Research Article Open Access
Protocol for: The Use of Intra-Gastric Balloons as an Adjunct to a Lifestyle Support Programme to Promote Weight Loss in Severely Obese Adolescents
Reece LJ1*, Copeland RJ1, Sachdev P2, Thomson M3, Wales JK2 and Wright NP21Sheffield Hallam University, HWB, Collegiate Hall, Centre for Sport and Exercise Science, Sheffield Hallam University, Sheffield, S10 2BP, UK
2Endocrinology Department, Sheffield Children’s Hospital, UK
3Gastroenterology Department, Sheffield Children’s Hospital, UK
- *Corresponding Author:
- Reece LJ
Sheffield Hallam University
HWB, Collegiate Hall
Centre for Sport and Exercise Science
Sheffield Hallam University, Sheffield
S10 2BP, UK
Tel: +441142254355
E-mail: l.reece@shu.ac.uk
Received Date: October 21, 2013; Accepted Date: November 11, 2014; Published Date: November 14, 2014
Citation: Reece LJ, Copeland RJ, Sachdev P, Thomson M, Wales JK et al. (2014) Protocol for: The Use of Intra-Gastric Balloons as an Adjunct to a Lifestyle Support Programme to Promote Weight Loss in Severely Obese Adolescents. J Child Adolesc Behav 2:173 doi:10.4172/2375-4494.1000173
Copyright: © 2014 Reece LJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Background: Severe childhood and adolescent obesity (BMI>3.5SD) remains a significant public health priority with an increasing incidence and is associated with significant morbidity including immediate and long-term cardiovascular, metabolic and psychological consequences. Current non-invasive treatments including lifestyle modification and pharmaceutical intervention are of limited effectiveness in this population, which leaves permanent bariatric surgery as the only viable option. As an alternative, intra-gastric balloons offer a reversible, potentially safer and less invasive option for severely obese adolescents for whom all other available treatments have been exhausted. Methods/design: BOB is a non-randomised pilot study. A cohort of 12 obese adolescents (BMI > 3.5SD, puberty stage 4 or more) aged 13 - 16 years, will be recruited to the study, where an intragastric balloon (ORBERA – inflated to 500-700ml) will be inserted into the stomach for 6 months, whilst receiving intense, weekly, behavioural support for the family. Follow-up will continue for 18 months after balloon removal with reduced behavioural support. The primary outcome measure will be the change in body weight and BMI standard deviation score from baseline following six months with the intragastric balloon and lifestyle therapy. Secondary outcome measures include the assessment of weight maintenance at 18 months post balloon removal, biomedical outcomes including blood glucose levels, physical activity and physical fitness, and psychosocial outcomes such as paediatric health-related quality of life.
Keywords
Childhood; Weight; Lifestyle; Pharmaceutical
Abbreviations
BOB - Balloons in obesity; LR - Lindsey Reece (lead author); RC - Robert Copeland; NW - Neil Wright; PS – Pooja Sachdev; LDA – Lizzy De Angelis; BMI - Body Mass Index; WHO - World Health organisation; NICE - National Institute for Clinical Excellence; BIB - Bioenterics fluid filled balloons; Peds QL - Paediatric quality of life; TPB -Theory of planned behaviour; HOMA - Homeostasis model assessment; HR PQCT - High resolution peripheral quantitative computed tomography; HDL - High density lipoprotein; LDL - Low density lipoprotein; GLP-1 - Glucagon-like peptide-1GIP - Gastric inhibitory polypeptide; DXA - Dual-energy X-ray absorptiometry; CYPSPP - Child and Youth Self-perception profile; OGTT - Oral glucose tolerance test; U&E -Urea and Electrolytes; LFT’s - Liver function test; PAQ - Physical activity questionnaire for adolescents
Background
The prevalence of overweight and obesity in children and adolescents continues to rise, presenting a major challenge for health-care providers. Globally, the number of overweight and obese individuals increased from 857 million in 1980, to 2.1 billion in 2013 [1]. Prevalence has increased substantially in children and adolescents in developed countries, with 23.8% (22·9–24.7) of boys and 22.6% (21.7–23.6) of girls overweight or obese in 2013 [1]. In developing countries, obesity also increased from 8.1% (7.7–8.6) to 12.9% (12.3– 13.5) in 2013 for boys, and from 8.4% (8.1–8.8) to 13.4% (13.0–13.9) in girls [1,2]. Here in the United Kingdom, UK, obesity rose amongst 2-10 years old to 13% in 2010-2012, with 18.7% of older children aged 11-15year obese and 35% overweight and obese [3]. Consequences of severe obesity at an early age include; orthopaedic complications, type 2 diabetes, increased risk of cardiovascular disease and hypertension [4]. Worryingly, the majority of these medical concerns have traditionally only presented in adults [2,4] and as Reilly and Kelly (2011) reviewed, a large body of evidence now confirms obesity in childhood and adolescence can lead to premature mortality and physical morbidity in later life [2]. The psychopathology of obesity in young people is a concern with overweight and obese children experiencing poor quality of life, lower self-esteem [5,6] and an enhanced risk of being socially isolated than their healthy weight counterparts [7]. Several variables are associated with low Quality of life, QOL, such as self-image, bullying, bodily pain, quality of food intake, physical activity, screen time, parents, and weight status [6]. Being obese in childhood is also associated with depressive symptoms and thoughts of suicide, often linked to bullying in schools and/or through the use of social media networks [8,9]. Taken collectively these data confirm the dire need to intervene with efficient and cost-effective treatment programmes for young people who are severely obese.
