D (1973). Availability: A heuristic for judging frequency and probability. Cogn Psychol 5(2):207-232.
- Geschwind MD (2016). Rapidly Progressive Dementia. Continuum (Minneap Minn 22(2):510-537.
[Crossref][Google Scholar] [PubMed]
- Finelli PF (1992). Drug-induced Creutzfeldt-Jakob like syndrome. Journal of Psychiatry and Neuroscience 17(3):103-103.
[Google Scholar] [PubMed]
- Geschwind MD, Haman A, Miller BL (2007). Rapidly progressive dementia. Neurol Clin 25(3):783-807.
- Velosa J, Delgado A, Finger E, Berk M, Kapczinski F, et al (2020). Risk of dementia in bipolar disorder and the interplay of lithium: a systematic review and meta-analyses. Acta Psychiatr Scand 141(6):510-521.
[Crossref][Google Scholar] [PubMed]
Citation: Stockton-Brown M (2023) Rapidly Progressive Dementia (RPD) in the Setting of Therapeutic Lithium. J Alzheimers Dis Parkinsonism. 13:566. DOI: 10.4172/2161-0460.1000566.
Copyright: © 2023 Stockton-Brown M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1979
- [From(publication date): 0-2023 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 1634
- PDF downloads: 345