Review Article Open Access
Pulmonary and Thoracic Vascular Involvement in Behcet's Disease on CT
Damgaci L*Department of Radiology, Ankara Numune Education and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Lale Damgaci
Department of Radiology
Ankara Numune Education and Research Hospital, Ankara
Ankara 06100, Turkey
Tel: 0905357687688
E-mail: ldamgaci@hotmail.com
Received date: May 31, 2017; Accepted date: June 13, 2017; Published date: June 20, 2017
Citation: Damgaci L (2017) Pulmonary and Thoracic Vascular Involvement in Behçet’s Disease on CT. OMICS J Radiol 6:263. doi: 10.4172/2167-7964.1000263
Copyright: © 2017 Damgaci L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
Behçet’s disease (BD) is characterized by recurrent oral and genital ulcerations, ocular and additional clinical manifestations. The exact cause of the disease is unknown. Thoracic manifestations of BD show a wide spectrum including vascular, mediastinal, pleural and parenchymal involvement. CT is the imaging modality that provides the assessment of the thoracic presentations of BD. The typical presentations of BD are aneurysms of the pulmonary arteries and venous occlusion.
Aneurysms of the aorta, occlusion of vena cava superior, venous aneurysms, mediastinal lymphadenopathy, mediastinal fibrosis, pneumonia, pulmonary hemorrhage, infarction, pleural and pericardial effusions, and pleural nodules are other thoracic manifestations of BD. Assessment of these thoracic involvements can be used in the diagnosis of BD.
Keywords
Behçet’s disease; CT; Thorax
Introduction
Behçet’s disease (BD) is a multisystem inflammatory disease. Although genetic factors and microorganisms are considered as causes of the disease, the exact etiology is unknown. It is characterized by recurrent oral and genital ulcerations and uveitis. Behçet first described the clinical trial of the disease in 1937 [1]. BD may affect the joints, the skin, the gastrointestinal system, the central nervous system, the hearth and vascular system, and the lungs [2]. Vascular involvement is seen approximately in 25-30% of patients [3]. The main pathologic process is vasculitis and inflammation [4]. Pulmonary manifestations are relatively infrequent and have been reported in 1-10% of patients [2,5]. The disease is common in Mediterranean countries, Middle East and Asia. The prevalence rate in Turkey is 80-370 per 100.000 [2,3]. Although chest radiography is the first imaging modality, CT is the preferred method for diagnosing thoracic involvement of BD. We review the pulmonary, pleural and thoracic vascular manifestations of BD with CT findings.
Clinical Diagnosis
International Study Group described the diagnostic criteria of BD in 1990. The diagnosis is depend on detection of recurrent oral ulcerations, and two of the following criteria including:
Ô?¬ Recurrent genital ulcerations;
Ô?¬ Uveitis, retinal vasculitis;
Ô?¬ Skin lesions (erythema nodosum, folliculitis); and
Ô?¬ Positive skin pathergy test (pustule formation 24-48 h following skin prick) [6].
Imaging Techniques
Patients with pulmonary symptoms are assessed with chest x-ray. Chest radiographs can show hilar or mediastinal enlargements. Pulmonary artery and thoracic aortic aneurysms can cause hilar and mediastinal enlargements. Parenchymal changes in BD are nonspecific and usually seen as focal opacities [7-10].
CT is the preferred imaging method in the diagnosis and followup of BD. CT Angiography (CTA) maintains excellent analysis of the aorta, pulmonary arteries and veins. The spatial resolution of CT is better than Magnetic Resonance Imaging (MRI). Additionally, CT can show the parenchyma and the pleura more detailed than MRI [11].
