Psychomotor Aging in Lebanon: Reliability and Validity of the Geriatric Psychomotor Examination
Received: 30-Aug-2017 / Accepted Date: 01-Sep-2017 / Published Date: 08-Sep-2017 DOI: 10.4172/2161-0460.1000372
Abstract
Objective: This study targets the standardization of the Geriatric Psychomotor Examination (GPE) that evaluates motor skills, time, memory, attention and perception among Lebanese elderly population.
Methods: The GPE, created in France and recently standardized in Portugal is now translated to Arabic and standardized in Lebanon on a sample of 381 people aged 60 years and above. Five raters collected data during two years. Apparent and construct validity, homogeneity and internal consistency, inter-observer and test-retest reliability of the tool were tested. This tool’s sensitivity to different populations was subsequently assessed.
Results: The GPE’s psychometric properties enable it to accurately define the progressive decrease in Lebanese elderly psychomotor skills. Comparison with the French agers shows the latter ones seem to preserve better capacities than Lebanese elders. Discussion: This difference can be analyzed in a holistic socio-cultural perspective and raises questions about new policies to enhance the elderly integration in Lebanon.
Keywords: Psychomotor assessment; Standardization; Cross cultural comparison
Introduction
One of the worldwide concerns of contemporary medical and paramedical fields is improving older people’s quality of life as well as lengthening its expectancy. This requires a deeper understanding of the cognitive, motor, psychological and social challenges, changes and issues of elderly. All these aspects are central to the psychomotor holistic view of the person, specifically the aging one. Through aging, several processes simultaneously operate at different levels of functional organization, resulting in age-related physiological and psychomotor changes [1-3]. Sensory (sight and hearing) and balance impairments increase the risk of falls [4]. In addition, modifications of the CNS through aging are considered a major cause of all the other changes in psychomotor skills. Brain atrophy (i.e., reduction in brain volumes particularly the medial temporal lobe, hippocampus and entorhinal cortex) [5] reduction of white substance, decreased cerebral plasticity and increased brain cells mortality, along with neurochemical changes in the brain interfere with the cognitive functions, leading to a reduction of older adults’ autonomy [6]. Moreover, a large decrease of motor performance is observed in older people [2]. This is associated with previously mentioned CNS changes, cognitive modifications and changes in peripheral structures, which explain difficulties to perform functional activities of daily life and increase risk of falls. The reaction time after a specific stimulus is globally increased in older people as they need more time to analyze a stimulus and choose the appropriate reaction. The movement duration increases by giving priority to movement accuracy at the cost of its speed. Decline in bimanual coordination increases with task complexity and movement frequency [7]. Older adults also exhibit a greater variability of movements [8].
Therefore, one of the main roles of the psychomotor therapist is acknowledging the usual, spontaneous and normal aging process among the population, before implementing efficient curative and palliative procedures in therapy [9,10]. However, few studies concerning the psychomotor impact of aging have been reported. This is partially due to the absence of specific psychomotor evaluation instruments for the elderly [11]. The inexistence of reference standards for the elderly population in general also highlights the importance of studying the psychomotor skills of the geriatric population associated with physical or mental decline associated to specific conditions such as dementia, Parkinson’s or Alzheimer’s disease [12]. Therefore, with longer life expectancy around the world [13], a raising concern has been recently attached to the means of offering an accurate approach of aging populations. Medical and paramedical (psychological, social, psychomotor, occupational, etc.) specialists are focusing on the development of a research-based approach to cover all of the aging people’s health and well- being concerns.
In the psychomotor conceptual framework, elders approach is similar to the youth. Based on a holistic view of the human being, psychomotor therapy is a complement and support for the pharmacological and medical treatment. It intends to work on disturbed motor, cognitive, perceptual, emotional and behavioral functions [14]. It starts with an assessment that aims to clarify and complement the clinical diagnosis and enable detailed study of psychomotor symptoms concerning etiology, detailed performance and pathological processes description. This is followed by the confrontation of the assessment’s results with other medical and paramedical evaluations in order to guide the implementation of a holistic project for the patient [15]. There are few psychomotor assessment scales validated with elderly populations [11] and none validated in Lebanon. To overcome this situation, professionals often use unidimensional scales, such as cognitive functions tests (e.g. the Mini Mental State Examination, the Clock drawing test), tests for perceptual and spatial functions (e.g. the Benton facial recognition test) and balance scales (e.g. the Tinetti scale) [11,16]. Therefore, the need for a global, detailed and specific psychomotor tool becomes a necessity.
In this perspective, the main objective of the present study is to translate, adapt and standardize the GPE in order to use it by psychomotor practitioners in Lebanon. This will likely complement clinical diagnosis and help planning multidisciplinary intervention.