The National Institute for Health and Clinical Excellence (NICE) presents treatment guidelines for overweight and obese children and young people, emphasizing the importance of lifestyle interventions focusing on diet control, physical activity and behavioural change all being delivered within a multi-disciplinary framework [10,11]. Yet, for many adolescents whose Body Mass Index (BMI) place them in the severely obese bracket (i.e. BMI >99th percentile), lifestyle interventions are ineffective with only modest short-term efficacy in terms of weight-related outcomes [2]. Perhaps due to the added complexity of being severely obese, treatment programmes for this population often report high attrition rates, usually failing to ensure significant and sustained weight loss longer-term [12]. As adults (equivalent BMI >40, or >35 with co-morbidities), these individuals would be considered for bariatric surgery [10], which is associated with long-term successful weight loss [13]. In response to rising obesity prevalence, there is a growing body of research exploring the use of bariatric surgery in young people. A review of bariatric procedures [13], including the adjustable gastric band, sleeve gastrectomey, roux-en-Y gastric bypass and biliopancreatic diversions, in obese children and adolescents indicate significant decreases in BMI one year post-surgery with some evidence of co-morbidity resolution and improvements in health-related quality of life [13,14] reported results from a prospective study of 81 adolescents undergoing laparoscopic Roux-en-Y gastric bypass and showed a 32% reduction in BMI after 2 years [15]. Despite growing evidence from the research community, for the use of bariatric surgery as a safe and effective treatment option for severely obese adolescents [13,15], inconsistencies with protocol reporting, lack of detail on surgical complications [16] and limited reports of the long-term effectiveness [13], results in some practitioners and policy-makers hesitant to recommend surgery as a treatment [17-19]. This reluctance to perform bariatric surgery more frequently in adolescents is reinforced by, current UK clinical guidelines that specify adolescent bariatric surgery should only be considered in exceptional individual circumstances [9]. Yet there is strong recognition that novel, less invasive, whilst equally effective treatment strategies tailored to the needs of severely obese adolescents [20,21] are warranted. One such approach, which is proposed here, is the use of intra gastric balloons as a potential, reversible, intervention for adolescent obesity.
Intragastric balloons were first proposed as an aid for weight loss more than 20 years ago [22]. Since then, Bioenterics fluid-filled balloons (BIB) have been sited endoscopically into the stomach typically for six months, to induce satiety by reducing the stomach capacity, thereby reducing food intake and encouraging weight loss amongst obese populations [23,24]. A systematic review by Dumonceau (2008) of BIB treatments reported a mean weight loss of 17.8 kg, ranging from 4.9 kg – 28.5 kg [21]. Imaz (2008) reported a weight loss of 14.7 kg at 6 months representing a 32.1% loss of excess weight and a BMI change of 5.7 [22]. Building on the learning from weight management literature, treatment with BIB should be proposed in the setting of a multidisciplinary framework [22] to help promote and sustain the lifestyle changes adopted [10]. Studies assessing lifestyle modification, quality of life and psychosocial impact are limited, with little data on long-term follow-up post balloon removal [22]. In addition to weight loss, psychopathologic outcomes must be assessed as participation in supervised exercise therapy interventions have been shown to improve measures of self-esteem and increased physical activity among obese children [25-28].
This pilot study proposes the use of intragastric balloons, alongside a lifestyle support programme, to help severely obese adolescents to lose weight. The study is entitled Balloons in Obesity given the acronym BOB.
Methods / Design
Study aims
The primary aim of BOB is to assess the feasibility of using an intrasgastric balloon, alongside a lifestyle support programme, to promote weight loss in severely obese adolescents at six months. Weight maintenance will be assessed 18 months post-balloon removal.
Study design and setting
BOB is a non-randomised pilot study. This involves 12 obese adolescents (BMI > 3.5SD, puberty stage 4 or more) aged 13 - 16 years, recruited to the study, where an intragastric balloon (ORBERA – inflated to 500-700ml) will be placed in-situ endoscopically under general anaesthesia at a specialised children’s hospital, for 6 months, whilst receiving intense behavioural, lifestyle support for the family. Follow-up will continue for 18 months after balloon removal with reduced behavioural support. This study incorporates medical evaluation and monitoring led by a paediatrician alongside receiving nutritional advice, physical activity counselling and behavioural support, delivered by a Research Fellow at an English university, aimed to optimise the likelihood of patients achieving desired outcomes.
Participant eligibility
Participants will be recruited according to the following inclusion criteria: (1) Clinically Obese and aged 13 - 16 years old (BMI > 3.5 SD); (2) have attained or nearly attained adult stature and stage 4 pubertal development; (3) Have previously attempted weight loss through a structured management programme (4) Are able to attend weekly sessions with researchers and are capable of adhering to the lifestyle changes advised. Exclusion criteria are as follows: (1) previous oesophageal or gastric surgery or history of intestinal obstruction; (2) history of inflammatory disease of the gastrointestinal tract such as oesophagitis, gastric or duodenal ulcers or congenital anomalies such as atresias or stenosis; (3) Hiatus hernia >5 cm (assessed at balloon insertion); (4) History of, or current significant psychological disorder (permission sought from lead care giver).
Ethical considerations
Significant public and patient involvement was sought during project development. Full ethical approval for this study has been obtained from the NHS Sheffield research ethics committee. Written informed consent will be required from all participants and their parents prior to commencing the study.
Study interventions
An intragastric balloon (ORBERA TM– inflated to 500-700ml) will be placed in-situ endoscopically under general anaesthesia. The balloon will remain in place for 6 months with monthly assessments by the research paediatrician and gastroenterologist to ensure correct balloon placement and provide routine medical check. To reinforce lifestyle changes, families will attend weekly sessions lasting for up to an hour, at a time that suits the family, with the research fellow at the university facility. Upon request, up to 6 sessions could be held in families’ local community to encourage sustained lifestyle change. In line with NICE (2011) guidance and previously reported evidencebased obesity intervention [25,28], the multi component intervention will include behaviour change strategies to increase families’ physical activity, improve eating behaviour, and provide social support as well as supervised exercise sessions. Sessions will be client-centred and tailored to the needs of the young person and their family. Follow-up sessions with the research paediatrician and research fellow will take place up to 18 months after balloon removal.
