Provider Views on Screening for Postpartum Depression and Strategies to Increase Access to Maternal Mental Healthcare
Received: 04-Feb-2021 / Accepted Date: 19-Mar-2021 / Published Date: 27-Mar-2021 DOI: 10.4172/2471-9846.1000276
Abstract
Background: Perinatal Mood and Anxiety Disorders (PMADs), including postpartum depression (PPD) are the number one complication of childbirth, with prevalence rates of approximately 7-15% in the US; however, rates as high as 40-60% for women living in poverty have been reported. Though validated screening tools and effective treatment exists, it is largely unrecognized and untreated. Consequences impact not only the mother but her infant as well and can have long term deleterious effects. Multiple poor obstetric outcomes have been reported due to untreated PMAD’s including: low attendance at prenatal care, preterm labor, low birth weight, maternal suicide, decreased breastfeeding rate, impaired maternal/infant bonding, and short and long term behavioral and cognitive issues for the child including social and language delays, impulsivity, and poor academic performance. Due to the significant public health sequalae, Butte County, California First 5 has identified PMAD’s as a critical maternal health focus area.
Methods: Based on a community needs assessment and a literature review, educational sessions were developed to increase screening and treatment of PPD within a rural health center in Northern California. During the four educational sessions, 32 providers and staff received information on PPD, instructions on screening with the Edinburg Postnatal Depression Scale (EPDS), triage/treatment guidelines, lactation safety information on common psychiatric medications, and community resources for PPD. Outcomes were measured by pre- and post- session surveys and by deidentified chart and referral data.
Outcomes: Of the 16 providers who completed post-surveys, 81% stated the sessions changed their PPD screening or treatment practices, and 100% found the information helpful. These sessions also resulted in a 133% increase in referrals for postpartum mental health issues. Integrating treatment into a preexisting home visitation program reduced evaluation and treatment waiting times from three to four months to seven to ten days, with a 97% breastfeeding continuation rate for women receiving treatment.
Conclusion: Building interdisciplinary triage/treatment pathways and holding educational sessions for providers and staff within a rural health clinic with strong lactation support services resulted in an increase in screening for PPD by obstetric and family practice providers and a decrease in waiting time for evaluation and treatment of affected women without an interruption in breastfeeding.
Keywords: Postpartum depression; PMAD; PPD; Screening; Rural health clinic
Abbreviations
PMAD: Perinatal Mood And Anxiety Disorders; PPD: Postpartum Depression; MRT: Mosby’s Research Tool; CATSR: Critical Appraisal Tool for Systematic Reviews.
Background
Perinatal Mood and Anxiety Disorders (PMADs) including Postpartum Depression (PPD) are the number one complication of childbirth, with prevalence rates of approximately 10% in US, but much higher rates have been reported for women living in poverty [1]. Although validated screening tools exist, they are rarely used in outpatient obstetrical settings, and although effective treatment options are available, misinformation abounds, further complicating issues. Lack of provider awareness about PPD can increase the feelings of shame and stigma experienced by women suffering from difficult postpartum adjustments, and misinformation regarding the safety of antidepressant medications often leads to early weaning, further exacerbating the depression and interrupting the breastfeeding dyad which carries so many benefits for both mother and baby [2].
As mentioned before, untreated perinatal mood and anxiety disorders can have devastating consequences. Women who are depressed during pregnancy often have fewer prenatal care visits, can have inadequate or excessive weight gain, are at higher risk for preterm labor or birth, are at risk for substance use, and are less likely to initiate or sustain breastfeeding [3-5]. Documented consequences for infants of mothers with untreated depression include: impaired bonding, changes in infant brain development, infant developmental and language delays, and potential for neglect or abuse [2,6]. In the most serious cases, untreated depression can be deadly [7]. Tragically, suicide is the second leading cause of death during the perinatal period [8], and infanticide, though rare, is a reality as well. However, instances are almost always associated with postpartum psychosis, not with other PMAD’s [9].
The negative impact of PPD on mothers and infants is well established, and while prevention is ideal, the next best thing is early screening and treatment. Universal screening for PPD was advocated by World Health Organization in 2009; and the Patient Protection and Affordable Care Act of 2010 (Section 2952) provides support for screening with no share of cost [5,10]. While there is controversy regarding universal screening, the bulk of the literature and expert opinions support it [5,6,11-14]. However, many OB and pediatric providers are hesitant to screen for multiple reasons.