Materials and Methods
Presentation of the geriatric psychomotor examination
The GPE is intended to assess psychomotor skills and some cognitive functions in aging population and to screen for pathological symptoms, particularly for people affected by Alzheimer’s disease and other dementias. It was created and standardized by Michel et al. [17] in order to bolster the given care by evaluating the perceptual, motor and cognitive aspects of older patients, associating the technical assessment to a rigorous holistic clinical observation. This assessment is conceived to highlight the symptomatology of a diagnosis, help adjust the palliative and curative procedures and clarify the expected long term prognostic.
The French standardization was made with a sample of 492 participant aged 60 and above [17]. A Portuguese version of the GPE was recently adapted (P-EGP), validated and standardized by Morais et al. [18] with a sample of 497 elders aged between 60 and 99 years. This standardization included the testing of content validity, internal consistency reliability of the items, tool’s stability using test-retest reliability and proportion of agreement between experts and the kappa statistic.
The GPE includes 17 items that measure static and dynamic balance, joint mobilization, praxis, fine motor skills of upper and lower limbs, knowledge of body parts, perception, perceptive and verbal memory, space and time fields, vigilance, verbal and non-verbal communication (Table 1).
| Static coordination I | Stability in standing position |
| Static coordination II | Balance in different positions (unipedal stand, bipedal tiptoe, unipedal tip-toe) |
| Dynamic coordination I | Quality of walking |
| Dynamic coordination II | Fast walking - Running over a short distance |
| Joint mobilization of upper limbs | Passive mobilization of upper limbs joints (wrist, elbow and shoulder) |
| Active mobilization of upper limbs joints | |
| Joint mobilization of lower limbs | Passive mobilization of lower limbs joints (ankle, knee and hip) |
| Active mobilization of lower limbs joints | |
| Upper extremity fine motor skills | Eye-hand coordination |
| Fingers dexterity (finger drumming, finger-thumb opposition, picking a coin, buttoning) | |
| Lower extremity fine motor skills | Eye-foot coordination (foot placement, kicking a ball, pointing with foot) |
| Praxis | Ideomotor praxis (pantomime) |
| Ideational praxis (use of cutlery) | |
| Visuo-constructive praxis (construction with cubes) | |
| Writing skills (copying shapes) | |
| Body part knowledge | Identification, designation and naming of body parts |
| Imitation of gestures | |
| Vigilance |
Preparatory attention |
| Shapes and colors identification | |
| Execution of instructions | |
| Attention span | |
| Perceptual memory | Recall of previously seen colours and body positions |
| Space field | Knowledge of basic spatial concepts |
| Geographical location and orientation | |
| Orientation using right/left concepts | |
| Estimation of measures | |
| Line bisection | |
| Verbal memory | Words encoding |
| Words recalling after a time lap | |
| Perception | Auditory perception |
| Reproduction of rhythmic structures | |
| Familiar theme recognition | |
| Image recognition | |
| Stereognosis | |
| Visual identification of images and letters (reading skills) | |
| Time field | Knowledge of days, months, current and birth dates |
| Reading time | |
| Reordering sequence of events | |
| Language consistency | |
| Communication | Language consistency |
| Face expressivity | |
| Adequacy of nonverbal communication | |
| Comprehension of instructions |
Table 1: Description of the geriatric psychomotor examination’s 17 items.
Each item is scored on a six points scale with a maximal total score of 102 points. The order of application of the items can vary according to the subject’s availability, with the exception of three items assessing memory (items 10, 11 and 12) that must be applied in a specific sequence and time interval. A pause is recommended at item 10.4 if the subject is feeling tired, in pain or uncomfortable. Some items can be skipped in case of pain, fatigue or awareness trouble. The overall examination time for these 17 items should not exceed one hour. The psychomotor therapist decides whether the assessment should be done during one, two or three sessions, depending on the patient’s attention span, awareness and physical weariness. However, the overall assessment period should not be too long in order to preserve the results’ coherence. The GPE also involves clinical observation to report qualitative aspects such as posture, tonic- emotional reactions, quality of the movement, laterality, tremors and involuntary movements, etc. [15]. Evaluation can be repeated every 3 to 6 months especially if the patient is undergoing a psychomotor treatment. It is important to clarify the assessment goals for the patient in order to enhance his active adherence throughout the evaluation process. It is also essential to synthesize the results for the patient and give him the possible adaptive strategies to reinforce his daily autonomy.