Intervention schedule
The BOB programme will be delivered, in total, over two years by a multi-disciplinary team (Paediatrician’s (NW & PS); Dietician (LDA); Chartered Psychologist (RC); Research Fellow (LR); Research Nurses. The medical component of the study is overseen by Consultant Paediatrician NW, delivered by Paediatrician PS, with the behaviouralprogramme overseen by Chartered Psychologist (RC) and delivered by Research Fellow (LR) specialising in delivering behaviour change programmes with obese populations. Once recruited, families begin with a four week preparatory phase prior to balloon insertion, then undergo six month intensive lifestyle support, and a two month relapse prevention phase post-balloon removal. Follow-ups with both the paediatrician and research fellow take place at 6, 12 and 18 months post-balloon removal.
Preparatory phase (0-4 weeks)
Once recruited, all families commence the study by undergoing weekly sessions for four weeks, aimed to ensure families are certain of their decision to participate, are fully aware of the implications of their decision, understand what is involved and are committed to the project. This time frame provides the opportunity for the research team to assess patient suitability, conduct the baseline assessments and continue to build rapport.
Early weeks of BOB (4-8 weeks)
This first month living with the balloon provides opportunity to build rapport between the research team, the adolescents and their families. The focus of the behaviouralprogramme is to explore participant expectations from the study,with individual success criteria and discussion of goals all informing tailored support and an agreed action plan for the delivery of the programme. From a medical perspective, the focus is on participant safety ensuring balloon placement is correct and offering weekly medical check-ups with associated appropriate tests.
Living with BOB (9–20 weeks) and Post BOB (20-28 weeks)
The remaining 5 months with the balloon inserted, and for 2 months after balloon removal, participants will follow a weekly lifestyle support programme delivered by the research fellow (LR). Individual sessions will last approximately 1 hour and include a mix of physical activity, support for behaviour change and nutrition advice (e.g. understanding food labels, portion control and healthful eating). The lifestyle programme will be underpinned by recognised models of health-related behaviour change [26,27] and adhere to previously efficacious approaches with overweight and obese young people [29,30]. To achieve a person-centred approach, sessions will be delivered in accordance within the spirit of Motivational Interviewing, MI [28]. Furthermore, the lifestyle programme will utilise a variety of commonly applied behaviour change techniques [30,31] to enhance physical activity and diet-related behaviour. Due to the lack of detail and consistent reporting of behaviour change techniques utilised in physical activity and health behaviour change programmes, Abraham and Mitchie developed the taxonomy of behaviour change techniques, to standardise and hopefully resolve this issue [29,30]. To standardise the techniques utilised in this study, table 1.0, attempts to map techniques with definitions and techniques provided by Abraham and Mitchie, with the addition of examples highlighting where they will be delivered throughout BOB.
| Label | Definition | Sessions | Example from BOB |
|---|---|---|---|
| Provide information on consequences of behaviour in general | Information about the relationship between the behaviour and its possible or likely consequences in the general case, usually based on epidemiological data, and not personalised for the individual | Familiarisation, Weeks 1-4 |
The researcher will initiate discussions regarding the impact of obesity on general health and wellbeing. |
| Provide information on consequences of behaviourto the individual | Information about the benefits and costs of action or inaction to the individual or tailored to a relevant group-based on that individual's characteristics (i.e. demographics, clinical, behavioural or psychological information). | Familiarisation, Weeks 1-4 |
The researcher will initiate discussions regarding the impact of obesity on the young peoples and their families' personal context. This will include the benefits of losing weight to them personally, E.g. - more able to attend college and participate in activities like other students. |
| Provide information about others’ approval | Involves information about what other people think about the target person's behaviour. It clarifies whether others will like, approve or disapprove of what the person is doing or will do. | Familiarisation, Weeks 1-4 |
Discuss with the participant how the opinions of family and friends might or might not change, as a result of making changes to their lifestyle as part of the BOB research study. |
| Provide normative information about others’ behaviour | Involves providing information about what other people are doing i.e. indicates that a particular behaviour or sequence of behaviours is common or uncommon amongst the population or amongst a specified group | Familiarisation, Weeks 1-2 |
Researcherwill explain that other young people and families are experiencing similar consequences as a result of their weight, and making lifestyle changes is also something others find difficult. |
| Goal setting (behaviour) | The person is encouraged to make a behavioural resolution (e.g. take more exercise next week). This is directed towards encouraging people to decide to change or maintain change. | Weeks 6 - 24 | Researchers ask the young people to identify a specific behaviour that they plan to make changes to. E.g. walking home from school on 2 days a week. The SMART principle to goal setting will be applied here (Locke, 2000). |
| Goal setting (outcome) | The person is encouraged to set a general goal that can be achieved by behavioural means but is not defined in terms of behaviour (e.g. to reduce blood pressure or lose/maintain weight), as opposed to a goal based on changing behaviour as such. | weeks 5, 6 | The researcher will explore with the young people general outcomes that they would like to achieve at the end of the project. Thought will be given to what they want to look like, how they feel about this and if they consider it realistic. i.e. - weight losses, fit in specific dress size, and wear a certain outfit. |
| Action planning | Involves detailed planning of what the person will do including, as a minimum, when, in which situation and/or where to act. ‘When’ may describe frequency (such as how many times a day/week or duration (e.g. for how long). | weeks 4-24 | The researcher will develop with the young person action plans to implement new behaviours. This will follow the 'if then' principle (Gollwitzer, 1999) and SMART goal setting. i.e. - if I am having a sad day - will telephone a friend. |
| Barrier identification/problem solving | This presumes having formed an initial plan to change behaviour. The person is prompted to think about potential barriers and identify the ways of overcoming these barriers. | Weeks 12 - 24, follow ups 6mth, 12mths, 18mths post balloon. | Young people will be supported to consider how life events, daily activities, emotions, might affect their ability to perform their chosen goal. The researcher will elicit a list of potential barriers form the young person whilst exploring potential strategies to overcome these. |
| Set graded tasks | Breaking down the target behaviour into smaller easier to achieve tasks and enabling the person to build on small successes to achieve target behaviour. This may include increments towards target behaviour or incremental increases from baseline behaviour. | On-going from week 9-24 | The researcher will explore with the young people their expectations from engaging in the BOB study. From this, the researcher can work with the families to break down into small achievable goals, applying the SMART principle (Locke, 2000) that will build over time to achieve their desired outcome. |
| Prompt review of behavioural goals | Involves a review or analysis of the extent to which previously set behavioural goals (e.g. take more exercise next week) were achieved. | On-going weeks 9 - 24 | The researcher will spend the start of each weekly session with the young person, discussing the progress made in relation to the young person's chosen behaviours. Achievement or failure of the goal will be explored with the participant adapting the goal in preparation for the following week. |
