Case Report Open Access
Pyogenic Granuloma of Buccal Mucosa: A Rare Case Report
N Rakesh*, Kuhu Majumdar, Yashoda Devi BK and Sujatha S Reddy
Department of Oral medicine, Diagnosis and Radiology, M.S. Ramaiah Dental College & Hospital, Bangalore
- Corresponding Author:
- N Rakesh MDS (Ph.D)
Department of Oral medicine
Diagnosis and Radiology
M.S.Ramaiah Dental College & Hospital, Bangalore
Karnataka, India
Tel: +919448507494
Fax: 23608136
E-mail: drnrakesh@gmail.com
Received date: June 27, 2014; Accepted date: August 4, 2014; Published date: August 11, 2014
Citation: N Rakesh, Kuhu Majumdar, Yashoda Devi BK and Sujatha S Reddy (2014) Pyogenic Granuloma of Buccal Mucosa: A Rare Case Report. J Interdiscipl Med Dent Sci 2:144. doi:10.4172/2376-032X.1000144
Copyright: © 2014 Rakesh, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Pyogenic granuloma is a common inflammatory hyperplasia of the oral cavity traditionally considered to be non neoplastic in nature. Its most common intraoral location is the gingiva and it is classically thought to arise due to either chronic irritation or hormonal influences. Extragingival sites are very rarely reported for this lesion and may tend to present a diagnostic dilemma to the clinician. Here we report one such case of pyogenic granuloma of the buccal mucosa in a 12 year old female child which was atypical in presentation and was treated by diode laser excision.
Keywords
Pyogenic granuloma; Lobular capillary haemangioma; Buccal mucosa; Diode laser
Introduction
Pyogenic granuloma is a common inflammatory hyperplasia of the oral cavity traditionally considered to be non neoplastic in nature [1]. It was first described by Poncet and Dor in 1897 as “human botryomycosis” [2,3]. Later, the name “pyogenic granuloma” was coined by Hartzell in 1904, however it is considered a misnomer as it neither produces pus nor does it represent a granulomatous inflammatory process [2]. Rather, it depicts an overzealous connective tissue response to a known stimulus or injury [4].
The term ‘pyogenic granuloma’ brings to mind a classical picture of the lesion. This includes a well circumscribed, profoundly erythematous, generally pedunculated, polypoid growth with a definite predilection for the maxillary anterior gingival [4,5]. In fact nearly 75% of all intraoral lesions are found on the gingiva and extra-gingival sites for pyogenic granuloma are fairly uncommon. Some lesions have been reported on the tongue, buccal mucosa and lips, but their clinical presentation tends to be atypical with lesions mimicking other benign soft tissue growths or even malignancy [5]. Pyogenic granulomas, primarily, are considered to arise due to either chronic irritation or hormonal influences. Here we report one such atypical case of intra-oral pyogenic granuloma arising at an extra-gingival site that was managed with diode laser excision.
Case Report
History
A 12 year old female patient reported to us with the chief complaint of a growth in the right buccal mucosa since two months. The growth was initially small in size and had enlarged progressively to a size large enough to interfere with her normal occlusion. The patient admitted to habitual cheek biting and reported occasional bleeding from the lesion but no pain.
Clinical presentation
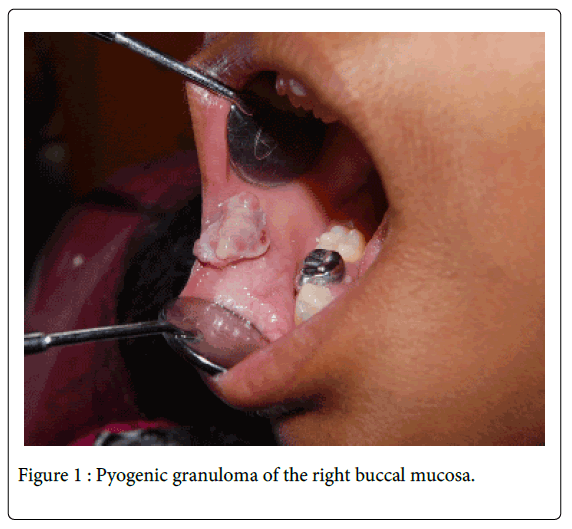
Clinical examination revealed an irregularly shaped, pedunculated growth in the right buccal mucosa near the angle of the mouth measuring around 2.5cm X 2cm (Figure 1). It had a lobulated surface and was predominantly greyish-white in colour with focal areas of erythema. On palpation, the lesion was found to be firm in consistency, non tender with no signs of hemorrhage/ discharge. There were no visible or palpable pulsations observed. Diascopy was also negative. The hard tissue examination revealed mixed dentition stage, stainless steel crowns in relation to pulpectomy treated 65, 85 and hard deposits on the teeth.
Based on the history and clinical presentation, we arrived at a provisional diagnosis of irritational fibroma of the right buccal mucosa.
Differential diagnosis
Due to the history of occasional bleeding, the differential diagnosis included vascular malformation and pyogenic granuloma and we decided to exercise caution while excising the lesion.
