Psychosocial Impacts of Stigmatization and Discrimination among Persons with Mental Disorders at Federal Neuropsychiatric Hospital Calabar, Calabar Cross River State
Received: 08-Jun-2022 / Manuscript No. ijemhhr-22-66116 / Editor assigned: 08-Jun-2022 / PreQC No. ijemhhr-22-66116 / Reviewed: 22-Jun-2022 / QC No. ijemhhr-22-66116 / Revised: 23-Jun-2022 / Manuscript No. ijemhhr-22-66116 / Published Date: 30-Jun-2022
Abstract
The purpose of this study was to assess the psychosocial impacts of stigmatization and discrimination among persons with mental disorders at Federal Neuropsychiatric Hospital Calabar, Cross River State, Nigeria. A cross-sectional descriptive survey design was adopted. A simple random sampling technique was used to select the sample size of 121 participants for the study. The instrument of data collection was a structured questionnaire which consisted of 4 sections. Data was collected using face-to-face method and questionnaire retrieved at the spot. Data were analyzed using descriptive statistics, frequencies, tables and percentages. The findings of the study revealed that large proportion 90 (74.4%) respondents always keep their mental health problem hidden from others with (X)=1.74; 75(62.0%) don’t have any close personal relationship with (X)=1.62, 101(81%) respondents often isolate from others due to fear of unfair treatment (X)=1.83. 88 (72.7%) participants adopted avoiding negative information that anger-in associated then avoid angry emotions, 76(62.8%) participants cope by attending social support groups with (X)=1.63. There was a significant relationship between age and the psychological impacts of stigmatization and discrimination (X2 =37.53 and P= 0.01). Stigmatization and discrimination had significant impact on psychosocial wellbeing resulting in self-isolation a major cause of suicidal thoughts.
Keywords: Psychosocial Impacts, Stigmatization, Discrimination, Mental Disorders Neuropsychiatric
Introduction
Mental disorders are one of the most worrisome public health concerned in the world. Mental disorders are health challenges that places significant burden on individuals, families, communities and societies. Mental disorders vary in the frequency and severity of their occurrence, ranging from common disorders such as anxiety, hysteria and trauma-related disorders, to severe mental disorders such as schizophrenia, schizoaffective disorder, bipolar disorder, depressive disorder, and neurocognitive disorder (Talatala, et al. 2020). In sub-Saharan Africa, mental illness accounts for 19% of Years of healthy life lost due to disability regionally (British Council, 2018). In Nigeria, statistics on mental disorders are alarming. It was reported that a population of approximately over 184 million people, 64 million Nigerians have some form of mental disorders (Oyewunmi, et al. 2015). The prevalence of mental disorders in Nigeria is related to the many socio-economic problems that can be considered as triggers (Armiyau, 2015).
Persons with mental disorders often have to deal with social misconceptions about various mental disorders which lead to stigmatization (Oexle, et al. 2017). Most individuals with mental disorders still have huge problems finding job placement due to employer’s discrimination. Mental disorders causes not only the difficulties arising from the symptoms of the disorders, but also the discomforts associated with societal reactions, as an added complication, persons with mental disorders may accept common misconceptions about mental disorders; turn against themselves and lose confidence. Stigmatization and discrimination deprive victims of mental disorders of their full measure of human dignity and participation in society as a whole by undermining social support and compromising treatment options; this is as a result of individual and institutional discrimination due to misconceptions, harmful stereotypes, and negative public and professional attitudes toward mental disorders (Picco, et al. 2016). The lack of effective community-based mental health services forcing patients to be cared for in psychiatric institutions and other places with limited facilities where they are subjected to traditional treatment that is considered inhumane (Morgades, et al. 2019).
The Modified Labeling Theory was adopted to guide the study, it was developed by Links et al in 1989 to Step away from the causal role of stigma. The theory assumes that during socialization, an individual forms beliefs about how mental illness is treated. For example, an individual may believe that persons with mental illness are discriminated against or treated as outcasts. These beliefs become particularly relevant if and when the individual is diagnosed or treated for symptoms related to mental illness because those beliefs are applied to oneself, thus, discrimination and negative reactions are anticipated. When this happens, the theory posit that individuals employ stigma management strategies to cope with the anticipated stigma. The theory propose three such strategies: education, withdrawal, and secrecy.