| Prompt review of outcome goals | Involves a review or analysis of the extent to which previously set outcome goals (e.g. to reduce blood pressure or lose/maintain weight) were achieved. | Weeks 1, 4, 4-8, 12, 16, 20, 24. 6mths, 12mths and 18mths post | Participant weight will be measured and recorded regularly along with waist and hip measurements. This result will then be discussed with the participant to gage an understanding of satisfaction with progress and to support the participant with future goal setting. |
| Prompt rewards contingent on effort or progress towards behaviour | Involves the person using praise or rewards for attempts at achieving a behavioural goal. | On-going weeks 9 - 24 | The researcher will continuously provide praise and positive affirmations when participants successfully attempt and achieve behavioural goals they have set. The family are also encouraged to provide praise throughout to support the young person's progress. Self-reward is encouraged during the weekly sessions. |
| Provide rewards contingent on successful behaviour | Reinforcing successful performance of the specific target behaviour. This can include praise and encouragement as well as material rewards but the reward/incentive must be explicitly linked to the achievement of the specific target behaviour i.e. the person receives the reward if they perform the specified behaviour but not if they do not perform the behaviour. | week 25 | The researcher will praise and offer positive affirmations for lifestyles changes the young person and their families achieve. A free pass to a local gym will be offered as a reward for completing the physical activity sessions during BOB, acting as an incentive to maintain the physical activity. |
| Shaping | Contingent rewards are first provided for any approximation to the target behaviour e.g. for any increase in physical activity. Then, later, only a more demanding performance, e.g. brisk walking for 10 min on 3 days a week would be rewarded. Thus, this is graded use of contingent rewards over time. | weeks 9 -24 | Any attempts made by the young people and their families' to be more physically active will be reinforced positively by the researcher. Throughout the programme praise will be given when this intensity of behaviour is increased. For example, during early gym sessions families will be praised when completing 2 minutes on the treadmill at 1% incline at a steady pace. Towards the latter stages, this praise would be given when completing 20 minutes a 2% at gradient at a brisk pace. A free pass to a local gym will also be offered at the end of the project for successful completion. |
| Prompting generalisation of a target behaviour | Once behaviour is performed in a particular situation, the person is encouraged or helped to try the behaviour in another situation. The idea is to ensure that the behaviour is not tied to one situation but becomes a more integrated part of the person's life that can be performed at a variety of different times and in a variety of contexts. | weeks 9-16 | The researcher will elicit from the young person situations where they are finding it difficult to adopt their desired behaviour yet have been successful at other times, e.g. eating lunch at school. Potential strategies to overcome this will then be explored. |
| Prompt self-monitoring of behaviour | The person is asked to keep a record of specified behaviour(s) as a method for changing behaviour. This should be an explicitly stated intervention component, as opposed to occurring as part of completing measures for research purposes. This could e.g. take the form of a diary or completing a questionnaire about their behaviour, in terms of type, frequency, duration and/or intensity. | Weeks 9 -24 | The researcher will share self-monitoring techniques, such as a food diary or exercise diary, with the young person/families. The researcher will then ask the young person to explore the drawbacks and benefits of their use to support them in achieving their desired outcomes. |
| Prompt self-monitoring of behavioural outcome | The person is asked to keep a record of specified measures expected to be influenced by the behaviour change, e.g. blood pressure, blood glucose, weight loss, physical fitness. | Week 4 – 8, 9 – 12, 16 – 20, 20-24, | The researcher will encourage the young people to monitor their desired outcomes, e.g. weight loss, through the use of pre and post photographs and clothes size. |
| Prompting focus on past success | Involves instructing the person to think about or list previous successes in performing the behaviour (or parts of it). | Weeks 1-4, 4-8 | Young people are asked to consider what has helped them achieve their desired outcomes in the past, and how this could inform helpful strategies within BOB. |
| Provide feedback on performance | This involves providing the participant with data about their own recorded behaviour | Weeks 4 - 8, 12, 16, 20, 24. 6mths, 12mths and 18mths post | The researcher will give the results of tests to the young person/family and elicit feedback on results from the participant. |
| Provide information on where and when to perform the behaviour | Involves telling the person about when and where they might be able to perform the behaviour | Week 20 - 24 | Families are given information about local facilities to be active, encouraging them to move more outside of their BOB sessions. |
| Provide instruction on how to perform the behaviour | Involves telling the person how to perform behaviour or preparatory behaviours, either verbally or in written form. | Weeks 9 -20 | The researcher will offer advice on suitable clothes to wear for the supervised physical activity sessions and essentials to bring. The researcher instructs how to use the gym equipment safely as well as how to perform body weight exercises safely. |
| Model/Demonstrate the behaviour | Involves showing the person how to perform a behaviour | Weeks 9 - 20 | The researcher will provide demonstrations on how to use the gym equipment and perform certain physical movements effectively allowing the participant to observe and ask questions if needed, before attempting to perform the movement themselves. |
| Teach to use prompts/cues | The person is taught to identify environmental prompts which can be used to remind them to perform the behaviour (or to perform an alternative, incompatible behaviour in the case of behaviours to be reduced). | weeks 16-24 | The researchers will facilitate a discussion asking the young person /family to consider their environment and identify strategies to help remind them to perform their desired behaviour. E.g. set an alert on their mobile phone to ensure the young person eats regularly throughout the day. |
| Environmental restructuring | The person is prompted to alter the environment in ways so that it is more supportive of the target behaviour e.g. altering cues or rein forcers. | Weeks16 - 24 | Families are encouraged to consider their home environment and identify ways this could be altered to support them to achieve a healthier lifestyle. E.g. Consideration given to availability of a table for the families to dine together. |
| Agree behavioural contract | Must involve written agreement on the performance of an explicitly specified behaviour so that there is a written record of the person's resolution witnessed by another. | Weeks 4,5 | A psychological contract is drawn up between the researcher and the young person, witnessed by the family, outlining key principles all will commit to throughout the study. |
| Prompt practice | Prompt the person to rehearse and repeat the behaviour or preparatory behaviours numerous times. Note this will also include parts of the behaviour e.g. refusal skills in relation to unhealthy snacks. | Young people will beasked to consider situations that they experience temptation to deviate from their desired behaviour or a situation where they find persisting with a given outcome difficult. The young person will elicit strategies to overcome this which the researcher encourages them to practice regularly. E.g. distraction strategies such as phoning a friend, if they feel bored and are tempted to eat when they do not need to. | |
| Use of follow-up prompts | Intervention components are gradually reduced in intensity, duration and frequency over time, e.g. letters or telephone calls instead of face to face and/or provided at longer time intervals. | Week 24, 6mths, 12mths, 18mths post balloon removal. | Weekly face to face sessions with the researcher will be reduced, with contact via telephone one month post-balloon removal. Face to face sessions will then only occur at follow-up appointments. |
