Short Communication Open Access
Psychoactive Medications as Independent Risk for Heat Injury in Emergency Medical Service Workers
Tony L. Brown1* and Emmett Larsen21Columbia University College of Physicians and Surgeons
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
The Upward Trend In Psychoactive Drug Prescriptions
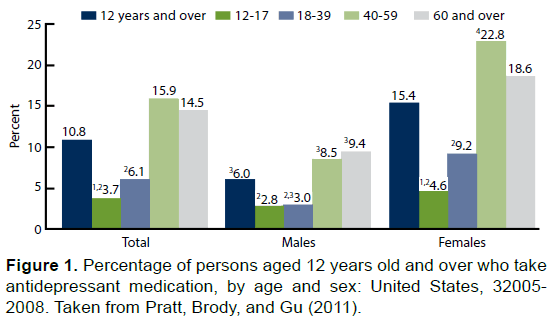
The dramatic increase in use of psychoactive medications in recent years has reached far and wide into many different spheres of American life. In the military, for example, a recent report on the prescribing of psychoactive medication noted that, “nearly 8 percent of active duty Army troops are on sedatives, and another 6 percent are on antidepressants, figures that are up eightfold since 2005” (Heyes, 2012). In civilian life, as well, this trend is even stronger; Figure 1, taken from Pratt, Brody, and Gu (2011), shows that nearly 11% of Americans aged 12 and over take antidepressants (a number, the authors note, which is up nearly 400% since the early 1990’s).
Effects of Psychoactive Drugs in Extreme Temperatures
Many side effects of psychoactive medications are still being discovered. Importantly, recent research has identified a causal relationship between psychoactive medication and heat injury as a result of certain unintended side effects. Page, Hajat, Kovats, and Howard (2012) found that antipsychotic medications were associated with a 7% increase in relative risk per 1°C increase in temperature. Similarly, Kudoh, Takase & Takazawa (2003) investigated temperature regulation during anesthesia and postoperative shivering in depression patients taking antidepressant drugs. Results indicated that intraoperative core hypothermia was difficult to accomplish in patients taking antidepressants. The group with increased incidence of shivering exhibited alterations in central thermoregulation attributable to antidepressant drug use resulting in serotonergic receptor down-regulation. These findings, taken together, support the notion that individuals taking certain psychoactive medications are at a substantially higher level of risk for heat injury when exposed to higher temperatures.
Drug Mechanisms of Action
This dangerous susceptibility becomes further evident when certain specific mechanisms of these medications are examined. Anti-depressants exert a plethora of physiological effects, including: affecting the hypothalamic-set temperature, impeding the function of thermoreceptors, impeding heat-production, impairing the efficacy of the cholinergic system (and thus sweat production), and impeding cutaneous vasodilatation.
Stollberger, Lutz, and Finsterer (2009) note that, specifically in SSRIs (Selective Serotonin Reuptake Inhibitors), another prominent side effect is the reduction of serum sodium and, in turn, the reduction of thirst. This could lead to accelerated dehydration during an extreme heat event.
Another class of antidepressants-tricyclics – causes subjects to experience disproportionate intolerance to heat increases, which Epstein, Albukrek, Kalmovitc, Moran, & Shapiro, (1997) postulate is to be due to their blocking effect on reuptake of norepinephrine and serotonin.
Fluoxetine (Prozac) exerts an effect of enhanced heat production and inhibited heat loss. Epstein et al. (1997) observes regarding this effect that since the release of serotonin in the anterior hypothalamus has been shown to stimulate cholinergic heat production pathways, inhibiting reuptake of serotonin will indeed increase heat production. Brown (2014) further note that enhanced serotonin activity inhibits dopamineric heat loss pathways in the medial anterior hypothalamic preoptic area.
Overall, these many effects amount to a substantial obstruction to the body’s ability to self-regulate in extreme temperature situations.
Risk to Emergency Workers
This collection of scientific findings bears significantly on the health risks of emergency workers, whose activities can very often be physically strenuous, causing heightened internal bodily temperatures. All this can also be easily exacerbated by extreme environmental temperatures, such as heavy protective equipment in summertime heat, proximity to fires, etc. Firefighters are, of course, a prime example of the at-risk population of emergency workers, in that their duties can include carrying patients out of fire areas, wearing heavy uniforms in hot conditions, etcetera. Indeed, a 2008 report by the University of Illinois Fire Service Institute noted that, “heat stress may be a common causal factor in both heart attacks and slips, trips and falls [in firefighters]” (Smith, Horn, Goldstein, & Petruzzello, 2008). However, the same risks hold true in the context of many other emergency workers (e.g. EMTs, paramedics, police, etc.) who may similarly wear heavy uniforms or be obliged to engage in comparably strenuous rescue-related activities.
Summary
The heat-related side effects of the psychoactive medications here discussed very urgently enjoin us to caution. Extreme heat situations pose a substantially heightened risk of injury to those taking antidepressants (and other medications), and emergency workers might be seen as an especially at-risk population due to the nature of their professional activities.
References
- Epstein, Y., Albukrek, D., Kalmovitc, B., Moran, D.S., & Shapiro. (1997). Heat intolerance induced by antidepressants. Annals of the New York Academy of Sciences, 813, 553-558
- Heyes, J. D. (2012). More than 110,000 U.S. soldiers remain on antidepressants and sedatives. Retrieved from: http://www.naturalnews.com/036001_soldiers_psychiatric_drugs_veterans.html#ixzz30IXGFpcp
- Kudoh, A., Takase, H., &Takazawa, T. (2003). Chronic treatment with antidepressants decreases intraoperative core hypothermia. Anesthesia & Analgesia, 97, 275-279.
- Page,L.A., Hajat, S., Kovats, S., & Howard, L.M. (2012). Temperature-related deaths in people with psychosis, dementia and substance misuse. The British Journal of Psychiatry, 200, 485-490
- Pratt, L.A., Brody, D.J., &Gu, Q. (2011). Antidepressant use in persons aged 12 and over: United States, 2005–2008. NCHS data brief, no 76. Hyattsville, MD: National Center for Health Statistics
- Smith, D.L., Horn, G., Goldstein, E., & Petruzzello, S.J. (2008). Fire fighter fatalities and injuries: the role of heat stress and PPE. Retrieved from: https://www.fsi.illinois.edu/documents/research/FFLSRC_FinalReport.pdf
- Stollberger, C., Lutz, W., & Finsterer, J. (2009). Heat-related side-effects of neurological and non-neurological medication may increase heatwave fatalities. European Journal of Neurology, 16, 879-882
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 19546
- [From(publication date):
specialissue-2015 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 14875
- PDF downloads : 4671