Research Article Open Access
Radical Surgery for Incidental Gallbladder Carcinoma. Which Subset of Patients is Really Suitable for?
Dario Borreca*, Francesco Balcet, Alberto Bona, Maurizio Bossotti and Paolo De Paolis
Department of General Surgery–“Gradenigo” Hospital, Turin, Italy
- *Corresponding Author:
- Dario Borreca
Via Cardinale Caprara, 36 - 00167 Rome, Italy
Tel: +39 328 3390199n
Fax: +39 06 6624818
E-mail: d.borreca@policlinicoumberto1.it
Received date: August 10, 2015 Accepted date: August 28, 2015 Published date: September 5, 2015
Citation: Borreca D, Balcet F, Bona A, Bossotti M, Paolis PD (2015) Radical Surgery for Incidental Gallbladder Carcinoma. Which Subset of Patients is Really Suitable for?. J Gastrointest Dig Syst 5:328. doi:10.4172/2161-069X.1000328
Copyright: © 2015 Borreca D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: There is a wide consensus on the fact that surgical treatment of incidental gallbladder carcinoma should be based according to T stage: while simple cholecystectomy is considered an adequate treatment for confined carcinomas to the lamina propria (T1a), it is still being discussed in the case of cancer limited to muscularis mucosae (T1b), and a secondary extended resection is the only curative option for tumors invading the perimuscolar connective tissue (T2), and seems to improve survival in selected advanced cases. However, it is still not clear which subset of patients is really suitable for aggressive reoperations, and their effective impact on the prognosis of incidental neoplasm. The purpose of this study is to evaluate these aspects in a retrospective review of gallbladder carcinomas diagnosed during or after 9284 cholecystectomies performed with a benign indication. Methods: From January 1995 to December 2014, 46 cancers were found. In 35 of these, an invasion beyond the lamina propria was detected. Due to clinical reasons, 17 out of these 35 patients had no further operation after cholecystectomy. Among the 18 reoperated patients, 11 had no residual disease at final pathologic examination. Results: Considering only T2 and T3 cancers, survival was improved in patients undergone a re-resection, but this result is statistically significant (p=0.01) only if a macroscopic residual disease was absent. Conclusions: If an acceptable mortality and morbidity are evaluated, an additional radical operation is justified, inasmuch as it is the best chance for long-term relapse-free survival. Nevertheless, the subset of patients which have a real benefit from this treatment is small and the better prognosis of incidental gallbladder carcinoma is probably still due to the large number of initial disease (T1a: 25% in our case series) rather than to secondary aggressive resection.
Keywords
Cholecystectomy; Carcinoma; Gallbladder; Incidental; Indication
Introduction
Gallbladder adenocarcinoma is a rare tumor, but it’s burdened by a poor prognosis: long-term survival reported in literature is about 5% at 5 years [1]. Currently, about two thirds of cases are an incidental finding after the removal of the gallbladder for a benign disease [2]. This situation may result, in relation to the wall depth invasion, in a need for a second surgical operation, which consists in the exeresis of liver segments V and IVb for a depth of 3 cm (Glenn’s procedure), associated with lymphadenectomy of the hepatoduodenal ligament, biopsy and eventual main bile duct resection [3]. This action is proposed, according to the majority of authors, since T2 stage and beyond [4], while it is still being discussed in cancers limited to muscularis mucosae (T1b) [5,6]. At the incidental carcinoma of the gallbladder is generally attributed a better prognosis than suspected preoperatively one, but it is not clear whether this is due to the actual feasibility of a second surgical procedure or to the presence of an early lesions for which a simple cholecystectomy is adequate. It should be noted that, because of a few-symptoms course, even incidental tumors comprise a small proportion of advanced lesions for which an R0 radicalization is difficultly executable. In fact, among patients sent to the operating theatre, are described resectability percentages even lower than 50% [7,8] due to an undiagnosed hepatic and, especially, peritoneal spreading, neither at previous cholecystectomy, neither using imaging techniques, overwhelmed with a postoperative complication rate up to 30-40% [8,9] even in recent publications. The aim of our study is to retrospectively evaluate the actual feasibility of a second surgery, and the impact on overall prognosis in our case series of incidental gallbladder carcinoma.