While adopting one or more of these strategies can assist an individual in coping with a negative label, they can also result in unconstructive social outcomes. Relying on secrecy as a stigma management strategy may encourage feelings of dissimilarity or shame. Withdrawal can result in social network constriction, which limits opportunities that could aid in successful social integration.
There is widespread stigma and discrimination among the mentally ill in Nigeria, even among the population who should be informed (Chan, et al. 2019). The widespread belief in the supernatural cause of mental disorders according to a researcher (Hipes, et al. 2016) is likely to contribute to the difficulties in designing an effective anti-stigma psychoeducation program in Nigeria. Moreover, the impact of stigmatizing attitudes and ignorance of mental disorders among Nigerians has shown to be a major challenge to improving mental health care services in Nigeria. Therefore, this study aims to assess the psychosocial effects of stigma and discrimination in patients with psychiatric disorders at the Federal Neuropsychiatric Hospital Calabar.
Material and Methods
Research Design and Setting: The research design adopted for this study is the cross-sectional descriptive design. The research setting is Federal Neuropsychiatry Hospital, Calabar, and Cross River State. The hospital is located in Calabar South Local Government Area.
Participant and Sample Size: The study population comprises of all adult patients receiving treatment for mental disorder at the Federal Neuropsychiatry Hospital, Calabar totaling one hundred and fifty (150). The sampling technique used in this study is the simple random sampling technique. A sample of one hundred and twentyone (121) patients was drawn from the target population of one hundred and fifty (150). The sample size was calculated using Slovin’s formula stated as follows:
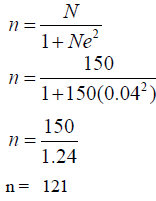
Therefore, the total sample size was 121
Inclusion Criteria
- Participant who have used the facility for the past one year.
- Participant must be 18 years and above.
- Participant must be mentally stable.
- Participant present at the time of the study.
- Participant must be willing to participate in the study.
Exclusion Criteria
- Patient experiencing severe mental disorder, and not mentally stable to respond to interview questionnaire
Study Tool: A well-structured questionnaire developed by the researchers based on the literature review was used for data collection. It consisted of Section A which elicited information on the socio-demographic characteristics of the respondents. Section B elicited information on the psychological impact of stigmatization and discrimination. Sections C used to obtain information on the social impact of stigmatization and discrimination. Sections D used to elicit information on the coping strategies adopted by patients.
Data Collection Procedure: Data was collected through face-to-face administration of questionnaires during a two-week visit to the hospital. and was retrieved on the spot through the help of a research assistant. After the respondent has completed the forms, the researcher gathers data for analysis.
Statistical Analysis: Data were analyzed using inferential and descriptive statistic using tables, frequencies and percentages. Hypothesis was tested using Chi-square at 0.05 level of significance.
Ethical Consideration: Ethical clearance was obtained from the research and ethical committee of the Federal Neuropsychiatry Hospital, Calabar. The researcher also got informed consent from the respondents. The respondents were given adequate information about the research work, which satisfied their right to full disclosure of information. Their rights to autonomy and voluntary participation were strictly adhered to. All procedures involving human subjects/patients were approved by Research and Ethical Committee Federal Neuropsychiatric Hospital of the relevant local, regional or national review body and approval number FNPH/PIS/40/S.II/VOL.X/312 was obtained on July, 26th 2021.
Results
Results in Table I showed that, 15(12.4%) were below 25 years old, 31 (25.6%) respondents were between 26- 34 years; 22 (18.2%) respondents were 35-44 years 25 (20.7%) respondents were within the ages of 45 and 54 years, while 28 (23.1%) respondents were aged 55 years and above. majority, 79 (65.3%) were male while 42 (34.7%) respondents were female. Most 58 (47.9%) respondents were single, 34 (28.1%) respondents were married; divorcees were 21 (17.4%), while 8 (6.6%) respondents were widows(er). Also, large number 67 (53.4%) had secondary education; 36 (29.8%), had tertiary education while 18 (14.9%) respondents attended primary education. In addition, 30 (24.8%) respondents were public/civil servants. 29 (24.0%) respondents were unemployed, 29 (24.0%) respondents were into business and trading, while 37 (30.6%) respondents were students. Lastly, majority of the respondents, 115 (95.0%) were Christians, 2 (1.7%) respondents were Moslems, while 4 (3.3%) respondents were African traditional religion worshippers.