| Facilitate social comparison | Involves explicitly drawing attention to others’ performance to elicit comparisons. | On-going weeks 9 -24 weeks | Researchers will draw on examples from other BOB families to encourage the individual to consider their progress not just individually, but also in comparison to other young people undergoing the same project. |
| Plan social support/social change | Involves prompting the person to plan how to elicit social support from other people to help him/her achieve their target behaviour/outcome. This will include support during interventions e.g. setting up a ‘buddy’ system or other forms of support and following the intervention including support provided by the individuals delivering the intervention, partner, friends and family. | weeks 4 - 8 | The researcher will encourage the young person to consider the support network around them, including family, friends, BOB research team, and what role they might play in supporting them in achieving their desired outcomes. |
| Prompt identification as role model/position advocate | Involves focusing on how the person may be an example to others and affect their behaviour,E.g being a good example to children. Also includes providing opportunities for participants to persuade others of the importance of adopting/changing the behaviour, for example, giving a talk or running a peer-led session. | weeks 9- 24 | The young people/ families will be encouraged to talk about their experience of undergoing lifestyle changes to other BOB families. The young people will also be supported to offer peer support to their siblings/friends who could also require support in leading a healthier lifestyle. |
| Prompt anticipated regret | Involves inducing expectations of future regret about the performance or non-performance of behaviour. This includes focusing on how the person will feel in the future and specifically whether they will feel regret or feel sorry that they did or did not take a different course of action. | week 1-4, week | The short time frame of the BOB project (6months) will be outlined explicitly to all the young people/families. As a result, they will be encouraged to consider how they can optimise this time to support them in the short term as well as the longer term. Throughout the project, the researcher will continuously encourage the individuals/families to consider how lifestyle changes made whilst on the project will be sustained over the longer-term after BOB. |
| Fear arousal | Involves presentation of risk and/or mortality information relevant to the behaviour as emotive images designed to evoke a fearful response | weeks 1 -4 | The risk associated with the insertion and removal procedure of the intragastric balloon will be discussed, along with anaesthetic and mortality risk. |
| Prompt self-talk | Encourage the person to use talk to themselves (aloud or silently) before and during planned behaviours to encourage, support and maintain action. | The young people will be asked to think about challenging situations they could face day to day, and then they will be asked to develop motivational phrases which they can say to themselves to support them with carrying out their desired behaviour. | |
| Prompt use of imagery | Teach the person to imagine successfully performing the behaviour or to imagine finding it easy to perform the behaviour, including component or easy versions of the behaviour. | weeks 4-8 | When discussing expectations of the BOB project, young people will be asked to visualise how they would like to look, clothes they would like to wear, and how they would like to feel at the end of the project. |
| Relapse prevention/coping planning | This relates to planning how to maintain behaviour that has been changed. The person is prompted to identify in advance, situations in which the changed behaviour may not be maintained and develop strategies to avoid or manage those situations. | weeks 20-24, 6mths, 12mths, 18mths | Young people will be asked to consider which changes they have made during this study that they think they will struggle to continue with. Strategies will be then be developed to support these behaviours. |
| Stress management/emotional control training | This is a set of specific techniques (e.g. progressive relaxation) which do not target the behaviour directly but seek to reduce anxiety and stress to facilitate the performance of the behaviour. It might also include techniques designed to reduce negative emotions or control mood or feelings that may interfere with performance of the behaviour, and/or to increase positive emotions that might help with the performance of the behaviour. | weeks 9-24 | The researcher will ask the young person to reflect on an experience where they have felt emotional and behaved in a way they did not want to. E.g. getting angry at mealtimes with the family. The researcher will then teach the individual to take deep breaths to calm themselves down, allowing them time to think before they respond. |
| Motivational interviewing | This is a clinical method including a specific set of techniques involving prompting the person to engage in change talk in order to minimise resistance and resolve ambivalence to change (includes motivational counselling). | On-going throughout | The researcher draws on principles of Motivational Interviewing to deliver the intervention such as expressing empathy and being directive in conversations with the young people. |
| Time management | This includes any technique designed to teach a person how to manage their time in order to make time for the behaviour. These techniques are not directed towards performance of target behaviour but rather seek to facilitate it by freeing up times when it could be performed. | week 9 - 12 | Young people will be asked to outline their typical week detailing firm commitments, social commitments and anything else. This will facilitate a discussion that explores opportunities in the week to be physically active. |
| General communication skills training | This includes any technique directed at general communication skills but not directed towards a particular behaviour change. | week 12-16 | The researcher will discuss with the young person ways to express themselves better through communication. E.g - educating young people on being assertive and able to say 'No'when they don't want a big portion of food at mealtimes. |
| Stimulate anticipation of future rewards | Create anticipation of future rewards without necessarily reinforcing behaviour throughout the active period of the intervention. Code this technique when participants are told at the onset that they will be rewarded based on behavioural achievement. | The researcher will continually use praise and positive affirmation as a reward for achievement of a desired goal by the BOB individual/family. Free gym passes will be available for those families who successfully engage and complete the project. |
Table 1: Mapping of behaviour change definitions and techniques to the BOB protocol
During sessions participants and their families and friends will also be offered a range of aerobic exercise modalities including gymbased equipment (e.g. treadmills and bikes), outdoor activities such as walking, as well as the use of exercise DVD’s. The exercise sessions will be delivered in small bouts of no more than 10-minutes to build self-efficacy and will be of moderate intensity, in line with Public Health England recommendations [31-33]. Sessions will also include mini-games and self-referenced competitions to help motivate and build self-worth. These approaches have been shown to help build global self-worth and promote adherence to the intervention [25]. During the sessions the rating of perceived exertion will be measured using the pictorial children’s effort rating table (PCERT) [32]. Participants will be asked to point to how they feel the exertion compares against a 10 point scale. Medical assessments take place once a month with PS at the children’s hospital. 4.9 Dietetic Input All participants and families will receive two, one-hour sessions with a specialist dietician (LDA). One session before the balloon is inserted to support participants from a full fluid diet through to the re-introduction of solid foods, and once after the balloon is removed to reinforce the maintenance of reduced calories and portion size and commitment to a healthy balanced diet. Under specialist circumstances participants can access dietetic support throughout the programme; however key healthy eating messages will underpin the weekly delivery of the lifestyle support programme as previously mentioned.