Materials and Methods
Since 1/1/1995 to 31/12/2014 out of 9284 cholecystectomies performed in 2 surgery services (Department of General Surgery VII OSG Battista, Turin and Surgery Division O. Gradenigo, Torino) were observed 46 incidental gallbladder carcinomas, recognized at the first surgical intervention performed for benign lesions (unsuspected tumors: 9 cases) or at the next histological examination (latent or inapparent tumors: 34 cases, to which are added a further 3 cases, came to our attention after cholecystectomy performed in other Institutions). These 46 patients were reviewed, 29 women and 17 men with a mean age of 67 years (range 59-90). In 45 cases the presence of cholelithiasis and its complications were the surgical indications for cholecystectomy (7 patients had an history of repeated episodes of acute cholecystitis and 4 of them took place in emergency room for empyema); in one case the indication for surgery was motivated by the presence of a broad-base polyp. Cholecystectomy was performed 16 times in a laparoscopic setting, while in 28 in a laparotomic fashion (10 of which are outcomes of a laparoscopic conversion). In the remaining 2 cases, it was not decided to perform the gallbladder exeresis due to the presence of peritoneal carcinomatosis. The histological result was always an adenocarcinoma except one case of squamous cell carcinoma. The latter was, however, included in our series, as this histological type does not have a different prognostic significance [10]. The 46 tumors were classified according to the UICC TNM system 7th edition and thus divided depending on invasion depth (Table 1).
| UICC T staging | Patients |
|---|---|
| Tis-T1 | 13 |
| T2 | 18 |
| T3 | 13 |
| Txa | 2 |
Table 1: Summary of examinated cases, stratified by UICC T parameter. aPatients with peritoneal carcinomatosis at laparoscopic exploration, who did not undergo to completion of cholecystectomy.
Before a possible second surgical radicalization, was routinely performed a CT scan of thorax and abdomen. The applied radicalization procedure consists in removal of liver segments V and VIb, with hepatoduodenal ligament lymph node dissection, associated with excision of the trocar scars, in case of a previous laparoscopic surgery; resection of the bile duct is performed only in the presence of a positive sampling of the cystic stump (this event did not occur in our series). Data related to clinical outcomes were obtained for all 46 patients. The mean follow-up is 45 months (range 2-221). Survival curve was calculated using Kaplan-Meier method. The differences between the curves were evaluated with the Log-Rank Test. A p value <0.05 was considered statistically significant.
Results
Overall, 18 patients were re-operated, of which 2 were T1 (due to histological Mascagni node positivity in a T1a patient, and finding of T1b in a second), 13 T2, 3 T3.
Only one of the 9 patients with intraoperative detection has undergone radicalization, although we have always proceeded to laparotomic conversion. In fact, a case was a carcinoma in situ arising out of an adenomatous polyp, in another 3 there was a significant peritoneal metastatic spread, and in further 4 cases advanced age (>75 aa) has not recommended the extent of the surgical procedure.
Among the 18 patients brought back to the operating theatre, the Glenn’s radicalization was executed 15 times, while in a T2 patient, surgery was limited to the hepatoduodenal ligament skeletonization due the important nodal involvement and the presence of metastases in the left liver; in an additional T2 was detected an important peritoneal spread, not previously highlighted, that allowed only a diagnostic biopsy. In the unique T1b, in addition to the hepatic pedicle dissection, was performed gallbladder bed exeresis.
Reoperation was achieved within 40 days from cholecystectomy, except for a patient referred from another Institution.
In-hospital mortality rate was 0%, while postoperative complications were recorded in 4 patients (22%): a biliary collection drained by ultrasound guidance (Dindo-Clavien grade IIIa), two pleural effusions (Dindo-Clavien grade I) and an episode of transient liver failure with raised cytolysis markers (Dindo-Clavien grade IV), spontaneously resolved.
Among the 15 radicalized patients, there was no evidence for residual disease in 9 cases: 2 T1, 6 T2, 1 T3. Histological diagnosis was otherwise positive in the other 6: detection of trocar metastasis on the right side and on the gallbladder bed in a T2, liver and nodal involvement in a second T2, nodal localization in further 2 T2 patients, and liver metastasis in a T3.