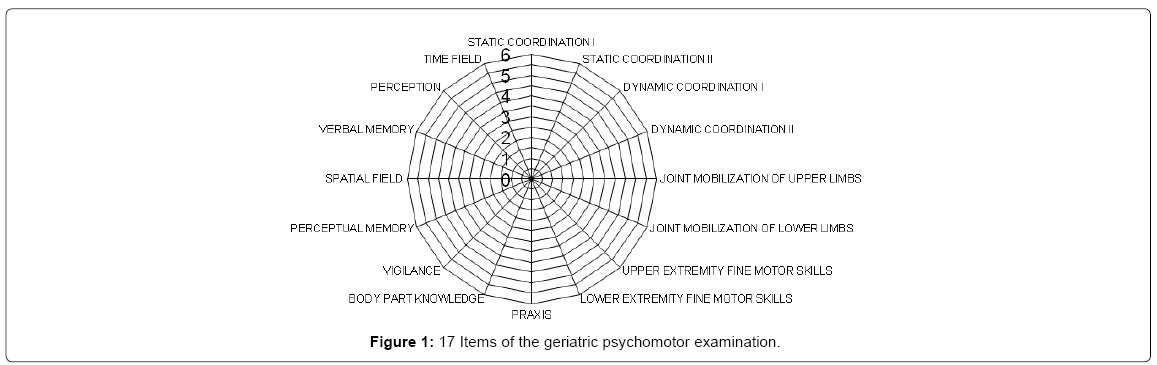
After the assessment, a synthesis Radar chart can highlight 16 psychomotor aspects evaluated by the GPE. Each item’s score is positioned on the appropriate segment. Once linked together, these points offer a holistic view of the strengths and weaknesses of the patient (Figure 1).
Translation of the text used in “perception” item and of words used in “verbal memory” items was done by the researcher, native speaker of Arabic and teaching in French. The translation was then validated by two judge raters, both native speakers of Arabic and proficient in French. The first rater was a Lebanese language and speech therapist, practicing in French and in Arabic with adult and senior patients. The second rater held an Arabic literature PhD degree. Both raters agreed on the construction and characteristics of the text as well as on the simplicity of the words chosen to be easily memorized.
Examination conditions
The administration conditions remained the same during all the examinations: they were all done individually in a quiet room with sufficient lightning. During this study the order in which the items were presented was systematically modified using a Latin square design, to avoid any order effect on the results. The assessment material was presented to the patient and then taken back and put out of sight to prevent his distractibility.
Five psychomotor therapists were involved in the data collection. They were previously trained by the researcher on the administration and scoring of the GPE. They proceeded separately and data was collected during two consecutive years. Application’s duration was of 50-70 min each.
Sampling participants
381 participants were enrolled in this study. The selection was made by combining an accidental sampling method (according to availability) and a purposive sampling method, thus choosing participants according to specific inclusion and exclusion criteria.The primary inclusion criterion was age (60 years and above). Two other major criteria were also defined for the selection:
Autonomy in daily life tasks (capability of self-care) which was confirmed by questions addressed to the subject himself or to the nursing staff in the nursing homes. Absence of major motor, sensory or cognitive impairment (neuro-degenerative pathologies, dementia, Parkinson’s disease, cerebrovascular accident, etc.). And absence of any non-stable psychiatric illness which was confirmed by the medical report of every participant.
Participants were chosen from different areas: residential homes (48%) and nursing homes (52%) distributed in the five Lebanese districts (Beirut, Mount Lebanon, South Lebanon, North Lebanon and the Bekaa Valley).
The field researchers clearly explained the study’s objectives to all participants. Anonymity was guaranteed to participants and to nursing homes’ administrations. Informed oral consent was given by all subjects prior to the GPE assessment.
Data Analysis
Participants were divided by gender and by age groups to enable the comparison between them (Table 2). Data was treated and analyzed using the Statistical Package for Social Sciences (SPSS), version 21. An analysis of variance (ANOVA) was used to compare the total scores and the 17 items scores of the different age groups. A preliminary analysis of variance (sex × age) was conducted on all the variables and showed no significant differences according to gender. Further analysis was performed using only the age variable. The statistical significance level retained was a value of p<0.05. Tukey’s post-hoc test was used to compare differences between the six age groups.
| Age (y;m) | Women | Men | Total | Mean (SD) | SeM |
|---|---|---|---|---|---|
| 60-64;11 | 38 | 26 | 64 | 94.1 (6.1) | 0.76 |
| 65-69;11 | 41 | 38 | 79 | 90.6 (8.4) | 0.94 |
| 70-74;11 | 44 | 37 | 81 | 84.2 (11.4) | 1.26 |
| 75-79;11 | 31 | 29 | 60 | 82.3 (9.7) | 1.25 |
| 80-84;11 | 38 | 27 | 65 | 78.9 (11.7) | 1.45 |
| Above 85 | 20 | 12 | 32 | 81.0 (12.3) | 2.17 |
| Total | 212 | 169 | 381 |
Table 2: Distribution, mean, standard deviation and standard error of the mean of the sample according to age and sex.