Outcome measures
The primary outcome measure is the change in body weight and BMI standard deviation score from baseline following six months intragastric balloon therapy and lifestyle programme. Secondary outcome measures include the assessment weight maintenance at 18 months post balloon removal, biomedical outcomes including blood glucose levels, and psychosocial outcomes such as paediatric healthrelated quality of life.
Biomedical outcomes
Biomedical outcomes comparing change in biomedical data at the various time points (baseline, following six months intragastric balloon therapy and subsequently at 18 months post balloon removal) include:
• Difference in fasting glucose, fasting insulin glucose ratio and HOMA
• Difference in total cholesterol, HDL, LDL, triglycerides and atherogenic index.
• Difference in systolic and diastolic blood pressure standard deviation scores.
• Change in liver function tests
• Changes in Ghrelin, GLP-1 and GIP levels
• Changes in adipokines, osteokines, bone formation and turnover markers
Changes in total fat mass, bone mineral content and bone density as assessed by DXA and changes in bone architecture as assessed by highresolution peripheral quantitative computed tomography, HR pQCT.
Psychosocial Outcomes
Paediatricquality of life
The PedsQL Measurement Model is a modular approach to measuring health-related quality of life (HRQOL) in children and adolescents including 1) Physical Functioning (8 items), 2) Emotional Functioning (5 items), 3) Social Functioning (5 items), and 4) School Functioning (5 items). The PedsQL consists of brief, practical, generic core scales suitable for use with healthy school and community populations, as well as with paediatric populations with acute and chronic health conditions [34]. In a study looking at health- related Quality of Life, overweight and obese adolescents reported significantly lower scores compared to their healthy counterparts [35].
Physical self-perceptions
Self-perception is to be measured on the subscale from the Children and Youth Physical Self-perception Profile (CY-PSPP) developed in 1989 and adapted for use in children in 1995 [36]. The CY-PSPP contains 6 subscales; Sport/Athletic, Attractive Body Adequacy, Condition, and Strength competence as well as Physical and Global Self-Worth. The Children and Youth Physical Self-Perception Profile (CY-PSPP) assesses the degree to which young people view themselves as competent in a variety of physical domains [37,38]. Each question contains two statements relating to either a positive perception of competence or a negative perception of competence. The respondent is required to choose which statement best describes the way they view themselves and answer either ‘sort of true for me’ or ‘really true for me’ for each statement. Questions are structured in an alternative format on a scale between 1 (low score) and 4 (high score). Affect [39].
Participants are asked to indicate the degree, using a scale of 1 (very slightly) to 5 (extremely), each adjective describes how they have felt the previous week. Positive items include proud, satisfied, happy, excited and relaxed and the negative effect includes unhappy, nervous, guilty and angry. Assessment of planned behaviour The Theory of Planned Behaviour (TPB) was developed to predict behaviours in which individuals have incomplete volitional control [27]. In light of the fact that the lifestyle intervention study holds a focus on improving physical self-competence and self-efficacy towards exercise and given that perception of behavioural control as indicated by TPB can reflect past experiences, anticipation of upcoming circumstances, and the attitudes of the influential norms that surround the individual, components from the TPB will be assessed [39]. Participants will be asked to indicate by circling a number between one (strongly agree) and 7 (strongly disagree) to what extent they agree with statements such as; “I would like to participate in physical activity at least three times per week”, “If I wanted to, I could easily take part in regular physical exercise” or “Most people who are important to me, think I should take part in regular physical exercise”.
Physical fitness
Physical fitness will be measured using the modified Balke protocol [40]. The modified Balke protocol requires participants to walk at a pace of 1.34 m s-1 at a grade of 6% for 2 minutes. At the end of the two-minute stage, the grade is increased by 2%. This continues until volitional exhaustion. On the occasions that the treadmill reaches maximal elevation the participant continues to walk at that gradient until volitional exhaustion. The speed of the treadmill remains constant at 1.34 m s-1 for the duration of the protocol. The protocol ends at volitional exhaustion with time to exhaustion recorded. The test is continuous with no rest periods between each stage. Heart-rate (HR) will be measured during the last minute of each stage using a shortrange radio-telemetry monitor.
Physical activity level
The Physical Activity Questionnaire for Adolescents [40] will collect specific information about participation in various physical activities during the previous week. Specifically, participants are questioned about their engagement in (1) physical activities in their spare time; (2) physical education (3) lunchtime physical activities (4) extracurricular activities, (5) evening physical activities and (6) weekend activities. Each physical activity is scored on a scale between 1 (not engaged) to 5 (involved 5-7 times per week).