We performed routine removal of the trocar scar in all cases of previous laparoscopic cholecystectomy, noticing the presence of secondariness in 2 cases out of 9 (22%). In one case it was a patient transferred from another institution and radicalized after 120 days since cholecystectomy, although it is outside the criteria proposed by Wise and Suzuki [11], which set up the limit for reoperation respectively at 3 and 2 months.
Discussion
The finding of an incidental carcinoma occurs with a frequency ranging between 0.2 to 2.9% in literature [7]. CAES registry, which comprises 117.840 laparoscopic cholecystectomies, identified 409 (0.35%) incidental carcinomas, and this data is confirmed in our experience, with an incidence rate of 0.49%.
It should be emphasized how the prognosis of an incidental cancer, although better than preoperative suspected one, it is still modest: reported survivals at 5 years in the literature are, respectively, 35% vs. 5%, with a median of 26.5 vs. 9.2 months in suspected cases [1].
Results of our series are slightly better (median: 37 months), but prognosis of unsuspected cancers seems daunting: in this group, it has been possible to radicalize only a single case out of 15 lesions >T1 and the median overall survival has not exceeded 6 months, versus 37 months of the unapparent forms (p=0.007). In addition, while patients with in-situ and intramucosal carcinomas are all alive after a mean follow-up of 69 months, T2 and T3 lesions showed, overall, an unsatisfactory prognosis with a median of 19 and 5 months for the two groups, respectively; these findings coincide with those reported by many authors[7,8,12-25].
Firstly, owing to the early nodal and liver spreading, in the literature are described resectability rate even lower than 50%: Toyanaga [7] could perform radicalizations in only 21 out of 50 cases of T2 and T3 carcinomas; Fong [8] in a series of 41 T2, T3 and T4 incidental tumors reported 21 cases of non-operability (only 5 diagnosed with preoperative imaging techniques) due to peritoneal metastases, liver infiltration, portal involvement or retropancreatic nodal spread. Furthermore, the frequent occurrence of the gallbladder carcinoma in the seventh and eighth life decade [3] (8 patients in our group are more than 75 years old) could make problematic the indication to a demanding surgical procedure comprising an extended liver resection and nodal dissection, in which are described postoperative complication rates up to 30-40% [8,9], even in the more recent literature [13-25].
In our case series, in 17 out of 35 locally advanced carcinomas >T1a (48%) ,we could not perform radicalization due to comorbidities and age >75 aa (13 cases), or tumoral extension to the liver and peritoneum (4 cases, one of which detected only at the operating theatre).
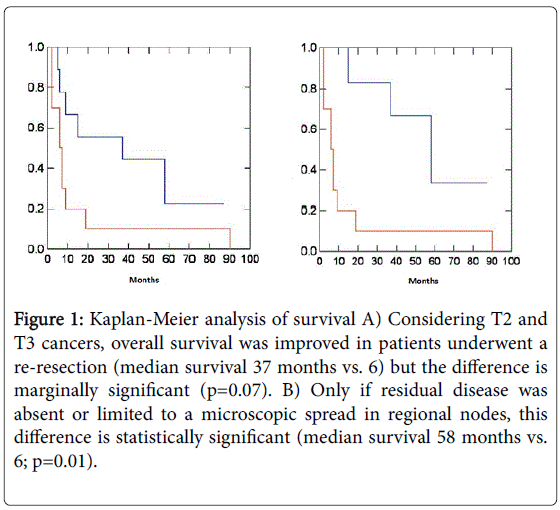
Regarding to actually radicalized tumors, Capussotti [9], in a case series of T2 carcinomas showed a significant survival improvement only in shortly-reoperated patients after cholecystectomy (median 2.2 weeks) and without preoperative evidence of macroscopic residual tumor. It could be interesting to note how this subgroup includes a non-negligible fraction (37%) of cases entirely without residual tumor at reoperation. Our experience coincides with these considerations (Figure 1) in only 4 out of 13 T2 (30%) residual tumor was histologically proven; moreover, radicalized T2 and T3 tumors exhibit a significantly better prognosis compared to the corresponding nonreoperated one (median survival: 37 months vs. 6), and this difference is at the limits of statistical significance (p=0.04); considering only the no-residual subgroup, this difference becomes more significant (median survival: 58 vs. 6 months, p=0.01).