The following psychometric properties of the GPE were assessed:
Apparent validity was achieved by the judgement of French and Lebanese experts in gerontology and geriatrics (physician, neuropsychologist, and psychomotor therapist).
Construct validity was investigated by testing a pathological group of 66 participants (51 women and 15 men) suffering from dementia (Alzheimer’s disease or related pathologies) whose average age is 72 years 2 months (youngest=53 years 2 months; oldest=99 years 4 months). An analysis of variance was then conducted to compare their results to those of a control group matched on age and sex.
Homogeneity was studied using the split-half method by dividing the items in two groups: pairs and odds before testing the correlation between them using the Pearson test.
Internal consistency was evaluated by using the Cronbach’s alpha coefficient.
Inter-observer reliability consisted in doing 33 examinations in the presence of two observers who were independently noting the results of the subjects. An observation of the average difference of points noted was then realized.
Test-Retest Reliability was investigated on 20 examinations that were done for the same participants and repeated after a period of 15 days. The comparison of the results of the two examinations was realized using the paired t-test to test the comprehensibility of the instructions, acceptability of time limits, wording of the items, consistency of responses, ensuring that this new version still retained its equivalence in an applied situation.
Results
Total score
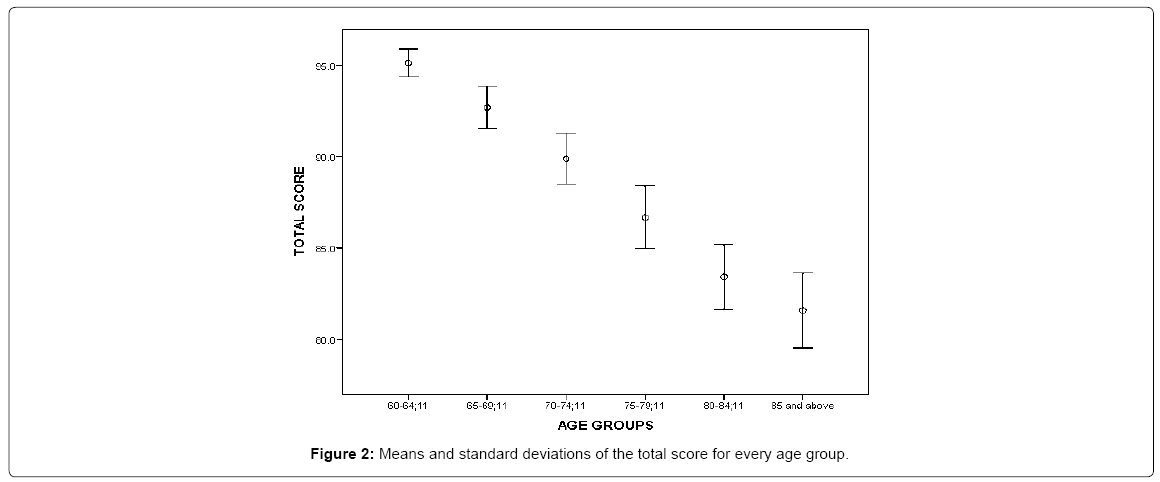
The Total score to the GPE decreases with aging with a mean of 94.05 (SD=6.06) for the sixty-year-old and 81.03 (SD=12.28) for the 85 year old, along with an increasing variability throughout the age groups. The analysis of variance showed a significant difference in the Total scores between the different age groups (F (5,375)=21.92; p<0.0001).
Tukey’s post-hoc test applied to the six age groups showed no significant difference between the first two age groups (60 to 69;11 years) as well as among the rest of the four other groups (70 to 85 and above). This is represented by the error bars in Figure 2 showing no overlap between the first two age groups and the rest of the groups.
Items scores
The analysis of variance of the items scores according to age showed a significant difference in the scores of the following 15 items: Static coordination I (F (5,375)=7.06; p<0.0001); Static coordination II (F (5,375)=16.18; p<0.0001); Dynamic coordination I (F (5,375)=5.29; p<0.0001); Dynamic coordination II (F (5,375)=23.22; p<0.0001); Joint mobilization of upper limbs (F (5,375)=2.38; p<0.05); Upper extremity fine motor skills (F (5,375)=5.37; p<0.0001); Praxis (F (5,375)=9.25; p<0.0001); Body part knowledge (F (5,375)=8.62; p<0.0001); Vigilance (F (5,375)=8.38; p<0.0001); Perceptual memory (F (5,375)=8.20; p<0.0001); Space field (F (5,375)=10.52; p<0.0001); Verbal memory (F (5,375)=6.91; p<0.0001); Perception (F (5,375)=14.40; p<0.0001); Time field (F (5,375)=14.70; p<0.0001); Communication skills (F (5,375)=8.26; p<0.0001).