Investigations
Routine hematological investigations were performed and found to be in the normal range. An excisional biopsy was planned.
Treatment
Oral prophylaxis was performed for the patient. The lesion was excised under local anaesthesia using diode laser focalized at 975 nm (LaserHFTM, Hager & Werken, Duisburg, Germany) in non-contact mode (2mm of focal distance) with a 350µm fiber. As per our apprehensions, there was a significant amount of hemorrhage during the procedure and primary closure had to be performed to achieve hemostasis. Usual precautions for the patient, operator and the assistant were observed. Post-operative instructions were given to the patient. The excised tissue was sent for histopathological examination.
Histopathology
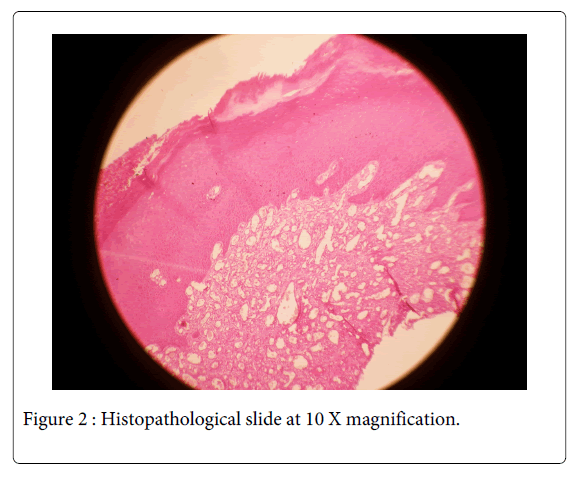
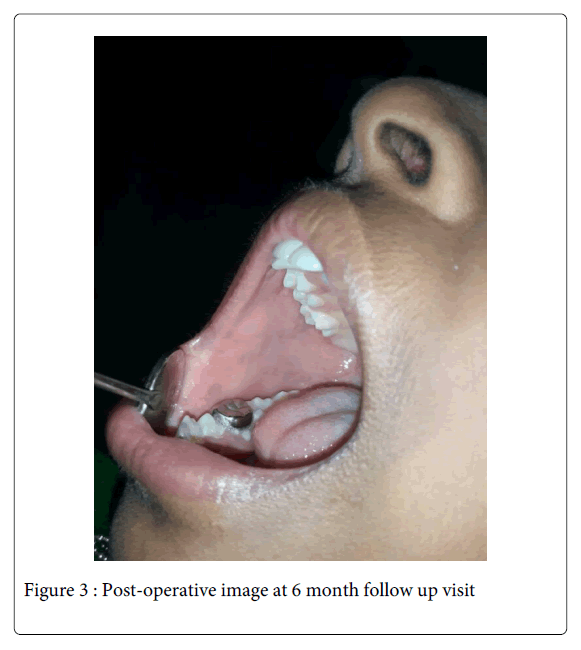
The histopathological analysis revealed a hyperplastic para-keratinized epithelium with a fibrous connective tissue stroma showing budding capillaries with plump endothelial cells, numerous blood vessels engorged with RBCs and hemorrhage at focal areas (Figure 2). All the features were suggestive of a diagnosis of ‘pyogenic granuloma’. The patient was recalled and after 3 weeks, the wound healing was completed uneventfully. The patient was counselled regarding her cheek biting habit and is on regular follow up to the present day (Figure 3).
Discussion
Pyogenic granulomas are benign soft tissue lesions of inflammatory origin that have a marked predilection for the gingiva. Among extra-gingival sites, tongue (4%) and lower lip (3%) are relatively more common [6]. When present on the skin, they are commonly found on the face, trunk and upper limb [7]. They are said to represent 26.8-32% of all reactive lesions [8,9]. A number of etiological factors have been considered for its development. These include, trauma or irritation from calculus or foreign materials, hormonal changes of pregnancy and certain types of drugs such as cyclosporine. Less frequently, patients undergoing guided tissue regeneration and bone marrow tranplantation procedures, have also been shown to develop pyogenic granulomas [10].
The pregnancy tumour variant of pyogenic granuloma occurs in up to 5% of pregnancies. The hormonal upheaval coincident with pregnancy increases the sensitivity of the host response to irritation; however bacterial plaque and gingival inflammation are required for the precipitation of these changes. Recent studies suggest that estrogen stimulates nerve growth factor (NGF), Granulocyte-Macrophage-Colony stimulating factor (GM-CSF) & Fibroblast growth factor (bFGß) and Transforming growth factor beta 1 (TGF-ß1) leading to formation of granulation tissue and subsequent wound healing. Estrogen is also known to enhance Vascular Endothelial Growth Factor (VEGF) production in macrophages. The fact that this effect is antagonized by androgens may explain the more frequent occurrence of pyogenic granulomas in females as compared to males (2:1 ratio) and its strong association with pregnancy. It has also been proposed that in the absence of VEGF post-pregnancy, Angiopoietin-2 (Ang- 2) causes blood vessels to regress with resultant egression of the lesion [8-10].