Figure 1: Kaplan-Meier analysis of survival A) Considering T2 and T3 cancers, overall survival was improved in patients underwent a re-resection (median survival 37 months vs. 6) but the difference is marginally significant (p=0.07). B) Only if residual disease was absent or limited to a microscopic spread in regional nodes, this difference is statistically significant (median survival 58 months vs. 6; p=0.01).
Conclusions
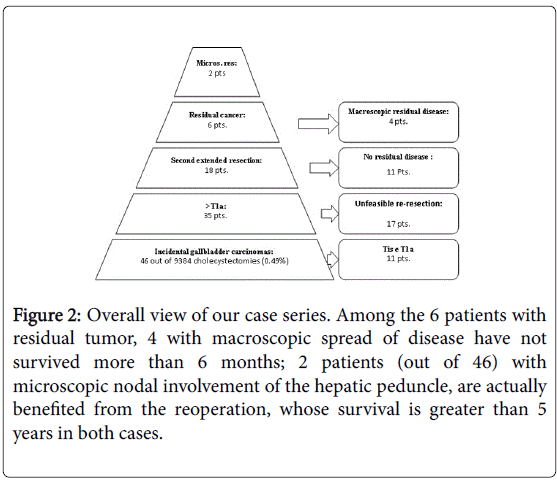
In our experience, best survival rate in incidental carcinomas compared to suspicion carcinomas one, seems mainly related to the presence of an important rate of early malignancies (11 out of 46 patients: 25%), where the simple cholecystectomy is considered sufficient, rather than the real effectiveness of a second radicalizing surgical procedure. Although the latter has allowed an overall survival improvement in resected patients, it was proved to be slightly incisive on the natural history of the disease (Figures 1 and 2) out of 46 incidentally diagnosed carcinomas in a series of 9284 cholecystectomies, a reoperation resulted not necessary in 11 patients (carcinoma in situ and T1a stage), not feasible in other 17 (age, comorbidities, peritoneal spreading), not useful in further 11 (residual tumor absence). Among the 6 patients with residual tumor, 4 with macroscopic spread of disease have not survived more than 6 months; 2 patients (4%) with microscopic nodal involvement of the hepatic peduncle, are actually benefited from the reoperation, whose survival is greater than 5 years in both cases. Waiting the diagnostic imaging progress, allowing the exclusion of the advanced forms and the patients without residual tumor, the usefulness of a second surgical act, albeit performed on a limited and well-established subset of patients, will have to contend with a significant percentage of impractical or ineffective interventions.
Figure 2: Overall view of our case series. Among the 6 patients with residual tumor, 4 with macroscopic spread of disease have not survived more than 6 months; 2 patients (out of 46) with microscopic nodal involvement of the hepatic peduncle, are actually benefited from the reoperation, whose survival is greater than 5 years in both cases.
References
- Goetze T, Paolucci V (2006) Does laparoscopy worsen the prognosis for incidental gallbladder cancer?below Surg Endosc 20: 286-293.
- Wullstein C, Woeste G, Barkhausen S, Gross E, Hopt UT (2002) Do complications related to laparoscopic cholecystectomy influence the prognosis of gallbladder cancer?below Surg Endosc 16: 828-832.
- Fong Y, Kermeny N, Lawrence TS (2001) Cancer of the liver and biliary tree. In: cancer principles and practice in oncology. Philadelphia, Lippincott 1162-1203.
- Shirai Y, Yoshida K, Tsukada K, Muto T (1992) Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy.below Ann Surg 215: 326-331.
- Wagholikar GD, Behari A, Krishnani N, Kumar A, Sikora SS, et al. (2002) Early gallbladder cancer.below J Am Coll Surg 194: 137-141.