Thoracic Vascular System Involvement
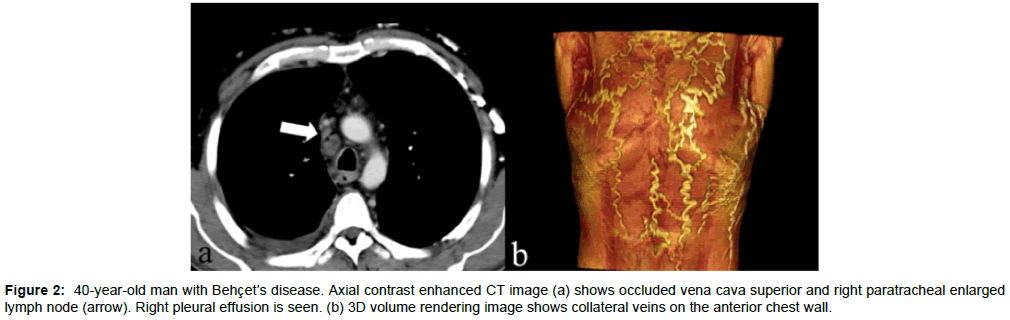
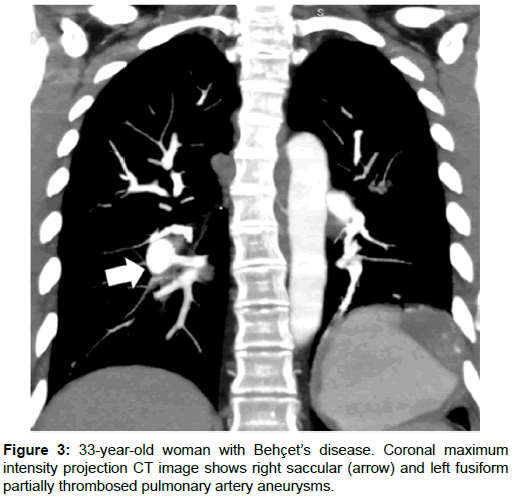
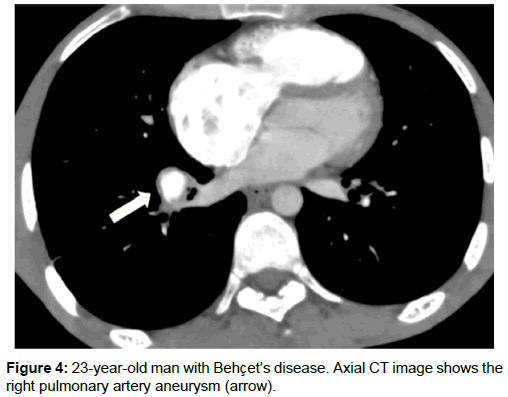
Pulmonary and thoracic aortic aneurysms, arterial and venous thrombosis are the main thoracic vascular manifestations of BD [12,13]. Vascular involvement occurs in 25-30% of patients and the complications can cause death [13-15]. Venous thrombosis is seen more than arterial involvement and presents 85% of vascular involvement. Superior vena cava occlusion is the most serious complication of venous involvement in BD [16]. Superior vena cava occlusion causes enlarged collateral veins in the mediastinum and chest wall (Figures 1 and 2). Thrombus can occur in the superior vena cava or propagate from a distal vein [17]. Venous aneurysms are rare in BD. Venous aneurysms in BD are due to presence of a predisposing factor such as trauma or other inflammatory disorders [18]. Arterial manifestations occur less frequently comparing with venous involvement and constitute 12% of vascular complications [12,19,20]. Aneurysm of the thoracic aorta, pulmonary artery and major branches occur in 65% of patients and occlusion in 35% [20,21]. BD is one of the most common causes of pulmonary artery aneurysms (Figures 3 and 4). Pulmonary artery aneurysms are caused by trauma, infections or Behcet’s disease (BD). Less common causes are pulmonary hypertension, congenital heart disease and neoplasm [22]. The inflammation of the vessel wall can cause dilatation and aneurysm formation.