Methods
A literature review of PubMed and Cochrane Data Base was undertaken using the search terms “postpartum depression” OR “perinatal mood and anxiety disorders.” Filters activated included: clinical trial, randomized controlled trial, systematic reviews, metaanalysis, published in the last 5 years, humans, and English language, which resulted in 206 articles. An additional search phrase added -AND- “prevention” or “treatment” which narrowed the results to 155 articles. Another search phrase “AND interventions” was included which narrowed the results to 39 articles. Additional articles were obtained using the same search criteria from weekly PubMed search updates and mining the reference lists of reviewed articles. Quantitative and qualitative research articles were reviewed and graded using Mosby’s Research Tool (MRT), and systematic reviews were analyzed using the Critical Appraisal Tool for Systematic Reviews (CATSR). Of the reviewed articles, 48 were synthesized based on relevance to the project. Several other studies and organizational position statements are included for background information. The evidence suggested that the Edinburgh Postnatal Depression Scale (EPDS) is the preferred method of screening with a cut-off of 10 or greater as a positive screen for the presence of depressive symptoms (giving a 90% sensitivity rate) [10]. While the EPDS is not diagnostic, there is significant evidence that requiring a formal structured clinical interview can be a barrier for the initiation of treatment for many women [5,10,12,15]. The literature also pointed to the importance of integrating screening into primary care and pediatric practices where women are typically already interfacing for care [6,10,11,15].
Based on a review of literature and a community needs assessment, a quality improvement (QI) project focused on increasing the screening and treatment of PPD by perinatal practitioners within a rural health clinic was initiated. Because screening has been shown to increase referral and treatment [5,10,15,16], the focus of the project was to increase screening for PPD using the EPDS within a federally designated rural health center (RHC). Objectives of the project were to determine the impact of the educational intervention on obstetric and pediatric provider knowledge of PMAD’s, rates of screening and referral for PPD both pre and post-intervention, impact of triage/ treatment/referral pathways on accessibility of mental health services for postpartum women, and impact of provider knowledge regarding psychiatric medications and lactation on breastfeeding rates. Pre- and post-surveys were used in conjunction with educational interventions to increase knowledge and comfort of perinatal providers regarding screening and treatment of PPD in a rural health center. The goal was to determine current PPD screening practices, barriers to screening, and to increase screening and treatment/referral rates within the clinic, as well as increasing provider comfort and knowledge regarding treatment options and community resources.
Between 3/4/2014 and 4/2/2014, four educational sessions (approximately 30 minutes in duration) were conducted with interested perinatal staff at the rural health center regarding the importance of PPD screening. Voluntary participants completed an anonymous pre-intervention survey that included the IRB approved consent form. Participants received educational training regarding PPD screening using the EPDS, treatment guidelines from the Academy of Breastfeeding Medicine, information on lactation safety of common psychiatric medications, and community resources for women with PMAD’s. Each provider office was also given a copy of the book Hale’s Medications and Mother’s Milk. Additionally, the recommended PPD screening-triage guidelines were shared and discussed [17]. Providers were given both electronic and hard copies (tool kits) of the information and were encouraged to begin screening postpartum women at the 2 and/or 6 week postpartum visit or at pediatric well-baby appointments and referring women who need further evaluation and/or treatment to specially trained home visiting nurses.
In order to assess the impact of the educational session on provider knowledge, comfort and screening practices, the post-intervention survey was sent out through Survey Monkey three months after the educational sessions. All responses were anonymous and the information aggregated. Participation in the educational intervention and surveys was voluntary, and information obtained from survey data purposefully did not differentiate license type (RN versus MD versus advanced practice registered nurse i.e., certified nurses-midwife, NP) to avoid comparisons among disciplines. All efforts were taken to insure to confidentiality and anonymity of participants in order to gain honest feedback regarding barriers to PPD screening.
Specific outcomes measured included: number of perinatal providers attending educational intervention, pre- and postintervention knowledge and comfort regarding screening and treatment of PMAD’s, percentage of women screened between 2 and 6 weeks postpartum and at well-baby pediatric visits (from anonymous provider survey), as well as time from positive screen to initiation of treatment, and breastfeeding rates for woman receiving treatment for PPD (from de-identified aggregated reports compiled by clinic support staff).
