Case Report Open Access
Proprioceptive Neuromuscular Facilitation Approach for Functioning Muscle Transfer: A Case Report
Yuan-Hung Chao1* and Yueh-Hsia Chen2
1School and Graduate Institute of Physical Therapy, College of Medicine, National Taiwan University, Taiwan
2Rehabilitation Center, Department of Plastic and Reconstructive Surgery, Chang Gung Memorial Hospital, Taoyuan County, Taiwan
- *Corresponding Author:
- Yuan-Hung Chao
Ph.D, PT, Assistant Professor, School and Graduate Institute of Physical Therapy
College of Medicine, National Taiwan University, Rm. 324, 3F, No. 17, Xuzhou Rd.
Zhongzheng Dist, Taipei City 10055, Taiwan
Tel: +886-2-3366-8129
Fax: +886-2-3366-8161
E-mail: yuanhungchao@ntu.edu.tw
Received date: May 10, 2016; Accepted date: May 20, 2016; Published date: May 31, 2016
Citation: Chao YH, Chen YH (2016) Proprioceptive Neuromuscular Facilitation Approach for Functioning Muscle Transfer: A Case Report. J Nov Physiother 6:294. doi:10.4172/2165-7025.1000294
Copyright: © 2016 Chao YH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Background: This case report of a patient with a an avulsion brachial plexus injury demonstrates the effectiveness of proprioceptive neuromuscular facilitation (PNF) integrated into hand therapy following a pedicled latissimus dorsi (LD) musculocutaneous flap transfer for elbow and fingers extension.
Methods: A 29-year-old right-hand dominant male suffered from high-energy crushing and avulsion injury at the workplace. He presented with pain (5/10), numbness over right upper limb, shoulder strength weakness (2/5), and brachial plexus injury including median, radial and ulnar nerve palsies. A pedicled LD musculocutaneous flap was performed to reconstruct the elbow and hand function simultaneously in the primary stage. The treatment program was divided into three phases: (1) immobilization phase (within 4 weeks after surgery), (2) facilitation phase (4 to 8 weeks after surgery), (3) strengthening phase (8 weeks after surgery). Application of PNF principles (manual contact, visual input and verbal instructions) and techniques (rhythmic initiation, repeated stretch, combination of isotonics and irradiation with D1 extension) were guided in the facilitation phase and early stage of strengthening phase to facilitate active control of elbow and finger extension.
Results: The patient could actively move the elbow and finger extensors after 2-weeks of PNF therapy. Up to 4 months after reconstructive surgery, the patient's elbow and fingers extensor reached strength of M4 and M3. In the next months, several palliative surgeries (e.g. elbow joint arthroplasty, thumb and wrist extension reconstruction) were performed. The patient returned to his original job as a manufactory worker 2 years after the accident.
Conclusion: PNF may be an effective and specific component of rehabilitation in the recovery of function in the early phase post injury for a patient with a major upper arm traction avulsion amputation reconstructed by a pedicled latissimus dorsi muscle.
Keywords
Proprioceptive neuromuscular facilitation; Functioning muscle transfer; Hand therapy
Background and Purpose
The function of the elbow joint is to provide stability and mobility in upper limb function [1]. With the advance of microsurgery, replantation after major limb amputation not only can allow patients to achieve a high survival rate, but also can restore successful upper limb function [2]. The reconstructive options for upper arm traction avulsion amputation are controversial [3,4]. It depends on the level of injury, status of the limb and the health status of the patient as well as the microsurgical techniques, the resources of the institution, the motivation of the patient and access to rehabilitation services.
Common options for elbow reconstruction consist of free functioning muscle transplantations [4-6] and a regional pedicled latissimus dorsi (LD) musculocutaneous flap transfer [1,7]. Rehabilitation is considered to be critical to achieve successful outcomes in these cases [8,9]. Rehabilitation requires activating the transferred muscles and learning new motor control strategies. Clinical trials and physiological studies have shown that cerebral cortical plasticity exists after free muscle transfer [10-12]. Apart from a tenodesis effect, Henseler et al. [13] and Plath et al. [14] also demonstrated with electromyography that the latissimus dorsi had viable muscle activity after tendon transfer for rotator cuff tears. Neural stimulation and motor reeducation seems to be essential to a successful rehabilitation program after muscle transfer. However, the above literature stresses the effectiveness of rehabilitation beyond the specificity of muscle reeducation post muscle transfer. No research literature could be located that specifically delineates how to retrain the transferred free or regional muscle flap particularly in terms of the formation and establishment of new neural pathways.