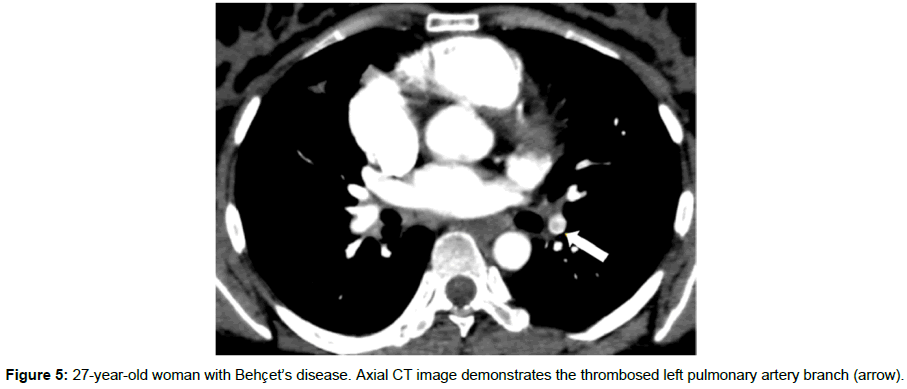
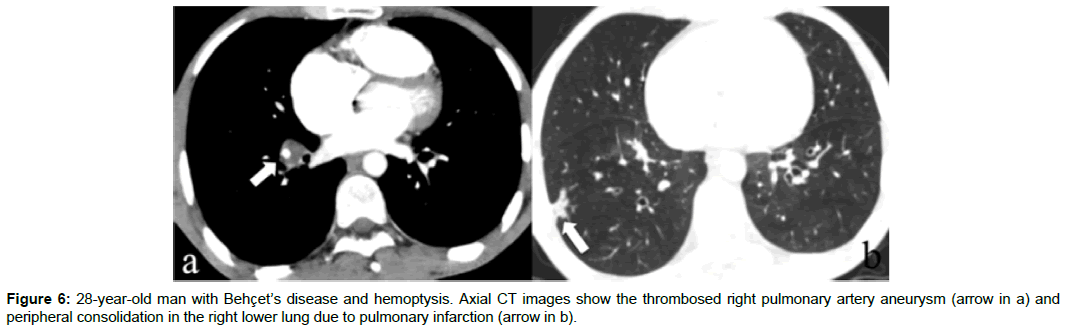
Inflammatory cellular infiltration also causes vessel wall thickening [23]. Steroid with combination of immunosuppressive agents can regress the pulmonary artery aneurysms. Early diagnosis of pulmonary artery aneurysm plays a critical role in the prognosis [24,25]. Occlusions and thrombosis of the pulmonary arteries are other complications of BD (Figure 5). The most common symptom, hemoptysis. Massive hemoptysis can cause death. Aneurysm rupture into a bronchus and pulmonary vessels thrombosis cause hemoptysis [12]. Pseudoaneurysms of the pulmonary artery, aortic arch, subclavian artery and coronary arteries have been reported in BD [26-28].
Mediastinum and Heart
Mediastinal lympadenopathy can be seen in BD (Figure 2a) [3]. Fibrosing mediastinitis is very rare in BD. Diffuse form of fibrosing mediastinitis may be presented as a mediastinal mass [3] One of the serious complications of BD is intracardiac thrombosis. It occurs mostly in the right atrium or ventricle. The prognosis of intracardiac thrombus is poor [29,30]. Pericardial effusion can occur because of the inflammation of the pericardium or thrombosis of the superior vena cava [3].
Pleura
Primary pleuritic disease is not common in BD [14]. Pleural effusion and pleural nodules can be seen in BD [2,13,14]. Pulmonary infarction, pneumonia, thrombosis of superior vena cava or vasculitis can cause pleural effusion (Figure 2a).