- Ouchi K, Sugawara T, Ono H, Fujiya T, Kamiyama Y, et al. (1999) Diagnostic capability and rational resectional surgery for early gallbladder cancer.below Hepatogastroenterology 46: 1557-1560.
- Toyonaga T, Chijiiwa K, Nakano K, Noshiro H, Yamaguchi K, et al. (2003) Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma.below World J Surg 27: 266-271.
- Fong Y, Heffernan N, Blumgart HL (1998) Galbladder carcinoma discovered during laparoscopic cholecystectomy. Aggressive resection is beneficial. Cancer 83: 423-427.
- Muratore A, Amisano M, Viganò L, Massucco P, Capussotti L (2003) Gallbladder cancer invading the perimuscular connective tissue: results of reresection after prior non-curative operation.below J Surg Oncol 83: 212-215.
- Misra MC, Guleria S (2006) Management of cancer gallbladder found as a surprise on a resected gallbladder specimen.below J Surg Oncol 93: 690-698.
- Wise PE, Shi YY, Washington MK, Chapman WC, Wright JK, et al. (2001) Radical resection improves survival for patients with pT2 gallbladder carcinoma.below Am Surg 67: 1041-1047.
- Paolucci V, Neckell M, Götze T; Workgroup Surgical Endoscopy, German Society of Surgery (2003) [Unsuspected gallbladder carcinoma--the CAE-S/CAMIC registry].below Zentralbl Chir 128: 309-312.
- Goetze TO, Paolucci V (2013) Prognosis of incidental gallbladder carcinoma is not influenced by the primary access technique: analysis of 837 incidental gallbladder carcinomas in the German Registry.below Surg Endosc 27: 2821-2828.
- Butte JM, Kingham TP, Gönen M, D'Angelica MI, Allen PJ, et al. (2014) Residual disease predicts outcomes after definitive resection for incidental gallbladder cancer.below J Am Coll Surg 219: 416-429.
- Hueman MT, Vollmer CM Jr, Pawlik TM (2009) Evolving treatment strategies for gallbladder cancer.below Ann Surg Oncol 16: 2101-2115.
- Lendoire JC, Gil L, Duek F, Quarin C, Garay V, et al. (2012) Relevance of residual disease after liver resection for incidental gallbladder cancer.below HPB (Oxford) 14: 548-553.
- Shindoh J, de Aretxabala X, Aloia TA, Roa JC, Roa I, et al. (2015) Tumor location is a strong predictor of tumor progression and survival in T2 gallbladder cancer: an international multicenter study.below Ann Surg 261: 733-739.
- Dutta U (2012) Gallbladder cancer: can newer insights improve the outcome?below J Gastroenterol Hepatol 27: 642-653.
- (2014) National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Hepatobiliarycancers.
- Birnbaum DJ, Viganò L, Ferrero A1, Langella S1, Russolillo N1, et al. (2014) Locally advanced gallbladder cancer: which patients benefit from resection?below Eur J Surg Oncol 40: 1008-1015.
- Gil L, Lendoire J, Duek F, Quarin C, Garay V, et al. (2014) [Radical surgery for incidental gallbladder cancer: the value of a deferred pathological finding of residual disease].below Cir Esp 92: 168-174.
- Goetze TO, Paolucci V (2014) [Incidental T1b-T3 gallbladder carcinoma. Extended cholecystectomy as an underestimated prognostic factor-results of the German registry].below Chirurg 85: 131-138.
- Barreto SG, Pawar S, Shah S, Talole S, Goel M, et al. (2014) Patterns of failure and determinants of outcomes following radical re-resection for incidental gallbladder cancer.below World J Surg 38: 484-489.
- Cavallaro A, Piccolo G, Di Vita M, Zanghì A, Cardì F, et al. (2014) Managing the incidentally detected gallbladder cancer: algorithms and controversies.below Int J Surg 12 Suppl 2: S108-119.
- Fuks D, Regimbeau JM, Pessaux P, Bachellier P, Raventos A, et al. (2013) Is port-site resection necessary in the surgical management of gallbladder cancer?below J Visc Surg 150: 277-284.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14714
- [From(publication date):
October-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10187
- PDF downloads : 4527