Commentary Open Access
Psychosocial Safety Climate: Role and Significance in Aged Care
Peter C Winwood1*, Bowden R2 and Fiona Stevens31School of Psychology, Social Work and Social Policy, University of South Australia, Australia
2WORKXtra Physiotherapy, Adelaide, South Australia, Australia
3Central Psychology Services, Adelaide, South Australia, Australia
- *Corresponding Author:
- Peter C Winwood
School of Psychology
Social Work and Social Policy
University of South Australia, Australia
Tel: 61883379904
E-mail: pwinwood@internode.on.net
Received date: August 13, 2013; Accepted date: October 21, 2013; Published date: October 29, 2013
Citation: Winwood PC, Bowden R, Stevens F (2013) Psychosocial Safety Climate: Role and Significance in Aged Care. Occup Med Health Aff 1:135. doi: 10.4172/2329-6879.1000135
Copyright: © 2013 Winwood PC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Occupational Medicine & Health Affairs
Abstract
Psychosocial Safety Climate (PSC) is increasingly being recognised as a ‘cause of causes’ and a significant mediator/moderator of a number of important workplace behaviours and attitudes including; morale, cynicism,engagement, commitment and absenteeism. In this paper we examine the role of PSC within the Aged Care industry in Australia. Currently this industry is notable for having the very high levels of workplace injury and compensation claims, particularly among unregistered carers. Our results indicate that there is a clear economic argument for owners and managers of aged care facilities to address issues of suboptimal PSC within their facilities as a priority. Failure to do so can result in a progressive download spiral of poor performance, low commitment, staff turnover (and rehiring costs) associated with high injury and compensation costs.
Keywords
Aged care; Intervention; Psychosocial safety climate; Organisational psychology; Management
Introduction
Anyone who has worked in an organisation for more than a few weeks understands that it only takes a short time before one acquires a fairly clear understanding of the ‘mood’ and ‘tone’ of that workplace. This occurs largely unconsciously, but may also be strongly informed by the behaviour, manner, and opinions of co-workers. To this extent, it represents an example of ‘emotional contagion’ [1].
Taken together, these direct and indirect observations and experiences sum to an abiding sense of the extent to which one feels ‘safe’ in the workplace. This is more than physical safety (which is usually well covered in relevant and mandatory Occupational Health and Safety (Work Safety) legislation). It encompasses the feeling and belief that one’s work is valued by the organisation. This value is demonstrated unmistakably by the philosophies, processes, behaviours and practices within the organisation, which impact on you and/or others around you, and which are clearly designed to prevent you (to the greatest extent that is practically possible) being injured or harmed, physically or emotionally, in that workplace.
This condition has been defined as ‘psychosocial safety climate’ or PSC [2,3]. Ongoing research into the phenomenon has demonstrated that it constitutes a very basic psychological underpinning to the work experience of every worker who is exposed to the ‘climate’.
Whether high or low, PSC functions as a ‘cause of causes’ within the organisation. It both mediates and moderates a number of important experiential phenomena and responses. These include; the extent, level and toleration of bullying, overall organisational morale, and the frequency of workplace injury and injury claim [4]. These are associated, in turn, with absenteeism, commitment (affective and perseverant) and work engagement.
The notable feature of PSC is that it is a ‘top down’ phenomenon. PSC is set and controlled by the organisation’s management from the highest levels downward. PSC is not ‘chosen’ by an organisation, indeed it is rarely considered as a deliberate policy. Nevertheless, every organisation and every workforce operates within a PSC, whether it is recognised and acknowledged or not. PSC cannot be faked or contrived, except insofar as cynical and insincere attempts to fake it will be seen, experienced, and inevitably contribute to a reduction or lowering of PSC.
In this paper the authors report on their experience and observations of PSC, and its ramifications, in the Aged Care industry in South Australia.
This growing industry faces significant difficulties. During the past decade, media reports ofnotorious cases of suboptimal conditions and treatment of residents have resulted in a significant body of regulations being imposed on owners of aged care facilities. However, the current funding model for these facilities is such that adequate staff/resident ratios are difficult to maintain. In addition, the wage rates for both registered and unregistered workers in this sector are notably lower than in acute care.