The role of therapists is to reeducate and facilitate each patient to acquire control of the new function of the transferred tendon or muscle. Sherrington defined the concepts of neuromuscular facilitation and inhibition in 1900s. Kabat developed the clinical proprioceptive neuromuscular facilitation (PNF) techniques in the 1940s. Knott and Voss further developed the PNF treatment approach to stimulate various neurological pathways. This technique places specific demands on the patient's neuromusculoskeletal system to facilitate natural functional movements.
Today, PNF is widely used to recover neuromuscular control by stimulation of muscle and joint proprioceptors as well as sensory inputs from peripheral organs to influence motor outputs of the central nervous system clinically. Originally PNF was applied to facilitate motor performance in patients post stroke [15-17]. Of late, PNF stretching techniques are extensively investigated and used to enhance joint ROM and muscle performance [18,19]. PNF induces muscle relaxation and elongation to relieve pain (e.g. low back pain, myofascial pain or knee pain) [20-22]. In addition, it is also extensively applied in the field of sports medicine [23,24]. However, despite the extensive research in wide, clinical applications, neurophysiological mechanisms involved in transforming sensory inputs from the periphery to cortical motor outputs at the spinal level and supraspinal level are still unknown.
A thorough literature review yields minimal information regarding the application of PNF for restoring muscle function post muscle transfer. Specific elements in PNF such as the principles of resistance, irradiation, traction, manual contact, stretch, and approximation in combination with specific PNF techniques, such as rhythmic initiation, combination of isotonics, reversal of antagonists, repeated stretch, contract-relax, hold-relax, and replications aim to initiate motion or to promote the learning of movement motor reeducation. Thus, the purpose of this case report is to demonstrate how PNF was used to develop an interventional approach for restoring the function of muscle transfers following a major upper arm traction avulsion injury of the brachial plexus. Although the underlying mechanisms are still unknown, we integrate these principles and techniques into training the transferred muscle to activate muscle performance and improve muscle strength. Our hypothesis was that PNF could improve voluntary motor performance and muscle strength post muscle transfer following a brachial plexus injury.
Background and description of the patient
The patient was a 29 year-old right hand dominant male who suffered from an industrial injury with 4th-degree burn at right arm and a compartment syndrome. He was admitted to a medical center. His lateral arm had major muscle and skin necrosis, and a laceration wound was found on his medial elbow with ulnar nerve exposure. Immediately post injury, fasciotomy and debridement were performed by a plastic hand surgeon.
This patient was a healthy young laborer, machine operator with generally good health. He lived with his wife and a four year-old child. His wife was also employed. No smoking, drinking or chronic disease was reported. Before this accident, he was reported to have a normal level of physical activity. Together, this couple raised their child independently before this accident. Since they were faced with a financial challenge after this accident, the patient desired to return to his pre-injury living status and had a strong motivation to return to work. The patient signed a consent form to be included in this case report of his experience.
Hand therapy examination
Mobility and functional status were assessed by a hand therapist 4 days after admission to the hospital. His right arm had a major wound with huge skin defect and severe swelling. The right arm wound was wet dressed. Pain was reported as a score of five out of ten. His fingers were cold. Numbness and loss of sensation was reported over his right upper limb. Right shoulder M2 muscle strength (Medical Research Council scale system) was documented. The elbow, wrist and fingers had no active motion (M0). The examination supported a right brachial plexus injury with median, radial and ulnar nerves palsy. Passive elbow range of motion (PROM) could not be performed due to the fragility of the wound and nerve exposure. Otherwise his wrist and fingers ROM was within normal limit. This patient was transferred by wheelchair to the rehabilitation center and appeared distressed. Most of his activities of daily living were partially independent, and required some assistance from his wife.
According to his status of injury, multiple stages of reconstructive surgeries were required. Prior to surgical intervention, rehabilitation consultation was obtained on maintaining joint and soft tissue flexibility. Education on improvement of his general performance in functional activities was provided prior to surgery. This included education and consultation about positioning, treatment goals, and therapy timeline. Avoidance of caffeine and nicotine was also provided as well.
During the period of hospitalization, this patient came to rehabilitation center every midweek day. The treatment programs prior to reconstructive surgery consisted of pain management, edema control, active or passive ROM exercise for hand, wrist, shoulder, and functional training for whole body reconditioning with transfer, ambulation, and self-care techniques.