Results
A total of 32 perinatal and family-practice providers and staff attended the sessions and received the screening-triage guidelines as well as the tool-kits for their offices. While initially, family practice providers were not targeted for the educational sessions, there was interest expressed by the primary care department who felt they were seeing a number of women coming in for depression or anxiety during the first year postpartum. Additionally, an educational session was conducted for approximately 30 labors and delivery RNs at the hospital affiliated with the clinic, and a presentation was given at the Butte County Perinatal Public Health Council with 12 attendees from various disciplines. All survey data collected were anonymous and aggregated to look at overall trends. Of the 32 attendees, 23 returned the pre-educational survey (72% response rate), and 16 returned the post-educational survey (50% response rate). Of the respondents, 35% identified their primary practice area as obstetrics/gynecology (n=6), 31% as family practice (n=5), 11% as behavioral health (n=2), 15% as pediatric (n=3) and 8% as “other” or unspecified (n=1). Of the 16 post-educational survey respondents, 81% (n=13) said the information in the educational session impacted their screening or treatment practices, and all attendees answered that they found the tool kit helpful to varying degrees (100%, n=16) (Figure 1). Open-ended question responses regarding how the sessions impacted their practices included, “More aware of local resources and screening tools,” “I have some resource tools to provide patients,” and “We are more unified as a Health Center in how we screen and treat PMAD’s.”
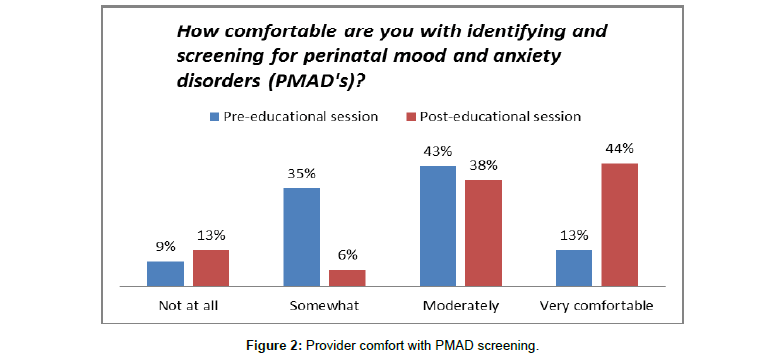
In terms of clinician comfort with identifying and screening for PPD, there was a significant shift towards being “moderately” or “very comfortable” versus “not at all” or “somewhat comfortable” in the post-education survey data (n=16) compared to the pre-education survey data (n=23) (Figure 2).
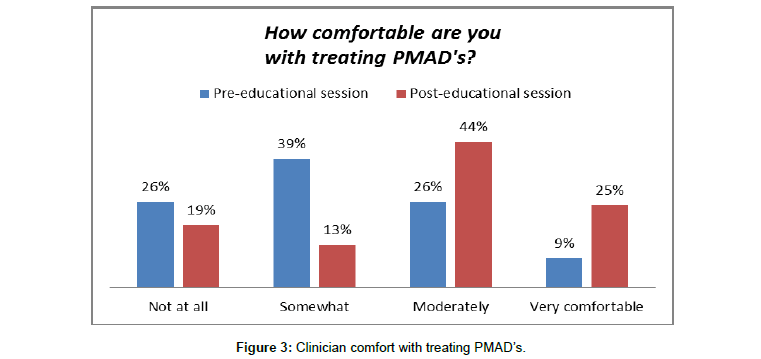
A positive trend was seen in comfort with treating PMAD’s in the post-educational survey data as well. Pre-education data revealed that only 35% reported feeling “moderately” or “very comfortable” treating PMAD’s versus 69% reporting such comfort in the post-educational surveys (Figure 3).