Taken together with the inherent demands of the work, these pressures result a chronic shortage of workers in the area. Consequently there has been an increasing tendency to recruit from overseas sources as well as among newly arrived migrants and refugees. Although addressing worker shortages, this move adds potential language and cultural difference difficulties to an already challenging mix.
It is self- evident that the economic imperative within such an organisational framework particularly includes; Low staff turnover (with associated retraining costs), Low absenteeism (with associated expensive agency staff usage), low sickness and injury frequency (low agency staff requirements) and low return to work times (RTW) when unavoidable staff injury absences do occur.
Between June 2010 and October 2012, the authors investigated some 10 aged care facilities. At each facility, staff were asked to complete a comprehensive questionnaire developed by the first author, the Occupational Psychosocial Risk Index (OPRI). This instrument comprises 105 items. In addition to demographic information, these items comprise a total of 19 subscales. Of these, 12 of the subscales were validated psychometric measures. These included:
• The Cognitive, Emotional, and Physical Demands subscales of the DISC scale [7].
The Chronic and Acute Fatigue and Recovery subscales of the OFER measure [8].
The Utrecht Work Engagement Scale [9].
The Sleep subscale of the Psychological Injury Risk Indicator [10].
The Cynicism subscale of the Maslach Burnout Inventory General Scale [11].
The Affective and Perseverant Commitment subscales of the Meyer and Allen Organisational Commitment scale [12].
In addition, the OPRI questionnaire comprised custom designed measures. The items for these scales (particularly where they departed from better known, validated, measures such as for Bullying) were created after discussions with people working in aged care. These custom scales included:
• Facility Resources, i.e. “If we need new, or more equipment, it is always obtained promptly” and “Problems with equipment or facilities are always attended to promptly here”, etc.
• Bullying. This custom scale of 5 items included “I have never seen anyone bullied here”, “I have never been bullied in any way while working here”, and “If ever I experienced any bullying here I could rely on management to resolve the issue for me quickly and effectively”.
• A broad guide to an understanding of bullying in the workplace was included in a footnote.
• Note: Workplace bullying is any behaviour that is repeated, systematic and directed towards an employee (or group of employees) that a reasonable person (considering the circumstances) would expect to victimise, humiliate, undermine or threaten, and which creates a potential risk to health and safety.
• Morale: 5 items included items such as: “There is always a good atmosphere between all staff working here” and “There is a lot of negative feeling between staff members here”.
• Absenteeism: 4 items included items such as: “I sometimes call in sick when I’m not actually sick”, “It doesn’t really bother me to call in sick when I’m not really ill”
• Physical Self Care at Work: 3 items included: “I ALWAYS use lifters when resident’s care plan says I must”, “I am careful not to get any injury to my back or joints at work”
• Persistent Work Related Pain at Home: 5 items included: “I often have a lot of muscle and/ or joint pain after I finish my work shift”, “I sometimes have to take time off work because of muscle and /or joint pain caused by my work”.
• Significant Physical Pains at Work: 7 items including; “I get a lot of muscle/joint pain from my work”, “.I usually don’t have any problems with muscle aches or joint pain”, and “Muscle aches and pains often affect how well I can work”.
The number of items and the Likert response scale for these subscales varied. However all had a 0 lowest score.
Accordingly all the scores, on all the subscales, were standardised to a 0-100 scale by applying the formula:
From an organisational psychology perspective, all of these experienced constructs could be expected to be mediated and/or moderated by worker commitment, both affective and perseverant; i.e. “…I work here because I like it” as opposed to “I only work here until I can get a better job”. Such commitment might be expected to be strongly associated with worker morale, and in turn, such morale moderated by PSC.
The number of respondents (staff completing measurement questionnaire) at each facility) varied between 65 and 115. In each case (facility) the N was sufficient to provide a Power of at least .8 for the analyses that were undertaken (i.e. bivariate correlation, one-way ANOVA (5 groups).