After 3 weeks post-surgery, shoulder elevation reached about 90 degrees. Although elbow, wrist and hand active motion were still limited, he could walk to the rehabilitation center from his ward and he was participating in self-care in dressing, eating, and toileting. During this period, wound debridements had been performed for 3 times.
Reconstructive surgery
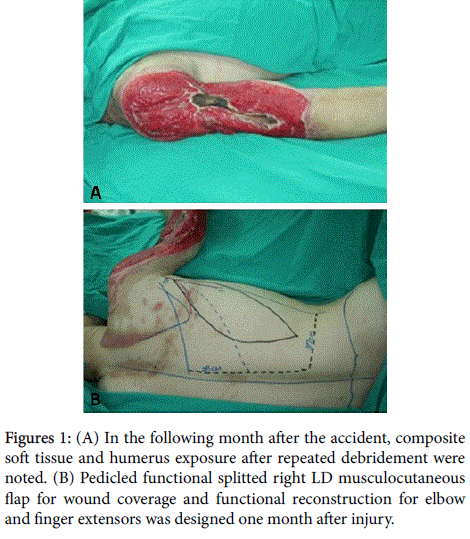
High-energy crushing and avulsion injury resulted in major soft tissue necrosis. Repeated debridements were accomplished 4 times in the month following the accident. Composite deltoid, triceps and soft tissue were debrided. Humeral bone was exposed with obvious median, ulnar, and radial nerve injuries (Figure 1A). One month after injury, a right pedicled latissimus dorsi (LD) musculocutaneous flap for wound coverage and functional reconstruction was performed (Figure 1B). The right vertical portion of LD musculocutaneous flap with skin paddle for excursion concern was transferred for finger extension, and transverse portion was fixed for elbow extension.
Figure 1: (A) In the following month after the accident, composite soft tissue and humerus exposure after repeated debridement were noted. (B) Pedicled functional splitted right LD musculocutaneous flap for wound coverage and functional reconstruction for elbow and finger extensors was designed one month after injury.
Interventions
Following LD musculocutaneous flap, the treatment programs were divided into three phases: (1) immobilization phase (within 4 weeks after surgery), (2) facilitation phase (4 to 8 weeks post-surgery), (3) strengthening phase (8 weeks post-surgery). The patient was intensively treated over 18 months.
Immobilization phase: In the immobilization phase, the orthosis was fabricated to protect the transferred LD musculocutaneous flap in a resting tension posture. After discussion with the hand surgeon, the orthosis was designed to place the elbow in full extension, wrist in 40° extension with metacarpophalangeal joints (MCPJ) and inter-phalangeal joints (IPJ) in full extension, and thumb abduction and extension. Considering LD muscle transfer for two-joint function, the orthosis was worn all day long for 4 weeks.
During the immobilization phase, interventions consisted edema control, soft tissue flexibility enhancement, shoulder joint range of motion (ROM) restoration, and functional training. At the initial 2 weeks, instructions to elevate right upper limb above heart level to prevent stress on the pedicle and to improve venous and lymphatic return were instructed. Gentle soft tissue mobilization on right hand was performed to prevent edema-induced stiffness. Furthermore, Coban® wrap around each finger from distal part to hand base was applied. Gradual right shoulder joint range of motion in pain-free range was implemented for 10 repetitions every section. This patient was instructed to perform massage, shoulder ROM exercise hourly at home during waking hours. In the following 3 weeks after flap reconstruction, a split thickness skin graft (STSG) was consecutively performed twice for residual skin coverage on his right arm and elbow. The patient was instructed to rest in bed and was successfully discharged from hospital after the skin graft. During this phase, pain was reported as a score of 3/10. No AROM was observed during this phase since this is in the immobilization phase.
Facilitation phase: The facilitation phase started at the 5th week after the LD musculocutaneous flap transfer. The patient attended the rehabilitation center for one on one therapy 3 times per week. The patient returned to the hospital with the orthosis for 6 weeks. He could elevate his shoulder around the shoulder level, but still demonstrated weakness in the brachial plexus distribution. Although he could not actively control his elbow, wrist and fingers, at this phase, the transfer was not innervated yet. Thus, conventional therapy in the first two weeks was initiated, and the orthosis was removed hourly for exercise. Scar massage on the transferred LD musculocutaneous flap and skin graft were employed 10 minutes prior to other treatment programs. Soft tissue massage and shoulder joint ROM exercise as described in the immobilization phase was implemented as well. Isolated shoulder, wrist and fingers were mobilized passively to prevent muscle, ligament or joint contracture since the range of each joint depended on the tension of the surrounding tissues. Electrical stimulation for radial, median and ulnar nerves denervated muscles in addition to the transferred functioning muscles was implemented to maintain muscle contractile properties [25,26]. A direct galvanic current was applied via probe surface electrodes on the estimated motor points of radial, median and ulnar nerves denervated muscles in addition to the transferred functioning muscles, and the intensity was adjusted for individual muscles to generate 20 visual muscle contractions on each site.