In two items, age doesn’t have a significant effect: Joint mobilization of lower limbs (F (5,375)=1.51; ns) and Lower extremity fine motor skills (F (5,375)=1.29; ns) (Table 3).
| Age | 60-64;11 | 65-69;11 | 70-74;11 | 75-79;11 | 80-84;11 | Above 85 |
|---|---|---|---|---|---|---|
| Items | (N=64) | (N=79) | (N=81) | (N=60) | (N=65) | (N=32) |
| Static coordination I | 5.9 (0.2) | 5.9 (0.2) | 5.7 (0.6) | 5.9 (0.4) | 5.6 (0.5) | 5.6 (0.6) |
| Static coordination II | 4.6 (1.3) | 4.0(1.2) | 3.3(1.5) | 3.1(1.4) | 2.7 (1.6) | 2.8 (1.6) |
| Dynamic coordination I | 5.9 (0.3) | 5.9 (0.3) | 5.7 (0.6) | 5.8 (0.5) | 5.6 (0.6) | 5.6 (0.8) |
| Dynamic coordination II | 5.1 (1.4) | 4.6 (1.9) | 3.1 (2.1) | 2.7 (1.8) | 2.4 (2.1) | 2.4 (2.3) |
| Joint mobilization of upper limbs | 5.1 (0.9) | 5.0 (1.1) | 4.9 (1.3) | 5.4 (0.9) | 5.4 (1.2) | 5.4 (0.9) |
| Joint mobilization of lower limbs | 4.9 (1.2) | 4.8 (1.2) | 4.5 (1.4) | 4.9 (1.2) | 4.5 (1.8) | 4.5 (1.6) |
| Upper extremity fine motor skills | 5.4 (0.8) | 5.3 (0.9) | 4.9 (1.2) | 4.9 (1.1) | 4.7 (1.1) | 4.9 (1.0) |
| Lower extremity fine motor skills | 5.9 (0.2) | 5.7 (0.4) | 5.6 (0.8) | 5.7 (0.6) | 5.7 (0.9) | 5.8 (0.6) |
| Praxis | 5.8 (0.5) | 5.5 (0.6) | 5.3 (0.9) | 5.1 (1.1) | 4.8 (1.1) | 5.2 (0.8) |
| Body part knowledge | 5.8 (0.4) | 5.8 (0.4) | 5.6 (0.6) | 5.4 (0.6) | 5.2 (0.8) | 5.5 (0.6) |
| Vigilance | 5.7 (0.6) | 5.7 (0.7) | 5.3 (0.9) | 5.3 (0.9) | 4.9 (1.1) | 5.2 (1.0) |
| Perceptual memory | 5.3 (0.9) | 5.0 (1.1) | 4.6 (1.3) | 4.4 (1.5) | 4.1 (1.6) | 4.2 (1.3) |
| Space field | 5.7 (0.5) | 5.3 (0.8) | 5.1 (0.9) | 4.9 (1.2) | 4.7 (1.0) | 4.7 (1.2) |
| Verbal memory | 5.4 (0.6) | 5.3 (0.8) | 1.1 (4.9) | 4.8 (1.0) | 4.7 (1.0) | 5.0 (0.8) |
| Perception | 5.6 (0.5) | 5.4 (0.8) | 4.9 (0.9) | 4.7 (1.1) | 4.4 (1.3) | 4.7 (1.2) |
| Time field | 5.7 (0.8) | 5.3 (0.9) | 4.8 (1.3) | 4.6 (1.4) | 4.1 (1.7) | 4.1 (1.7) |
| Communication | 5.9 (0.4) | 5.7(0.7) | 5.5(0.9) | 4.9(1.5) | 5.2(1.2) | 5.1(1.5) |
Table 3: Means and standard deviations of items scores according to age.
Construct validity
The construct validity of the tool is measured by comparing the “normal” sample results to those of a pathological group. This comparison was made between a group of 66 participants suffering from dementia (Alzheimer’s disease) who are not part of the original research sample, and a control group of 66 participants from the original sample. It highlighted lower and more variable overall scores among the pathological sample (M=68.8; SD=17.3) as compared to the control subjects (M=87; SD=8.8) with a significant difference F (1,130)=52,05; p<0.0001).