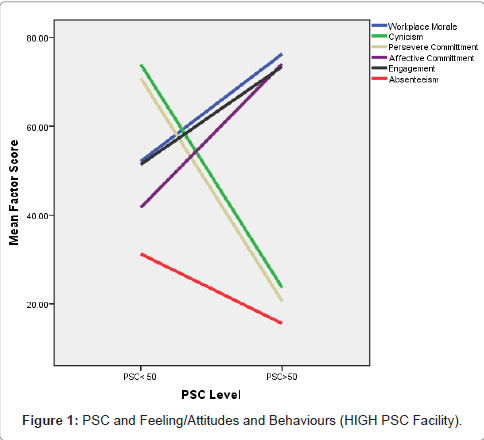
Figure 1 indicates relationships between PSC, Morale, Cynicism, Affective and Perseverant Commitment, and Work Engagement. This graph is derived from data recorded at a facility with 102 respondents with an overall high PSC score (PSC score 62.8) and represents an ‘extreme case (high)’ exemplar (Figure 1).
At this facility the overall mean score for perceived PSC was measured at 62.8 on a standardised 0-100 scale.
The variation of the other constructs according to a split half (above and below 50) of respondentPSC scores is very evident. Notable positive and negative correlations between PSC and the other factors are clear. These are reported exactly in Table 1.
| PSC | Workplace Morale | Cynicism | Persevere Commitment | Affective Commitment | Work Engagement | |
| PSC | 1.00 | |||||
| WorkplaceMorale | .42** | 1.00 | ||||
| Cynicism | -.40** | -.50** | 1.00 | |||
| Persevere Commitment | -.17 | -.44** | .32* | 1.00 | ||
| Affective Commitment | .25 | .71** | -.44** | -.48** | 1.00 | |
| Work Engagement | .29 | .67** | -.49** | -.41** | .53** | 1.00 |
| Notes: **. Correlation is significant at the 0.01 level (2-tailed).*. Correlation is significant at the 0.05 level (2-tailed).PSC =Psychosocial Safety Climate. Notable correlations are bolded. | ||||||
Table 1: Pearson Bivariate Correlations of PSC, Morale, Cynicism, Commitment and Engagement at Work.
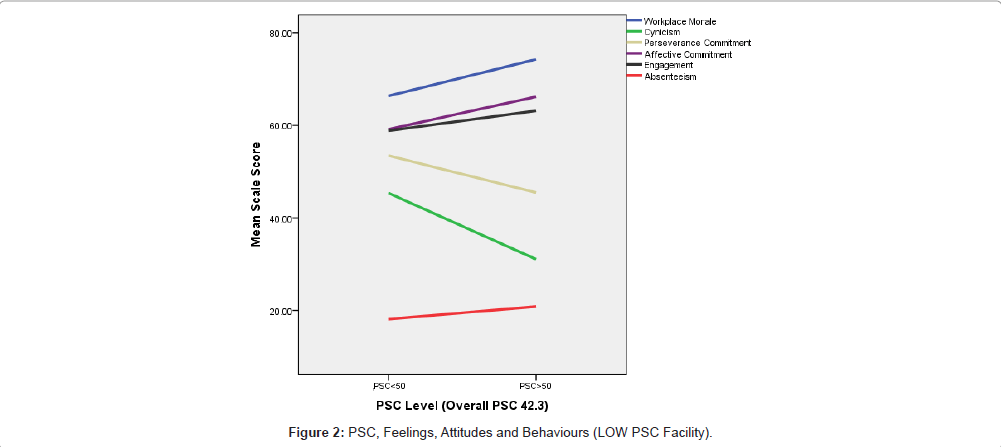
By contrast, Figure 2 reports the relationship of PSC with other factors in a low PSC facility with some 82 respondents where the mean perceived PSC was recorded at 42.3 on the PSC 12 scale. This represents an ‘extreme cases (low)’ exemplar (Figure 2).
Although the same positive and negative correlations between PSC and the other factors (Figure 1) are evident, the actual differences in mean respondent score between the split half of respondent PSC scores is much lower. In other words, in this low PSC (overall) environment, the workplace feelings, attitudes, and behaviours are more uniformly poor, or less desirable.
Practical observations on issues affecting PSC level
At facilities where PSC was to prove to be high (>50 on the PSC 12 scale) it was notable that the facility owner/manager tended to speak in positive terms about the staff. The phrase “…my staff are my biggest asset”, or words to this effect, were commonly expressed. By comparison, at facilities where PSC was to prove low (<50 on the PSC 12 scale), managers/owners expressed a quite different attitude towards staff. The focus was very much on the residents and their relatives and keeping them happy. The staffs was taken for granted-they were just ‘there’ to serve this requirement. As PSC decreased, this attitude also seemed to deteriorate. Often there was an outright distrust of staff (particularly carers) who were ‘expected’ to be; “...out for what they can get….”, and “… make false claims for injury”… and “…have no intention to come back to work after making a claim…”.