| Variables | Frequency | Percentage (%) | Mean (X) |
|---|---|---|---|
| Age | |||
| Below 25 | 15 | 12.4 | 34 |
| 26 - 34 | 31 | 25.6 | |
| 35- 44 | 22 | 18.2 | |
| 45-54 | 25 | 20.7 | |
| 55 years & above | 28 | 23.1 | |
| Gender | |||
| Male | 79 | 65.3 | |
| Female | 42 | 34.7 | |
| Marital status | |||
| Married | 34 | 28.1 | |
| Cohabiting | 58 | 47.9 | |
| Divorced | 21 | 17.4 | |
| Widow | 8 | 6.6 | |
| Educational Qualification | |||
| Primary education | 18 | 14.9 | |
| Secondary education | 67 | 53.4 | |
| Tertiary education | 36 | 29.8 | |
| Occupation | |||
| Civil servant | 30 | 24.8 | |
| Unemployed | 29 | 24 | |
| Business/traders | 25 | 20.6 | |
| Student | 37 | 30.6 | |
| Religion | |||
| Christians | 115 | 95 | |
| Muslims | 2 | 1.7 | |
| African traditional religion | 4 | 3.3 | |
Table 1:Socio-demographic data.
Results in Table 2 revealed that majority of the respondents, 90 (74.4%) agreed that they always keep their mental health problem hidden from others due to fear of stigmatization, but 31 (25.6%) respondents disagreed. seventy-five (62.0%) respondents revealed that they don’t have any close personal relationship due to fear of stigmatization, but 46 (38.0%) respondents did not. Also, 101 (83.5%) respondents reported that they often isolate from others because I fear I might be discriminated, but 20 (16.5%) respondents did not. Furthermore, 81 (66.9%) respondents asserted that they no longer find meaning in life because of the people take them. Also, 67 (55.4%) respondents asserted that they no longer feel the need to seek help, but 54 (44.6%) respondents did not. Lastly, 65 (53.7%) respondents agreed that they sometimes have suicidal thoughts as a result of unfair treatment from others, but 56 (46.3%) respondents did not. In addition, the table showed that the total mean score obtained by the respondents is 9.96 out of 15.0. The highest mean score per item is 1.83 out of 3.0, and it was obtained on psychological impact of stigmatization on associating with people. This is followed by a mean score of 1.74 which is obtained on psychological impact of stigmatization on keeping condition away from people. The lowest mean score per item is 1.53 out of 3.0, and it was obtained on psychological impact of stigmatization and discrimination on the thought of suicidal. This is followed by a mean score of 1.55 which is obtained on the psychological impact of stigmatization and discrimination on hopefulness.
| Statements | Responses | |||||
|---|---|---|---|---|---|---|
| Agreed | % | Disagreed | % | ∑ | (X) | |
| I always keep my mental health problem hidden from others due to fear of stigmatization. | 90 | 74.4 | 31 | 25.6 | 211 | 1.74 |
| I don’t have any close personal relationship due to fear of stigmatization. | 75 | 62 | 46 | 38 | 196 | 1.62 |
| I often isolate from others because I fear of unfair treatment from people. | 101 | 83.5 | 20 | 16.5 | 222 | 1.83 |
| I no longer find meaning in life because of the way people take me. | 81 | 66.9 | 40 | 33.1 | 202 | 1.67 |
| I no longer feel the need to seek help.. | 67 | 55.4 | 54 | 44.6 | 188 | 1.55 |
| I sometimes have suicidal thoughts as a result of unfair treatment from others | 65 | 53.7 | 56 | 46.3 | 186 | 1.53 |
| Total mean±(SD) score = | 9.96 | |||||
Decision: Mean (X) ± SD score < 1.5 = low impact, while 1.5 & above = high impact.
Table 2:Psychological impact of stigmatization and discrimination among persons with mental disorders at federal neuropsychiatric hospital calabar(n = 121).