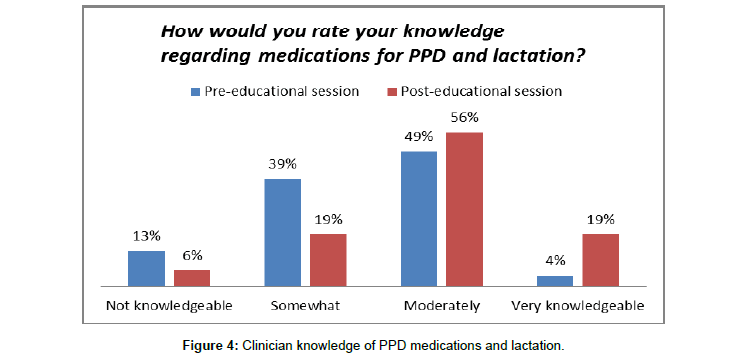
In terms of knowledge regarding lactation and medications for PPD, the post-educational session surveys also showed a positive shift from 42% rating their knowledge as “not knowledgeable” or “somewhat” on the pre-education survey (versus 22% on the posteducation survey) and 65% of respondents rating their comfort level as “moderately” or “very comfortable” post-education (versus 35% preeducation) (Figure 4).
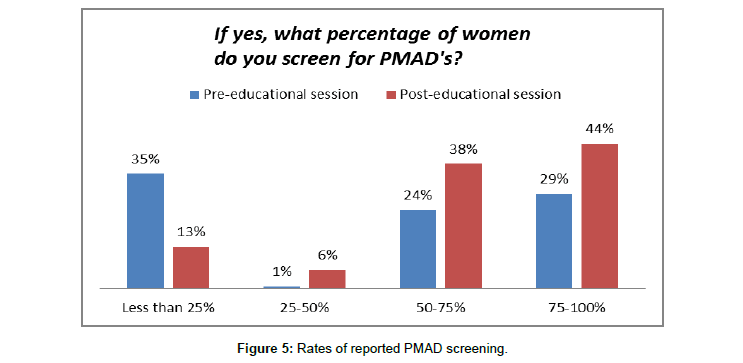
Prior to the educational sessions, providers were asked about PPD screening practices. Of the 23 respondents, 74% reported that they did screen women for PPD or other PMAD’s. Of those screening women, 35% (n=6) reported screening less than 25% of the time, none reported screening 25-50% of the time, 24% (n=4) reported screening 50-75% of the time, and 29% (n=5) reported screening 75-100% of the time (Figure 5).
The most common time for screening was at the 2 and/or 6 week postpartum appointment (76%, n=13) but other times were cited as well, including initial prenatal visit (41%, n=7), pediatric well-baby visits (24%, n=4), and “other” (18%, n=3). Respondents were allowed to choose multiple answers regarding timing of screening, so results do not equal 100%.
The most commonly used screening tool was the EPDS (65%, n=11), but other methods that were used included: “informal method” (47%, n=8), “specific formal questions developed by our office” (18%, n=2), PHQ-2 (6%, n=1), PHQ-9 (6%, n=1), and “other” (12%, n=2). No one reported using the Beck Inventory (Figure 6).
Following the educational sessions, there was no significant difference in the percentage of providers who reported screening (74% versus 76%), but there was a significant difference in the percentage of providers who reported screening 75-100% of the time (29% versus 44%).
Additionally, there appeared to be a formalization of screening, moving away from “informal method” and “specific formal questions developed by our office” (65% pre-educational session versus 29% post-educational session), towards an increased use of the EPDS (65% pre- educational session versus 79% post-educational session).
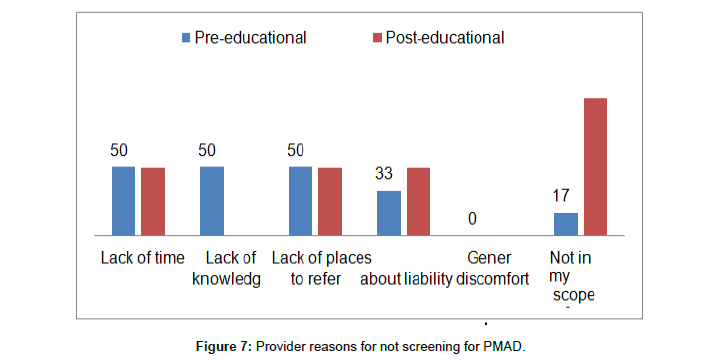
Reasons for not screening women for PPD were also examined in the surveys. In the pre- educational session survey, 26% of respondents (n=6) reported not screening women for PPD. Respondents were given multiple options for reasons and could choose as many as applicable. “Lack of time”, “lack of knowledge” and “lack of places to refer for treatment” were all cited by half of respondents (n=3). “Concerns about liability” were cited by two respondents, and one respondent answered “not seeing the patient as much”. None of the respondents cited “general discomfort” as a factor in their choice to not screen. Following the educational sessions, 24% of respondents reported not screening (n=5) which was a consistent proportion to the pre-education data. While “lack of time” and “lack of places to refer” remained the same in frequency of reasons cited for not screening, “concerns about liability” increased from 33% to 50%, and “not in my scope of practice” increased dramatically from 17% to 100% of providers who reported not screening women for PPD following the educational session. “General discomfort” was not cited as a reason in either group of survey data, and “lack of knowledge” decreased dramatically from 50% to zero in the post-educational session surveys (Figure 7).