As for the traumatic etiology of pyogenic granuloma, according to Shafer et al., oral pyogenic granuloma arises as a result of infection by either staphylococci or streptococci. Some minor trauma to the tissues may provide a channel for non-specific microbial infection. The tissues respond to these organisms of low virulence by the exuberant proliferation of a vascular type of connective tissue [11].
The lesions typically occur in the second decade of life. Clinically these lesions usually present as single nodule or sessile papule with smooth or lobulated surface. These may be seen in any size from a few millimeters to less than 2.5cm, although lesions greater than 4 cm in diameter have also been reported [5]. In this case, as the patient had not attained puberty yet, a hormonal etiology of the lesion could well be ruled out. On the other hand, trauma due to the patient’s cheek biting habit could be implicated as a trigger for its development as the lesion was noted along the line of occlusion.
It has been observed that young pyogenic granulomas are more vascular in appearance because they demonstrate prominent capillaries and bleed spontaneously or upon the slightest provocation. Whereas older lesions tends to become more collagenized & pink [10]. This explains the atypical appearance and non-hemorrhagic clinical presentation of the current case.
In this case we opted for laser excision of the lesion with the perception that it would reduce intra-operative bleeding, operator time and post-operative pain as compared to scalpel excision. Since pyogenic granuloma is essentially a lesion exhibiting increased vascularity and is known to bleed profusely even on careful manipulation, haemorrhage was bound to occur in this case. However, the intra-operative haemorrhage that occurred was significantly controlled by laser excision as compared to that anticipated by scalpel excision. As White has pointed out, these factors generally improve patient compliance, which was particularly desirable in this case since the patient was very young [10].
Previously, Rai et al. [12] have successfully treated a patient with recurrent pyogenic granuloma of the gingiva using diode laser while Licata et al. [13] have achieved the similar results using Er, Cr: YSGG laser.
An important consideration is the difficulty distinguishing between pyogenic granuloma and haemangioma histopathologically. In fact another name for pyogenic granuloma is lobular capillary haemangioma. The only subtle difference is that in comparison to pyogenic granuloma, capillary haemangiomas have more plump, histiocytoid endothelial cell proliferation without presence of acute inflammation [10]. History plays a vital role in their differentiation. Haemangiomas are developmental in origin, usually beginning a few weeks after birth and growing rapidly thereafter. Pyogenic granulomas, on the other hand, tend to develop suddenly.
Conclusion
Intra-oral pyogenic granulomas developing at extra-gingival sites can prove to be a diagnostic challenge to the clinician. In the case under discussion, successful excision of the lesion was performed using diode laser and the post-operative outcome was found to be encouraging. This emphasizes the importance of thorough history and clinical examination in the formulation of a diagnosis and the importance of a sound knowledge of atypical lesion presentations that help to prevent erroneous diagnoses and disastrous consequences.
Acknowledgement
We would like to thank our Principal, Dr. B.V. Sreenivasa Murthy for his support and guidance.
References
- Neville BW, Damn DD, Alen Cm, Boquot JE (2002) Oral and maxillofacial pathology. (3rdedn), Elsevier, Philadelpia.
- Kamal R, Dahiya P, Puri A (2012) Oral pyogenic granuloma: Various concepts of etiopathogenesis. J Oral MaxillofacPathol 16: 79-82.
- Patil K, Mahima VG, Lahari K (2006) Extragingival pyogenic granuloma. Indian J Dent Res 17: 199-202.
- Regezi JA, Sciubba JJ, Jordan RC (2012) Oral pathology: clinical pathologic correlations. (6th edn), Elsevier Health Sciences.
- Gnepp DR (2009) Diagnostic Surgical Pathology of the Head and Neck. (2ndedn), Health Sciences.
- Saravana GH (2009) Oral pyogenic granuloma: a review of 137 cases. Br J Oral MaxillofacSurg 47: 318-319.
- Shenoy SS, Dinkar AD (2006) Pyogenic granuloma associated with bone loss in an eight year old child: A case report. J Indian SocPedodPrev Dent 24: 201-203.
- Amirchaghmaghi M, Falaki F, Mohtasham N, Mozafari PM (2008) Extragingival pyogenic granuloma: a case report. Cases J 1: 371.
- K A K, Ashok L, G P S (2013) Pyogenic granuloma on the upper labial mucosa: a case report.J ClinDiagn Res 7: 1244-1246.
- Jafarzadeh H, Sanatkhani M, Mohtasham N (2006) Oral pyogenic granuloma: a review.J Oral Sci 48: 167-175.
- Rajendran R (2009) Shafer's textbook of oral pathology. (6thedn), Elsevier.
- Rai S, Kaur M, Bhatnagar P (2011) Laser: a powerful tool for treatment of pyogenic granuloma.J CutanAesthetSurg 4: 144-147.
- Licata ME, Albanese A, Giannatempo G, Dioguardi M, Campisi G (2013) Minimally invasive approach to eliminate pyogenic granuloma using Er, Cr: YSGG laser. Ann Stomatol (Roma) 4: 25.
--
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 17323
- [From(publication date):
October-2014 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 12559
- PDF downloads : 4764