Homogeneity and internal consistency
Homogeneity study showed a high correlation with r=0.80 (p<0.0001). This leads to the conclusion that the GPE tool measures the same dimension in its different parts. The Cronbach’s alpha coefficient showed a strong internal consistency (α=0.87).
Inter-observer reliability
The average difference among the 33 examinations noted by two observers was of 1 point over the total number of assessments; with a maximal difference of 5 points for one participant only. This indicates that the scoring criteria are well defined.
Test-retest reliability
The comparison between the 20 assessments repeated after 15 days showed no difference between them (t (19)=0.82; ns.) which proves the stability of the GPE over time.
Comparison between the Lebanese and the French Results
The average of Lebanese results are all lower than those of French results and their standard deviations are larger which implies more dispersion among Lebanese population’s results. However, Pearson’s correlation test applied to the Means of both populations’ total scores indicates a positive correlation between them: r=0.28. Therefore, Total scores Means regress in a similar way throughout the six age groups among the French and the Lebanese population.
The analysis of variance applied to the Total scores Means of the French and Lebanese results shows a significant effect of the Country F (1,861)=95.32; p
In order to investigate this significant difference of the interaction Country × Age, Tukey’s post-hoc test was applied to the different age groups of both samples. This shows no significant difference between the Total scores of the Lebanese and the French population regarding the first group (60-64 years and 11 months) and the last group of age (85 years and above). However, the results significantly differ among the four intermediate groups (Table 4).
| Age (y;m) | Country | N | Mean (SD) | *p |
|---|---|---|---|---|
| Lebanon | 64 | 94.1 (6.1) | ||
| 60-64;11 | 0.09 | |||
| France | 103 | 95.8 (4.2) | ||
| Lebanon | 79 | 90.6 (8.4) | ||
| 65-69;11 | 0 | |||
| France | 73 | 95.1 (4.8) | ||
| Lebanon | 81 | 84.2 (11.4) | ||
| 70-74;11 | 0 | |||
| France | 105 | 94.2 (5.0) | ||
| Lebanon | 60 | 82.3 (9.7) | ||
| 75-79;11 | 0 | |||
| France | 69 | 90.4 (8.4) | ||
| Lebanon | 65 | 78.9 (11.7) | ||
| 80-84;11 | 0 | |||
| France | 68 | 87.7 (6.5) | ||
| Lebanon | 32 | 81.0 (12.3) | ||
| 85 and above | 0.52 | |||
| France | 74 | 81.8 (9.9) |
Note: Significance level is *p < .05
Table 4: Comparison of total scores of the GPE between the Lebanese and French population.
Discussion
The investigation of changes concerning psychomotor aging among Lebanese population requires the use of a reliable tool that measures different psychomotor aspects without bias. The Geriatric Psychomotor Examination was therefore imported and standardized among a Lebanese representative sample.
Results proved the GPE to be age sensitive. In fact, there is a significant difference according to Total scores throughout the six groups of age previously defined. Further analysis shows that Lebanese psychomotor skills appear to be rather similar in the early aging years (before the age of 70), which may be due to the conservation of a good level of activity as Lebanese retirement is set to the age of 64. Comparison between the French and the Lebanese results showing no significant difference between Total scores of the first group of age confirms the preservation of a high level of functionality regardless of socio-demographic and cultural factors. At the age of 70, a psychomotor decline is noticed among the Lebanese population according to the GPE results which can be associated to CNS modifications gradually occurring. This decline is followed by a mild decrease of the psychomotor skills throughout later years. Therefore, psychomotor skills slowly decrease after the age of 70, with no significant difference between the consecutive groups. This overall similarity after the age of 70 might be due to the homogeneity of the sample chosen for the GPE standardization, which is mainly constituted of people undergoing a “regular” aging process and therefore preserving a similar level of autonomy, daily activity and vigilance.
In addition, GPE seems to be sensitive to functional changes in individuals undergoing a “regular” aging process as compared to those suffering from a specific impairment. It can thus be accurately used as a clinical tool for implementing a psychomotor and multidisciplinary therapy plan, proposing supplementary input for precise diagnosis and for assessing therapy outcomes.
The high correlation and internal consistency between the GPE’s 17 different items confirm its status as a valid tool to measure several psychomotor aspects homogeneously among aging people. The interobserver and the test-retest assessments point out a strong construct validity since GPE results seem to be independent of the rater’s proficiency and remain constant over time. The scoring criteria are therefore well defined to evaluate the desired skills while reducing external bias. These findings enable psychomotor therapists to use the GPE as a reliable clinical and research tool in Lebanon.