Results in Table 3 revealed that most of the respondents, 87 (71.9%) agreed that they find it difficult to attend religious meetings as a result of stigmatization, but 34 (28.1%) respondents disagreed. One hundred and four (104 (86.0%) respondents stated that they always shy away from participating in their neighborhood activities due to fear of stigmatization, but 17 (14.0%) respondents did not. Also, 78 (64.5%) respondents asserted that it is difficult for them to go to a regular health facility due to fear of discrimination, but 43 (35.5%) respondents did not. Furthermore, majority of the respondents, 102 (84.3%) Maintained that they no longer participate in their family activities due to mental health problem, but 19 (15.7%) respondents did not. Also, 68 (56.2%) respondents agreed that they are still employed despite their mental health conditions, but 53 (43.8%) respondents disagreed. Lastly, 71 (58.7%) respondents asserted that they still engage in my daily activities and means of livelihood despite my mental health condition, but 42 (10.6%) respondents disagreed. In addition, the table showed that the total mean score obtained by the respondents is 10.2 out of 15.0. The highest mean score per item is 1.86 out of 3.0, and it was obtained on social impact of stigmatization on participating in neighborhood activities. This is followed by a mean score of 1.84 which is obtained on social impact of stigmatization on participating in family activities. The lowest mean score per item is 1.56 out of 3.0, and it was obtained on social impact of stigmatization on client’s occupation. This is followed by a mean score of 1.59 which is obtained on social impact of stigmatization on daily activities.
| Statements | Responses | ||||||
|---|---|---|---|---|---|---|---|
| Agreed | % | Disagreed | % | ∑ | (X) | ||
| I find it difficult to attend religious meetings as a result of stigmatization | 87 | 71.9 | 34 | 28.1 | 208 | 1.71 | |
| I always shy away from participating in my neighborhood activities due to fear of stigmatization. | 104 | 86 | 17 | 14 | 225 | 1.86 | |
| It is difficult for me to go to a regular health facility due to fear of discrimination. | 78 | 64.5 | 43 | 35.5 | 199 | 1.64 | |
| I no longer participate in my family activities due to mental health problem | 102 | 84.3 | 19 | 15.7 | 223 | 1.84 | |
| I am still employed despite my mental health condition. | 68 | 56.2 | 53 | 43.8 | 189 | 1.56 | |
| I still engage in my daily activities and means of livelihood despite my mental health condition. | 71 | 58.7 | 50 | 41.3 | 192 | 1.59 | |
| Total mean ± (SD) score = | 1236 | 10.2 | |||||
Decision: Mean (X) ± SD score < 1.5 = low impact, while 1.5 & above = high impact.
Table 3: Social impact of stigmatization and discrimination among persons with mental disorders at federal neuropsychiatric hospital calabar (121).
Results in Table 4 revealed that majority of the respondents, 88 (72.7%) copes with stigmatization by voiding negative information that is anger-in associated then cope by withholding angry emotions, but 33 (27.3%) respondents do not. Ninety-three 93 (76.9%) respondents use positive thinking that tries to alter the way he/she thinks or feels about stigma and discrimination, but 28 (23.1%) respondents do not. Also, 84 (69.4%) respondents often use recreational activities to overcome stigmatization, but 37 (30.6%) respondents do not. Furthermore, 93 (76.9%) respondents get relief from stigmatization by interprets a situation or stressor as modifiable; use of problem-solving skill, planning, and information seeking, but 28 (23.1%) respondents do not. Also, 76 (62.8%) respondents cope by attending social support groups that help them vent emotions, but 45 (37.2%) respondents do not. Lastly, 69 (57.0%) respondents cope by focus on religiosity and finding comfort in religious and spiritual beliefs, but 52 (43.0%) respondents do not. In addition, the table showed that the total mean score obtained by the respondents is 10.16 out of 15.0. The highest mean score per item is 1.77 out of 3.0, and it was obtained on using positive thinking that tries to alter the way he/she thinks or feels about stigma and discrimination. This is followed by a mean score of 1.76 which is obtained on interprets a situation or stressor as modifiable; use of problem-solving skill, planning, and information seeking. The lowest mean score per item is 1.57 out of 3.0, and it was obtained on Focus on religiosity and finding comfort in religious and spiritual beliefs.
| Statements | Responses | |||||
|---|---|---|---|---|---|---|
| Agreed | % | Disagreed | % | ∑ | (X) | |
| Avoiding negative information that is anger-in associated then cope by withholding angry emotions | 88 | 72.7 | 33 | 27.3 | 209 | 1.73 |
| Positive thinking that tries to alter the way he/she thinks or feels about stigma and discrimination | 93 | 76.9 | 28 | 23.1 | 214 | 1.77 |
| Often use recreational activities to overcome stigmatization. | 84 | 69.4 | 37 | 30.6 | 205 | 1.69 |
| Interprets a situation or stressor as modifiable; use of problem-solving skill, planning, and information seeking. | 93 | 76.9 | 28 | 23.1 | 214 | 1.76 |
| Often attend social support groups that help me used venting of emotions | 76 | 62.8 | 45 | 37.2 | 197 | 1.63 |
| Focus on religiosity and finding comfort in religious and spiritual beliefs has helped in adaptation. | 69 | 57 | 52 | 43 | 190 | 1.57 |
| Total mean ± (SD) score = | 1229 | 10.16 | ||||
Decision: Mean (X) ± SD score < 1.5 = low impact, while 1.5 & above = high impact.