It seemed that some owners/managers had a bad experience(s) in the past with particular employees. This (isolated) experience became an entrenched bias. Consequently attitudes towards staff were based upon an expectation of the worst of their employer experiences. Tragically, this tended to produce a ‘self-fulfilling prophesy’. Within such facilities, work-related claims and costs, absenteeism and bullying behaviours tended to be very high, and along with this went high staff turnover. All of which was explained away by (and blamed on) the attitudes of the staff (particularly new migrants), reinforcing the bias that had developed.
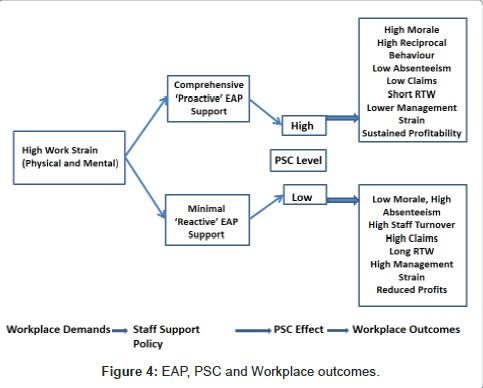
In parallel research, the first author interviewed some 16 for profit aged care facility owners and/or managers to enquire about what Employee Assistance Programs (EAP) they offered for their staff. Such programs might include for example; low cost (or no cost) physiotherapy to treat work related musculo/skeletal strains, low cost (or no cost) psychology referral for emotional problems affecting work, (limited) financial support to assist family emergency, time off to attend family problems, etc.
Once again there were considerable differences of view and attitude towards EAP expressed by owner/managers. Whereas some employers were keen to support their staff in any way possible because; “…they are our best asset”, others viewed such additional supports as; “…nice in theory, but quite unaffordable”.
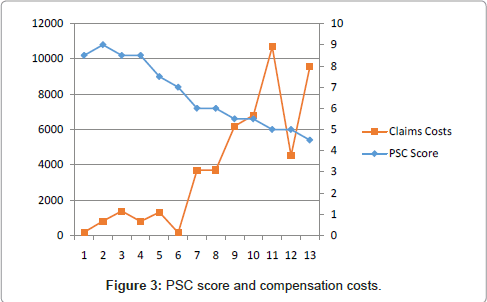
However, such views would appear to be short-sighted and economically questionable. Figure 3 represents the relationship between injury compensation claims costs (in $AUD 1000’s), at 13 of the 16 facilities for which data could be derived. Injury cost data was supplied by the State based workers compensation agent-WorkCover SA; PSC level was assessed on a 0-10 scale as a function of EAP support provided by the facility owner according to his description. The more support in the way of EAP was provided (Figure 3).
(With consequential PSC level increase), the lower the work compensation (for injury) costs were evident (Figure 3).
Notes: PSC score is indicated on a 0-10 scale (Right Y Axis), Claims costs are in $AUD 1000’s (Left Y Axis). Number of Facilities is shown on the X axis.
Taken together, the author’s observations indicate that there is a significant economic argument for deliberate and careful attention to PSC within aged care. This argument rests on a number of undoubted factors.
1. High PSC facilities tend to have lower staff turnover. This results in lower costs for retraining.
2. Consistent work teams tend to work more efficiently and effectively; they know each other’s capacities and ‘oddities’ and adjust accordingly.
3. Consistent staffing enables workers to know residents and their particular needs without being told and provide overall more effective care. They also know and develop useful relationships with relatives, all of which militates for more effective and harmonious relationships and enhancement of the facility reputation.
4. Happy staff tend to actually look after themselves (use of lifters, manual handling) more consistently.
5. Injuries at work tend to be fewer.
6. Return to Work (RTW) times tend to be lower (unhappy injured staff do not hurry to return to where they are unhappy).
7. Lower injury rates and overall claims costs allow facilities to negotiate lower WorkCover insurance rates.
In sum, the cost of providing those supports and conditions which make for high PSC levels is significantly outweighed by the savings and reductions indicated above.
This is represented in the model shown overleaf in Figure 4.