The subsequent comparison between Lebanese and French results to the GPE confirmed the sensitivity of this tool to socio-demographic factors. In fact, a significant difference was flagged between the Lebanese and the French psychomotor skills throughout aging. This difference is predominant among the middle groups of age (65 to 85 years). This can be associated to several factors such as health quality, distress and social components that affect the aging process [11], health, distress and social components affect the aging process. In Lebanon, older people are marginalized in the public health policy [19] while excessive health care often becomes a necessity after the age of 70. This might reduce the preservation of their motor and cognitive skills as compared to the French aging population having the advantage of wider gerontology care and assistance [20]. On the social level, the Lebanese functional aging is highly affected by the experience of instability and conflict for several decades [21]. In fact, people aged 65 and above in 2015 are those who were the most functional during the 1970-1990’s Lebanese civil war. This past psychological and physical distress, along with a present continuous lack of security and social instability, lead to chronic anxiety and stress which have been proven to significantly accelerate the aging process [22]. In addition, the education level may also be behind the overall higher scores of the French results as literacy rates are different between both countries. In fact, 99% of the French population is educated, while only 93.9% of the Lebanese people have only benefited from elementary education [23].This affects psychomotor evolution throughout aging for three main reasons: first, education contributes in raising awareness on how to preserve good health since childhood (physical activities, healthy eating, and avoiding environmental unhealthy factors). In addition, education is one of the factors enhancing cognitive reserve: literacy and the pursuit of higher levels of education are considered to provide benefits against cognitive decline, thus preserving cognitive skills longer [24]. And last, better education usually guarantees better working conditions. Hence, older people who did not have access to proper education, are more likely to have worked in high-risk fields increasing their physical fatigue or health problems, which reduces the preservation of their motor skills throughout aging.
On the other hand, the cross-cultural comparison flagged similar regressive directions of Lebanese and French results. This indicates that the GPE measures universal psychomotor skills that similarly evolve throughout aging regardless of the socio-demographic and cultural factors. This is related to the previously mentioned CNS modifications and sensory decline [5] affecting the perceptive, cognitive [6,7] and motor aging [2].
Furthermore, results of Lebanese and French subjects aged 80 years and above do not significantly differ. This might be linked to the fact that the sample chosen from both countries fit in the same “normal aging” criteria: autonomy in daily tasks and absence of sensory impairments and untreated diseases. Therefore, the different aging pathways followed by both elderly populations throughout aging seem to reach the same “final pattern” during the latter years. This can be understood in the perspective of the motor development as conceived by Thelen [25], assuming that this final pattern is the result of biological constraints similar for all populations, indicating a weaker impact of cultural factors after the age of 80.
The GPE appears to be an accurate tool in evaluating the psychomotor aging while being sensitive to elderly impairments and to cultural specificities. It broadly assesses different psychomotor aspects, without being sensitive to inter-judge bias. This standardization procured a pattern to understand the decrease of psychomotor abilities among Lebanese elders and set a general regular aging profile: it pointed out a prominent decline after the age of 70 followed by a mild decrease throughout later years.
Conclusion
The significant difference flagged between the Lebanese and the French aging population favouring the latter one revealed the high impact of multi-causal psychological, educational and socio-cultural factors on psychomotor skills. This finding confirms the need for a reform in the health and education system and policies in Lebanon, along with the necessity to raise awareness regarding the means of preventing early psychomotor decay. Medical, paramedical and social care should be integrated as a holistic support system for promoting a better integration of the older population in the Lebanese society whether in private residences, in nursing homes or in hospitals.
In this perspective, psychomotor intervention should be getting more weight among palliative and curative actions in Lebanon. The use of the GPE in association with other cognitive and functional assessment instruments will enable practitioners to analyze more precisely the modifications, difficulties and needs of normally aging people and of people suffering from specific disabilities or diseases. This will constitute the first pillar stone for proposing adequate intervention plans targeting the well-being and autonomy of older adults.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
The local ethical committee of Saint Joseph University of Beirut reviewed this project and approved its conduct and publication. The approval reference number is USJ-2015-44.
References
- Franceschi C, Valensin S, Bonafè M, Paolisso G, Yashin AI, et al. (2000) The network and remodeling theories of aging: Historical background and new perspectives. Exp Gerontol 35: 879-896.
- Seidler RD, Bernard JA, Burutolu TB, Fling BW, Gordon MT, et al. (2010) Motor control and aging: Links to age-related brain structural, functional and biochemical effects. Neurosci Biobehav Rev 34: 721-733.
- Vaillancourt DE, Newell KM (2002) Changing complexity in human behavior and physiology through aging and disease. Neurobiol Aging 23: 1-11.