Table 4: Coping strategies adopted by persons with mental disorders at federal neuropsychiatric hospital calabar (121).
Testing for Hypothesis
Null Hypothesis: There is no significant relationship between age and the psychological impacts of stigmatization and discrimination among patients with psychiatric disorders.
Alternate Hypothesis: There is a significant relationship between age and the psychological impacts of stigmatization and discrimination among patients with psychiatric disorders.
The result Chi-square (X2) analysis in Table 5 revealed that the calculated value of 37.53 is higher than the critical value of 9.49 at 0.05 level of significant with 4 degrees of freedom. This implies that the result is significant; therefore, the null hypothesis which stated that there is no significant relationship between age and the psychological impacts of stigmatization and discrimination among patients with psychiatric disorders was rejected. Hence, the alternate hypothesis that there is a significant relationship between age and the psychological impacts of stigmatization and discrimination among patients with psychiatric disorders was accepted. From the result, older patients suffering from mental health disorders were more likely to experience psychological impacts of mental health disorders than younger patients. The higher the age of a mental health patient, the higher the psychological impact of stigmatization and discrimination suffered by the patient.
| Age | Psychological impacts | Total | df | Sig. | X2 Crit |
X2 Cal |
Decision | |
|---|---|---|---|---|---|---|---|---|
| Low impact | High impact | |||||||
| Below 25 | 7 | 9 | 15 | 4 | 0.05 | 9.49 | 37.53 | Rejected |
| 26 - 34 | 13 | 15 | 31 | |||||
| 35- 44 | 9 | 13 | 22 | |||||
| 45-54 | 10 | 16 | 25 | |||||
| 55 & above | 9 | 19 | 28 | |||||
| Total | 46 | 73 | 121 | |||||
Significant at 0.05; df = 4, X2 Crit = 5.99; X2 Cal = 37.53.
Table 5: Chi-square (X2) analysis of age and the psychological impacts of stigmatization and discrimination among patients with psychiatric disorders (N = 121).
Discussions of Findings
The findings of this study revealed that persons with mental disorders always keep their mental health problem hidden from others and isolate themselves from people due to fear of being stigmatized and discriminated. Some prefer not to have close personal relationship; others consider life to be meaningless and sometimes had suicidal thoughts as a result of unfair treatment from people. This implies that most persons who are being discriminated may have prolong healing and recovering process. More awareness is needed to educate the society on the effect of discrimination against the mentally ill persons. This will go along way to help in integration of persons with mental disorders. These findings correspond with a study (Picco, et al. 2016), who maintained that persons with mental disorders reported having feelings of hopelessness and significantly higher frequencies of suicidal ideation due to stigmatization. Similarly, finding was consistent with a study (Morgades, et al. 2019) whose findings showed that person’s suffering from mental health disorders were associated with self-isolation and thoughts of suicide. Another related study by (Armiyau, 2015) who maintained that persons with mental disorders have selfisolation, self-confinement and self-alienation due to fear of stigmatization and discrimination.
The findings also revealed that majority of respondents find it difficult to attend religious meetings as a result of stigmatization. Also, they always shy away from participating in their neighborhood and family activities, and some find it difficult to go to a regular medical checkup due to fear of discrimination. This finding is consistent with a study by (Li, et al. 2020) whose findings maintained that person with mental disorders have impaired social inequality of life regarding group association, attending religious gatherings, participating in neighborhood and family activities.
Furthermore, the findings revealed that the coping strategies adopted by persons with mental disorders were avoiding negative information that anger-in associated by withholding angry emotions, positive thinking that alter the way he/she thinks or feels about stigma and discrimination, attending social support groups, and cope by focus on religiosity. This finding corresponds with a study by (Karnieli, et al. 2013) whose findings revealed that in order to increase persons with mental disorders social functioning and reduce the stress of stigmatization; individuals with mental disorders associate themselves with social groups. Similarly, the findings agree with findings by researcher (Oyira, et al. 2019), who found out that persons with mental disorders reported being personally discriminated against because of their mental illness, are more likely to identify with other people with mental illnesses; those who socially identify with other people with mental illnesses tend to have better well-being because they perceive their in-group as a source of social support.