Assessment of outcomes
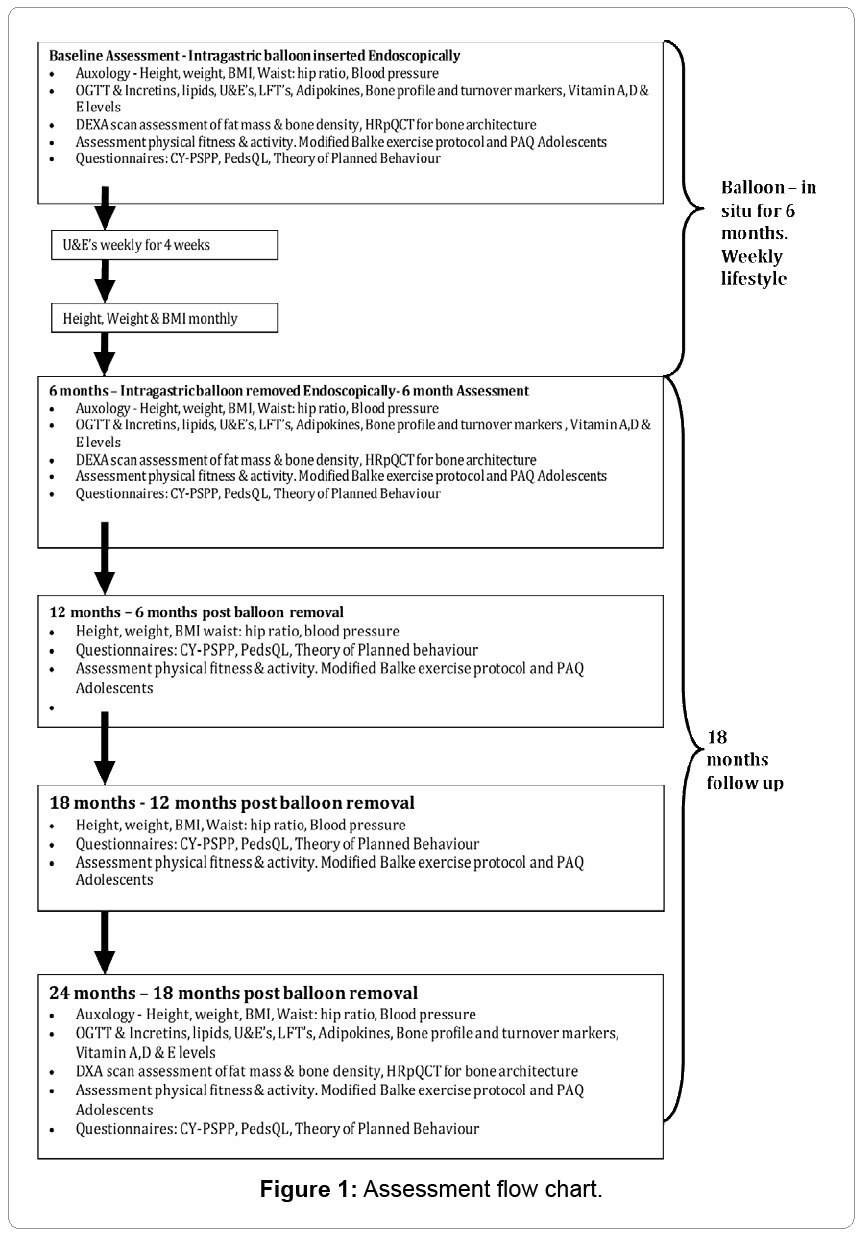
All outcomes will be measured at baseline, within 2 weeks of balloon insertion, and within 2 weeks of balloon removal after 6 months, then a further 6, 12 and 18 months post balloon removal (5 times). Figure 1 provides an overview of this.
Sample size
Sample size was selected as the optimal size for a pilot study balancing the requirements of obtaining data on potential outcomes with the number of individuals receiving a treatment, with those not shown to be effective, based upon Julious [41].
Statistical analysis
The primary outcome will be the patient’s BMI SDS at sixmonths. As this is a pilot study, with an insufficient sample size to power statistical significance, the mean and standard deviations will be reported. Secondary outcomes include, but are not an exhaustive list, further change in BMI after balloon removal; changes in Blood Pressure, Lipid profile, GLP-1 and GIP levels, bone density and fat mass, adipokines, osteokines, bone turnover markers and Quality of Life scores, with means and standard deviations plotted over time. Analysis of the OGTT results will be performed using a generalised least square (GLS) random-effects model. Longitudinal analysis and multilevel modelling of changes in BMI and biomedical markers will be undertaken to account for changes over time in relation to treatment and other co-variates such as age at baseline and sex.
Time Plan
Recruitment began in November 2011, with all balloon insertions and removals completed by February 2014. Follow-up data will be completed by December 2015.
Author’s contributions
Neil Wright, Jerry Wales and Robert Copeland were responsible for identifying the research question and securing the funding for the research. Lindsey Reece and PoojaSachdev contributed to the development of the protocol as members of the research team. All authors were responsible for the drafting of this paper and read and approved the final version.
Acknowledgements
This paper presents independent research as part of the Obesity Theme within the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care for South Yorkshire (NIHR CLAHRC SY). The views and opinions expressed are those of the authors, and not necessarily those of the NHS, the NIHR or the Department of Health.
CLAHRC SY would also like to acknowledge the participation and resources of our partner organisations. Further details can be found at www.clahrc-sy.nihr. ac.uk. An additional thank you to LizzyDeAngelis for providing the dietetic expertise in this study.
References
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384: 766-781.
- Foresight (2007). Tackling obesities: future choices (2nd Edn.,) Government office for science.
- Public Health England (2014) Child weight data factsheet.
- Kelly AS, Barlow SE, Rao G, Inge TH, Hayman LL, et al. (2013) Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation 128: 1689-1712.
- Reilly JJ, Kelly J (2011) Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 35: 891-898.
- Buttitta M, Iliescu C, Rousseau A, Guerrien A (2014) Quality of life in overweight and obese children and adolescents: a literature review. Qual Life Res 23: 1117-1139.