Discussion and Recommendations
Increasing access to mental health care for postpartum women is important both for the suffering women and for their dependent infants. Developing triage and treatment/referral pathways and tool kits with resources for providers was welcomed and overwhelmingly seen as helpful. Provider feedback by anonymous survey showed an increase in knowledge and comfort with screening and treatment, thus one recommendation would be to continue to offer brief trainings and support services for interested perinatal providers. Enlisting pediatric and obstetric doctors as change agents may also be useful in engaging some harder to reach medical offices.
The resistance to screening seen within the pediatric discipline was disappointing but not surprising. Although clearly maternal depression negatively impacts the development of the infant in her care, the fact that the mother is not the patient of the pediatric office hinders the willingness and ability of pediatric providers to see screening for PPD as part of their scope of practice. This, coupled with an already stretched to capacity schedule and minimal, if any, reimbursement for screening and referral does not create an environment amenable to practice change adoption. Within the pediatric department, there was understanding regarding the importance of recognizing and treating PPD, and providers and office staff expressed a willingness to give paper copies of the EPDS to mothers bringing their infants in for well-baby visits, but the office staff and pediatric providers were uncomfortable scoring and counselling mothers regarding the results. It is recommended that continued stakeholder discussions with pediatric providers be conducted to better understand barriers to maternal PPD screening and develop workable solutions.
Another recommendation from this project is the importance of targeting not only obstetric and pediatric providers for education on PPD, but family practice providers as including these advance practice nurses who often see women during the first year postpartum for other health issues. Nationally, due to a lack of psychiatric specialists, primary care providers have had to take a lead role in diagnosing and treating many common mental health issues [15]. Because most primary care providers do not specialize in obstetrics or lactation, there may be discomfort or a lack of knowledge regarding best treatment approaches for PPD. Furthermore, since mental health issues can often present with somatic complaints [4], raising awareness and index of suspicion for PPD within primary care clinics increases the likelihood of identifying women in need of treatment and support. Education regarding lactation safety of psychiatric medications also enables primary care providers to provide women with appropriate treatment options which support breastfeeding continuation whenever possible.
Limitations
As with any quality improvement project, there are limitations in the design that may impact the interpretation and generalizability of the project findings. In order to accommodate the needs of providers in an evolving clinical environment, the project interventions adjusted over the course of implementation. Because providers self-selected to participate, there may be selection bias and lack of generalizability of interpretations of results, and the small sample size also limits generalizability of results. The survey instruments were reviewed by stakeholders and content experts, but they were not validated for reliability and only offer descriptive and trend data without risk adjustment or formal statistical analysis. Finally, the timeframes of the project limited the ability to collect data over an extended period. Nonetheless, it is hoped that this project will offer insight into barriers to screening and potential solutions to increasing access to perinatal mental health care for this population of childbearing women.