Implication to Nursing: This study could create awareness and consciousness on the psychosocial impacts of stigmatization and discrimination among persons with mental disorders. It will also give nurse educators and nurses in general an insight into the coping strategies adopted by persons with mental disorders. They will therefore strategize towards sensitizing the general public for avoidance of stigmatization and discrimination of persons with mental disorders. Also, persons with mental disorders will be educated on how to cope with their health condition, and this will enable them function effectively in the society.
Conclusion
The Based-on findings of the study; it was concluded that stigmatization and discrimination have significant impact on psychosocial wellbeing resulting in self-isolation, avoidance of close personal relationship and a major cause of suicidal thoughts. Also, it was recommended that health policy makers, hospital managements and nurse leaders should educate persons with psychiatric disorders on coping strategies and organize regular mass orientation and sensitization programs for the general public against stigmatization and discrimination. This will help to change negative beliefs and perceptions leading to stigmatization and discrimination of persons with psychiatric disorders. Members of the society, family members of people with psychiatric disorders should love and care for their relatives with psychiatric disorders.
References
Armiyau, A.Y. (2015). A review of stigma and mental illness in Nigeria. Journal of Clinical Case Report, 5(1), 1-3.
Indexed at, Google Scholar, Crossref
British Council. Next generation Kenya: listening to the voices of young people. 2018.
Chan, K. K. S., & Fung, W. T. W. (2019). The impact of experienced discrimination and self-stigma on sleep and health-related quality of life among individuals with mental disorders in Hong Kong. Quality of Life Research, 28(8), 2171-2182.
Indexed at, Google Scholar, Crossref
Hipes, C., Lucas, J., Phelan, J. C., & White, R. C. (2016). The stigma of mental illness in the labor market. Social Science Research, 56, 16-25.
Indexed at, Google Scholar, Crossref
Karnieli-Miller, O., Perlick, D. A., Nelson, A., Mattias, K., Corrigan, P., & Roe, D. (2013). Family members of persons living with a serious mental illness: Experiences and efforts to cope with stigma. Journal of Mental Health, 22(3),254-262.
Indexed at, Google Scholar, Crossref
Li, XH., Zhang, TM., Yau, YY., Wang, YZ., Wong, YLI., Yang, L., et al. (2020). Peer-to-peer contact, social support and self-stigma among people with severe mental illness in Hong Kong. International Journal of Social Psychiatry, 67(6), 622-631.
Indexed at, Google Scholar, Crossref
Morgades-Bamba CI, Fuster-Ruizdeapodaca MJ, Molero F. (2019). Internalized stigma and its impact on schizophrenia quality of life. Psychol Health Med. 24(8), 992-1004.
Indexed at, Google Scholar, Crossref
Oexle, N., Ajdacic-Gross, V., Kilian, R., Mueller, M., Rodgers, S., Xu, Z. et al. (2017). Mental illness stigma, secrecy and suicidal ideation. Epidemiology and psychiatric sciences, 26(1), 53-60.
Indexed at, Google Scholar, Crossref
Oyewunmi, A. E., Oyewunmi, O. A., Iyiola, OO, & Ojo, A. Y. (2015). Mental health and the Nigerian workplace: Fallacies, facts and the way forward. International Journal of Psychology and Counselling, 7(7), 106-111.
Indexed at, Google Scholar, Crossref
Oyira, E. J. & Agba, M. (2019). Prevalence, and Outcome of Management of Major Depressive Disorder among Patients in Federal Neuro-Psychiatric Hospital, Calabar, Cross River State, From January, 2012 to December, 2014. Sumerianz Journal of Medical and Healthcare, 2(7),70-79.
Picco, L., Pang, S., Lau, Y. W., Jeyagurunathan, A., Satghare, P., Abdin, E., et al. (2016). Internalized stigma among psychiatric outpatients: Associations with quality of life, functioning, hope and self-esteem. Psychiatry research, 246, 500-506.
Indexed at, Google Scholar, Crossref
Talatala, M., Ramano, E., & Chiliza, B. (2020). Reducing psychosocial disability for persons with severe mental illness in South Africa. South African Health Review, 2020(1), 11-18.
Share This Article
Open Access Journals
Article Usage
- Total views: 1436
- [From(publication date): 0-2022 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1076
- PDF downloads: 360