Lung
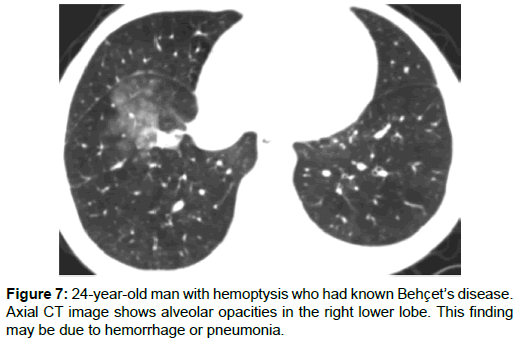
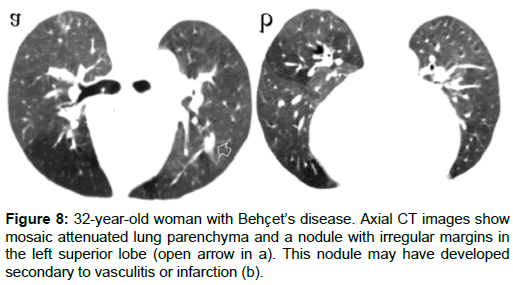
Lung parenchyma and pleural involvement occur in 1-10% of BD [31,32]. Pulmonary infarctions, pneumonia, pulmonary hemorrhage, atelectasis, bronchitis, fibrosis and emphysema are the involvement types of lung in BD. Thrombosis of pulmonary arteries may cause infarction, atelectasis, and hemorrhage (Figure 6) [12,13,18]. Focal or diffuse alveolar opacities, wedge-shaped consolidations, linear opacities, atelectasis, cavitary nodules, round opacities, reticulation and mosaic attenuation can be seen in the lung parenchyma (Figure 7). Alveolar opacities occur because of the vasculitis and hemorrhage [4,14,25]. In some patients with BD mosaic attenuation may be seen on CT scans due to small airway diseases or pulmonary artery thrombosis (Figure 8a and 8b) [14]. Pulmonary hemorrhage or pneumonia causes airspace consolidation or ground-glass opasification. Pneumonia may be seen secondary to immunosuppressive therapy [33]. Pulmonary infarctions can cause atelectasis, wedge shaped subpleural consolidations, linear parenchimal opacities or pleural effusions. Small-vessel vasculitis can cause reticulation [12,29].
Conclusion
Vascular involvement in BD can cause serious complications. Patients with pulmonary artery aneurysms have poor prognosis. Aortic and superior vena cava involvement may occur. Lungs, pleura, mediastinum may be involved. CT can show different thoracic manifestations of BD.
Conflict of Interest
The authors declare no conflict of interest. None of the authors has disclosed financial interests related to the material in the manuscript.
References
- Behçet H (1937) About recurring aphtous, virus-induced ulcers on mouth, eye and genitals (in German). Dermatol Monatsschr 105: 1152-1157.
- O’Duffy JD, Carney JA, Deodhar S (1971) Behçet’s disease. Report of ten cases, three with new manifestations. Ann Intern Med 75: 561-570.
- Hiller N, Lieberman S, Chajek-Shaul T, Bar-Ziv J, Shaham D (2004) Thoracic manifestations of Behc╠žet disease at CT. Radiographics 24: 801-808.
- Hamuryudan V, Yurdakul S, Moral F, Numan F, Tuzun H, et al. (1994) Pulmonary artery aneurysms in Behçet’s syndrome: reporta of 24 cases. Br J Rheumatol 33: 48-51.
- Lakhanpal S, Tani K, Lie JT, Katoh K, Ishigatsubo Y, et al. (1985) Pathologic features of Behçet's syndrome: a review of Japanese autopsy registry data. Hum Pathol 16: 790-795.
- International Study Group for Behçet’s disease (1990) Criteria for diagnosis of Behçet’s disease. Lancet 335: 1078-1080.
- Chajek T, Fainaru M (1975) Behçet's disease. Report of 41 cases and a review of the literature. Medicine 54: 179-196.
- Yamamato S (1974) A nation-wide survey of Behçet’s disease in Japan: I. Epidemiological survey. Jpn J Opthalmol 18: 282-290.
- Hirohata T, Kuratsune M, Nomura A, Jimi S (1975) Prevalence of Behçet's syndrome in Hawaii. With particular reference to the comparison of the Japanese in Hawaii and Japan. Hawaii Med J 34: 244-246.
- Erkan F (1999) Pulmonary involvement in Behçet’s disease. Curr Opin Pulm Med 5: 314-318.
- Cho YK, Lee W, Choi SI, Jae HJ, Chung JW, et al. (2008) Cardiovascular Behçet disease. The variable findings of rare complications with CT angiography and conventional angiography and its interventional management. J Comput Assist Tomogr 32: 679-689.
- Erkan F, Gul A, Tasali E (2001) Pulmonary manifestations of Behçet’s disease. Thorax 56: 572-578.
- Tunac─▒ A, Berkmen YM, Gokmen E (1995) Thoracic involement in Behçet’s disease: pathologic, clinical and imaging features. AJR 164: 51-56.