Conclusion
Building interdisciplinary triage/treatment pathways and holding educational sessions for providers and staff within a Federally Qualified Rural Health Clinic (FQRHC) resulted in an increase in screening for postpartum depression (PPD) by obstetric and family practice providers. During the four educational sessions, 32 providers and staff received information on PPD and instructions on screening with the EPDS, as well as triage and treatment guidelines. Of the 16 who completed post-surveys, 81% stated the sessions changed their PPD screening or treatment practices, and 100% found the information helpful. These sessions also resulted in a 133% increase in referrals for postpartum mental health issues. Integrating front-line treatment into a preexisting home visitation program reduced evaluation and treatment waiting times from three to four months to seven to ten days, and a 97% breastfeeding continuation rate for women receiving treatment. Based on qualitative and quantitative survey data, project intervention overall increased provider awareness and comfort with screening for and treating PPD as well as lactation safety of psychiatric medications and available community resources for affected women. However, in order to sustain and expand screening locally and nationally, legislative and organizational policy issues need to be addressed. Increasing billing incentives for providers to screen for PPD, integrating screening into billing requirements for insurance or into Centers for Medicare and Medicaid (CMS) core measures, and standardizing electronic health records (EHR’s) to prompt providers to screen for PPD are just some examples of ways to increase screening and treatment of PPD on a systems level.
Postpartum depression is a serious but treatable disease. Women suffering with PPD deserve competent and compassionate care, and their infants deserve to have their mothers functioning at their optimal level. Developing community triage and referral networks, increasing provider awareness and screening is crucial for early recognition and treatment. Mothers and babies in our communities are depending on us.
References
- Bauman BL, Ko JY, Cox S (2020) Vital Signs: Postpartum Depressive Symptoms and Provider Discussions About Perinatal Depression-United States, 2018. MMWR Morbitity & Mortal Weekly Report 69:575-581.
- Wisner KL, Sit DK, Hanusa BH, Moses-Kolko EL, Bogen DL, et al. (2009) Major depression and antidepressant treatment: Impact on pregnancy and neonatal outcomes. Am J Psychiatry 166(5):557-566.
- Dennis CL, Hodnett ED (2007) Psychosocial and psychological interventions for treating postpartum depression. Cochrane Database Syst Rev 17(4):CD006116.
- Misri S, Kendrick K (2007) Treatment of perinatal mood and anxiety disorders: A review. Can J Psychiatry 52(8): 489-498.
- Santoro K, Peabody H (2010)  Identifying and treating maternal depression: Strategies and considerations. National Institute for Health Care Management.
- Earls MF (2010) Clinical report-Incorporating recognition and management of perinatal and postpartum depression into pediatric practice. Pediatrics 126(5): 1032-1039.
- Dennis CL, Hodnett E, Reisman HM, Kenton L, Weston J, et al. (2008) Effects of peer support on prevention of postnatal depression among high risk women: Multisite randomized controlled trial. BMJ 338:a3064.
- Lindahl V, Pearson JL, Colpe L (2005) Prevalence of suicidality during pregnancy and the postpartum. Arch Womens Ment Health 8(2):77-87.
- Horowitz JA, Murphy CA, Gregory KE, Wojcik J (2011) A community-based screening initiative to identify mothers at risk for postpartum depression. J Obstet Gynecol Neonatal Nurs 40(1):52-61
- American College of Nurse-Midwifery. (2002). Depression in women: Position statement. Division of Women’s Health Policy and Leadership.
- Gaynes BN, Gavin N, Meltzer-Brody S, Lohr KN, Swinson T (2005) Perinatal depression: Prevalence, screening, accuracy, and screening outcomes. Agency for Healthcare Research and Quality, AHRQ Pub 5:E006.
- Myers ER, Aubuchon-Endsley N, Bastian LA, Gierisch JM, Kemper AR, et al. (2013). Efficacy and safety of screening for postpartum depression. Comparative Effectiveness Reviews 106. AHRQ Publication 13-EHC064-EF. Rockville, MD: Agency for Healthcare Research and Quality.
- Sharma V, Burt VK, Ritchie HL (2010) Assessment and treatment of bipolar II postpartum depression: A review. J Affect Disord 125:18-26.
- Yawn BP, Olson AL, Bertram S, Pace W, Wollan P, et al. (2012) Postpartum depression: Screening, diagnosis, and management programs 2000 through 2010. Depress Res Treat 2012:363964.
- Hale TW (2012) Medications and Mother’s Milk 2012. Amarillo, TX: Hale Publishing.
Citation: Kralj H (2021) Provider Views on Screening for Postpartum Depression and Strategies to Increase Access to Maternal Mental Healthcare. J Comm Pub Health Nursing 6: 276. DOI: 10.4172/2471-9846.1000276
Copyright: © 2021 Kralj H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2237
- [From(publication date): 0-2021 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 1645
- PDF downloads: 592