- Schwimmer JB, Burwinkle TM, Varni JW (2003) Health-related quality of life of severely obese children and adolescents. JAMA 289: 1813-1819.
- THOMAS, Hannah J, CONNOR, Jason P, SCOTT, et al. (2014) Integrating traditional bullying and cyberbullying: Challenges of definition and measurement in Adolescents–a review. Educational psychology review 1-18.
- National Institute for Health and Clinical Excellence (2013): Managing overweight and obesity in children and young people: lifestyle weight management services.
- Pfeil M (2011) Weight loss surgery for morbidly obese adolescents: a review. J Child Health Care 15: 287-298.
- Sjöström L (2013) Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med 273: 219-234.
- Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev 8: CD003641.
- Black JA, White B, Viner RM, Simmons RK (2013) Bariatric surgery for obese children and adolescents: a systematic review and meta-analysis. Obes Rev 14: 634-644.
- Olbers T, Gronowitz E, Werling M, Mårlid S, Flodmark CE, et al. (2012) Two-year outcome of laparoscopic Roux-en-Y gastric bypass in adolescents with severe obesity: results from a Swedish Nationwide Study (AMOS). Int J Obes (Lond) 36: 1388-1395.
- Colquitt JL, Picot J, Loveman E, Clegg AJ (2009): Surgery for obesity. Cochrane Database of Systematic Reviews.
- Iqbal CW, Kumar S, Iqbal AD, Ishitani MB (2009) Perspectives on pediatric bariatric surgery: identifying barriers to referral. SurgObesRelat Dis 5: 88-93.
- Livingston EH (2010) The incidence of bariatric surgery has plateaued in the U.S. Am J Surg 200: 378-385.
- Zitsman JL, Inge TH2, Reichard KW3, Browne AF4, Harmon CM5, et al. (2014) Pediatric and adolescent obesity: management, options for surgery, and outcomes. J PediatrSurg 49: 491-494.
- Woolford SJ, Clark SJ, Sallinen BJ, Geiger JD, Freed GL (2012) Bariatric surgery decision making challenges: the stability of teens' decisions and the treatment failure paradox. PediatrSurgInt 28: 455-460.
- Hofsteenge GH, Chinapaw M, Delemarre-van Waal H, Weijs P (2014): Long term effect of the Go4it group treatment for obese adolescents: A randomised controlled trial. Clinical Nutrition 33: 385-391.
- Dumonceau JM (2008) Evidence-based review of the Bioentericsintragastric balloon for weight loss. ObesSurg 18: 1611-1617.
- Imaz I, Martínez-Cervell C, García-Alvarez EE, Sendra-Gutiérrez JM, González-Enríquez J (2008) Safety and effectiveness of the intragastric balloon for obesity. A meta-analysis. ObesSurg 18: 841-846.
- Sallet JA, Marchesini JB, Paiva DS, Komoto K, Pizani CE, et al. (2004) Brazilian multicenter study of the intragastric balloon. ObesSurg 14: 991-998.
- Daley AJ, Copeland RJ, Wright NP, Roalfe A, Wales JK (2006) Exercise therapy as a treatment for psychopathologic conditions in obese and morbidly obese adolescents: a randomized, controlled trial. Pediatrics 118: 2126-2134.
- Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: Towards an integrative model of change. J of Consul and Clin Psychol. 51:390-395.
- Ajzen I (1991) The Theory of Planned Behaviour. Organizational behaviour and human decision processes50: 179-211.
- Daley AJ, Copeland RJ, Wright NP, Wales JK (2005) Protocol for: Sheffield Obesity Trial (SHOT): a randomised controlled trial of exercise therapy and mental health outcomes in obese adolescents [ISRCNT83888112]. BMC Public Health 5: 113.
- Miller WR, Rollnick S (1991) Motivational interviewing: preparing people to change addictive behaviour. New York: Guilford Press.
- Abraham C, Michie S (2008) A taxonomy of behaviour change techniques used in interventions. Health Psychology 3: 379-387.
- Michie S, Ashford S, Sniehotta FF, Dombrowski SU, Bishop A, et al. (2011) A refined taxonomy of behaviour change techniques to help people change their physical activity and healthy eating behaviours: the CALO-RE taxonomy. Psychol Health 26: 1479-1498.
- Public Health England (2014) Everybody Active, Everyday: Evidence based approach to Physical Activity.
- Yelling M, Lamb K, Swaine I (2002) Validity of a pictorial perceived exertion scale for effort estimation and effort production during stepping exercise in adolescent children. European physical activity review8: 157-175.
- Varni JW, Seid M, Kurtin PS (2001) PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care 39: 800-812.
- Keating CL, Moodie ML, Swinburn BA (2011) The health-related quality of life of overweight and obese adolescents--a study measuring body mass index and adolescent-reported perceptions. Int J PediatrObes 6: 434-441.
- Whitehead JR (1995) A study of children's physical self-perceptions using an adapted self-perception profile questionnaire. Paediatric Exercise Science 7: 132-151.
- Raustorp A, Ståhle A, Gudasic H, Kinnunen A, Mattsson E (2005) Physical activity and self-perception in school children assessed with the Children and Youth--Physical Self-Perception Profile. Scand J Med Sci Sports 15: 126-134.
- Ebbeck V, Weiss M (1998) Determinants of children's self-esteem: an examination of perceived competence and affect in sport. Paediatric Exercise science 10: 285-298.
- Hagger MS, Chatzisarantis NL (2009) Integrating the theory of planned behaviour and self-determination theory in health behaviour: a meta-analysis. Br J Health Psychol 14: 275-302.
- Rowland TW (1993) Aerobic exercise testing protocols. In Paediatric laboratory testing edited by: Rowland TW, Champaign, IL Human Kinetics 19-41.
- Kowalski K, Crocker N, Kowalski NP (1997) Convergent validity of the Physical Activity Questionnaire for Adolescents. Paediatric Exercise Science 4: 342-352.
- Julious S (2005) Sample size of 12 per group rule of thumb for a pilot study. Pharmaceutical statistics 4:287-291.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 16686
- [From(publication date):
December-2014 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 11977
- PDF downloads : 4709