Conclusion
The progressive aging of Australia’s population creates significant challenges to be able to meet the needs of this expanding proportion of citizens who can no longer care for themselves, or be cared for by their families. Government derived money to fund the increasing number of aged care facilities in clearly not unlimited. There will always be economic pressure on facility owners and managers in the aged care industry.
However, our research indicates that a solution to such problems for the ‘bottom line’ are not solved by minimising spending on staff care in favour of resident care. Quite the reverse appears to be the case. Caring for staff with as much zeal as caring for the residents i.e. building and maintaining the highest levels of PSC we contend is the optimum course to ensure that profitability is maintained.
Happy, healthy, long tenured and confident staff will deliver better care, with greater efficiency, and minimal losses due to absenteeism, high injury incidence and high RTW times which clearly accompany the alternative found in low PSC organisations.
Acknowledgements
The authors acknowledge the support of Employers Mutual Insurance and the Aged Care Association of Australia in the development of their work in the Aged Care sector in South Australia.
References
- Melwani S, Barsade SG (2011) Held in contempt: the psychological, interpersonal, and performance consequences of contempt in a work context. J Pers Soc Psychol 101: 503-520.
- Dollard MF, AB Bakker (2010) "Psychosocial safety climate as a precursor to conducive work environments, psychological health problems, and employee engagement." Journal of Occupational and Organizational Psychology 83: 579-599.
- Dollard MF, McTernan W (2011) Psychosocial safety climate: a multilevel theory of work stress in the health and community service sector. Epidemiol Psychiatr Sci 20: 287-293.
- Law R, Dollard MF, Tuckey MR, Dormann C (2011) Psychosocial safety climate as a lead indicator of workplace bullying and harassment, job resources, psychological health and employee engagement. Accid Anal Prev 43: 1782-1793.
- Hall, Garry B, Dollard, Maureen F, Coward, et al. (2010) "Psychosocial Safety Climate: Development of the PSC-12." International Journal of Stress Management 17: 353-383.
- Hall GB, Dollard MF, Winefield AH, Dormann C, Bakker AB (2013) Psychosocial safety climate buffers effects of job demands on depression and positive organizational behaviors. Anxiety Stress Coping 26: 355-377.
- de Jonge J, Dormann C (2003) The DISC model: Demand-Induced Strain Compensation Mechanisms in Job Stress. Occupational Stress in the Service Professions. A H W Maureen F Dollard, Helen R Winefield. London, Taylor & Francis: 43-67
- Winwood PC, Lushington K, Winefield AH (2006) Further development and validation of the Occupational Fatigue Exhaustion Recovery (OFER) scale. J Occup Environ Med 48: 381-389.
- Schaufeli WB, Sarah Jane Cotton, Edgar Bresó, Jan de Jonge, Maureen Dollard, et al. (2006) "The measurement of work engagement with a short questionnaire - A cross-national study." Educational and Psychological Measurement 66: 701-716.
- Winwood PC, Peters R, Peters M, Dollard M (2012) Further validation of the psychological injury risk indicator scale. J Occup Environ Med 54: 478-484.
- Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52: 397-422.
- Meyer JP, Allen NJ (2007) "A three-component conceptualization of organizational commitment: Some methodological considerations." Human Resource Management Review 1: 61-98.
Relevant Topics
- Child Health Education
- Construction Safety
- Dental Health Education
- Holistic Health Education
- Industrial Hygiene
- Nursing Health Education
- Occupational and Environmental Medicine
- Occupational Dermatitis
- Occupational Disorders
- Occupational Exposures
- Occupational Medicine
- Occupational Physical Therapy
- Occupational Rehabilitation
- Occupational Standards
- Occupational Therapist Practice
- Occupational Therapy
- Occupational Therapy Devices & Market Analysis
- Occupational Toxicology
- Oral Health Education
- Paediatric Occupational Therapy
- Perinatal Mental Health
- Pleural Mesothelioma
- Recreation Therapy
- Sensory Integration Therapy
- Workplace Safety & Stress
- Workplace Safety Culture
Recommended Journals
Article Tools
Article Usage
- Total views: 15850
- [From(publication date):
October-2013 - Apr 20, 2025] - Breakdown by view type
- HTML page views : 11180
- PDF downloads : 4670