- Kulmala J, Viljanen A, Sipilä S, Pajala S, Pärssinen O, et al. (2009) Poor vision accompanied with other sensory impairments as a predictor of falls in older women. Age Ageing 38: 162-167.
- Fjell AM, McEvoy L, Holland D, Dale AM, Walhovd KB, et al. (2013) Brain changes in older adults at very low risk for Alzheimer’s disease. J Neurosci 33: 8237-8242.
- Lemaire P, Bherer L (2005) Psychologie du vieillissement: Une perspective cognitive. Bruxelles: De Boeck Université.
- Goble DJ, Coxon JP, Van Impe A, De Vos J, Wenderoth N, et al. (2010) The neural control of bimanual movements in the elderly: Brain regions exhibiting age-related increases in activity, frequency-induced neural modulation and task-specific compensatory recruitment. Hum Brain Mapp 31: 1281-1295.
- Contreras-Vidal JL, Teulings HL, Stelmach GE (1998) Elderly subjects are impaired in spatial coordination in fine motor control. Acta Psychol (Amst) 100: 25-35.
- Graff MJ, Adang EM, Vernooij-Dassen MJ, Dekker J, Jönsson L, et al. (2008) Community occupational therapy for older patients with dementia and their care givers: Cost effectiveness study. Br Med J 336: 134-138.
- Steultjens EM, Dekker J, Bouter LM, Leemrijse CJ, van den Ende CH (2005) Evidence of the efficacy of occupational therapy in different conditions: An overview of systematic reviews. Clin Rehabil 19: 247-254.
- Albaret JM, Aubert E, Sallagoïty I (2001) Evaluation psychomotrice du sujet âgé. Fam Pract 10: 449-453.
- Scherder E, Dekker W, Eggermont L (2008) Higher-level hand motor function in aging and (preclinical) dementia: Its relationship with (instrumental) activities of daily life: A mini-review. Gerontology 54: 333-341.
- World Health Organization (2016) Number of people over 60 years set to double by 2050; Major societal changes required.
- Michel S, Roux J, Albaret JM, Soppelsa R (2009) L’Examen Géronto-Psychomoteur. Un nouveau-né en gériatrie. Évolutions Psychomotrices 21: 70-78.
- Michel S, Soppelsa R, Albaret JM (2010) Pour une légitimité du travail en géronto- psychomotricité : L’Examen Géronto Psychomoteur. In Entretiens de Psychomotricité 2010: 90-93.
- Hugonot-Diener L, Barbeau E, Michel B F, Thomas-Antérion C, Robert P (2010) Grémoire: Tests et échelles de la maladie d’Alzheimer et des syndromes apparentés. Marseille: Solal.
- Michel S, Soppelsa R, Albaret JM (2011) L’Examen Geronto-Psychomoteur. Manuel d’application. Paris: Hogrefe.
- Morais A, Santos S, Lebre P (2016) Psychometric properties of the Portuguese version of the examen Géronto-Psychomoteur (P-EGP). Educational Gerontology 42: 516-527.
- Doumit J, Nasser R (2010) Quality of life and wellbeing of the elderly in Lebanese nursing homes. Int J Health Care Qual Assur 23: 72-93.
- Somme D, Trouvé H, Passadori Y, Corvez A, Jeandel C, et al. (2014) The French society of geriatrics and gerontology position paper on the concept of integration, Part One. Geriatr Psychol Neuropsychiatr Vieil 12: 5-12.
- Sibai A, Sen K, Baydoun M, Saxena P (2004) Population ageing in Lebanon: Current status, future prospects and implications for policy. Bull World Health Organ 82: 220-223.
- Simon NM, Smoller JW, McNamara KL, Maser RS, Zalta AK, et al. (2006) Telomere shortening and mood disorders: Preliminary support for a chronic stress model of accelerated ageing. Biol Psychiatry 60: 432-435.
- Central Intelligence Agency (2016) The World Factbook. Central Intelligence Agency Website.
- Tucker AM, Stern Y (2011) Cognitive reserve in aging. Curr Alzheimer Res 8: 354-360.
- Thelen E (1995) Motor development. A new synthesis. Am Psychol 50: 79-95.
Citation: Faddoul SG, Abizeid CM, Albaret JM (2017) Psychomotor Aging in Lebanon: Reliability and Validity of the Geriatric Psychomotor Examination. J Alzheimers Dis Parkinsonism 7: 372. DOI: 10.4172/2161-0460.1000372
Copyright: © 2017 Faddoul SG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4636
- [From(publication date): 0-2017 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 3810
- PDF downloads: 826