- Matsumoto T, Uekusa T, Fukuda Y (1991) Vasculo-Behçet's disease: a pathologic study of eight cases. Hum Pathol 22: 45-51.
- Kabbaj N, Benjelloun G, Gueddari FZ, Dafiri R, Imani F (1993) Vascular involvements in Behçet’s disease: based on 40 patients records. J Radiol 74: 649-656.
- Ahn JM, Im JG, Ryoo JW, Kim SJ, Do YS, et al. (1995) Thoracic manifestations of Behçet syndrome: radiographic and CT findings in nine patients. Radiology 194: 199-203.
- Sakane T, Takeno M, Suzuki N, Inaba G (1999) Behçet’s disease. N Eng J Med 341: 1284-1291.
- Burkill GJ, Burn PR, Padley SP (1997) Aneurysm of the left brachiocephalic vein: an unusual cause of mediastinal widening. Br J Radiol 70: 837-839.
- Guney B, Demirpolat G, Sava┼? R, Alper H (2004) An unusual cause of mediastinal widening: bilateral innominate vein aneurysms. Acta Radiol 45: 266-268.
- Park JH, Chung JW, Joh JH, Song SY, Shin SJ, et al. (2001) Aortic and arterial aneurysms in Behçet disease: management with stent grafts-initial experience. Radiology 220: 745-750.
- Koc Y, Gullu I, Akpek G, Akpolat T, Kansu E, et al. (1992) Vascular involvement in Behçet’s disease. J Rheumatol 19: 402-410.
- Grenier PH, Bletry O, Cornud F, Godeau P, Nahum H (1981) Pulmonary involvement in Behçet’s disease. AJR 137: 565-569.
- Raz I, Okon E, Chajek-Shaul T (1989) Pulmonary manifestations in Behçet’s syndrome. Chest 95: 585-589.
- Celenk C, Celenk P, Akan H, Ba┼?o─?lu A (1999) Pulmonary artery aneurysms due to Behçet’s disease: MR imaging and digital substraction angiography findings. AJR 172: 844-845.
- Emad Y, Ragab Y, Shawki Ael-H, Gheita T, El-Marakbi A, et al. (2007) Houges-Stovin syndrome: is it incomplete Behçet’s? Report of two cases and review of the literature. Clin Rheumatol 26: 1993-1996.
- Okita Y, Ando M, Minatoya K, Kitamura S, Matsuo H (1998) Multipl pseudoaneurysms of the aortic arch, right subclavian artery and abdominal aorta with Behçet’s disease. J Vasc Surg 28: 723-726.
- Nonaka K, Makuuchi H, Naruse J, Kobayashi T, Goto M, et al. (1998) Pseudoaneurysms of aortic arch and rupture into pericardium, a case report of succesful surgical management. Jpn J Thorac Cardiovasc Surg 46: 772-776.
- Modaghegh MH, Kazemzadeh GH, Jokar MH (2010) A case of Behçet disease with pulmonary artery pseudoaneurysm: long term follow-up. East Mediterr Health J 16: 346-349.
- Mogulkoc N, Burgess MI, Bishop PW (2000) Intracardiac thrombus in Behçet’s disease.: a systematic review. Chest 118: 479-487.
- Houman MH, Ksontini I, Ghorbel IB, Lamloum M, Braham A, et al. (2002) Association of right heart thrombosis, endomyocardial fibrosis, and pulmonary artery aneurysm in Behçet’s disease. Eur J Int Med 13: 455-457.
- Fairley C, Wilson JW, Barraclough D (1989) Pulmonary involvement in Behçet’s sydrome. Chest 96: 1428-1429.
- Cadman EC, Lundberg WB, Mitchell MS (1976) Pulmonary manifestations in Behçet’s syndrome. Arch Intern Med 136: 944-947.
- Ceylan N, Bayraktaroglu S, Erturk SM, Savas R, Alper H (2010) Pulmonary and vascular manifestations of Behçet disease: imaging findings. AJR 194: 158-164.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 4507
- [From(publication date):
June-2017 - Jul 14, 2025] - Breakdown by view type
- HTML page views : 3666
- PDF downloads : 841