During the facilitation phase, PNF techniques were also implemented to facilitate active elbow and finger extension. PNF for 30 minutes was integrated into the conventional program. First, rhythmic initiation was directed to facilitate motion of elbow extension. The motion was initiated in the sequence of passive elbow flexion and extension (isolating in the pivoting movement of ulnar-humerus only) with verbal instruction to guide the patient through the desired movement for 10 repetitions. At the same time, the therapist determined the end range of elbow flexion not to over stress the tension of the transfer. In addition, a partial pattern isolating shoulder rather than full PNF pattern was performed to maintain the tension of transferred LD musculocutaneous flap. The therapist instructed the patient to present the previous action of LD muscle, and resistance was given on the dorsal side of upper arm against medial rotation and extension to facilitate LD muscle contraction. As the patient intended to contract his LD muscle, the therapist reminded him to observe a synchronized contraction of the transferred muscle flap on right upper arm. Visual input was used to help the patient be aware of the muscle contraction and the resulted motion. The other hand of the therapist manually contacted the distal part of the transferred muscle flap to apply pressure against muscle contraction and simultaneously call the patient's attention to perceive the direction of the motion. These procedures were aimed for muscle reeducation through integrating all kinds of sensory inputs (e.g. muscle and joint proprioceptors, visual and verbal inputs). These techniques were practiced for 2 weeks.
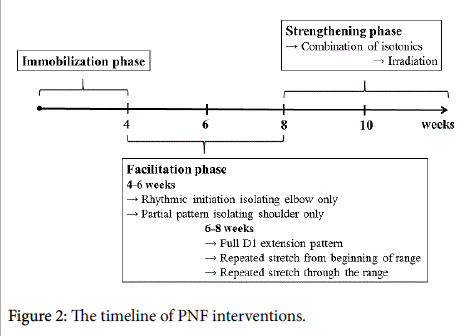
After 2 weeks of LD muscle reeducation to achieve a new role, the patient gained awareness of the transferred LD muscle’s new function. Elbow extension strength began to develop and was assessed as M1. However the patient still could not actively flex his elbow and fingers. The orthosis was removed but was worn for additional 2 weeks at night to maintain the transferred muscle length and tension. During the next few weeks, several PNF techniques including repeated stretch, combination of isotonics and irradiation to activate more elbow and fingers extension were implemented with the full pattern of D1 extension. The timeline of PNF interventions was shown in Figure 2.
The former and new role of the transferred muscle was simultaneously merged into D1 extension pattern to recruit more contraction of the transferred LD muscle. The therapist flexed the elbow and fingers to the end range. Therapist’s one hand applied a quick stretch on the transferred muscle, while the other hand provided quick taps to trigger a stretch reflex, guiding the patient's right upper extremity into D1 extension pattern. The therapist verbally instructed the patient to activate elbow extension through the technique of repeated stretch from the beginning of the range. If the muscle was not strong enough to contract into full extension, gently repeated stretching through the range was integrated. As the transferred muscle had been already immobilized in extension for six weeks, the length of the muscle shortened and the tension was high enough to evoke the stretch reflex.
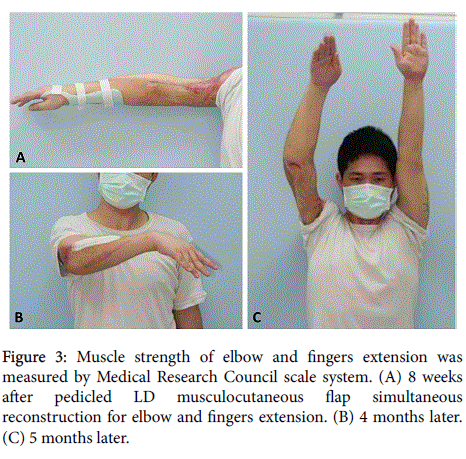
Up to 8 weeks after reconstructive surgery, following the PNF techniques the patient was aware of the contraction of the transferred LD muscle. His elbow and fingers extension showed M3 and M2 muscle strength, respectively (Figure 3A). Furthermore, his shoulder, elbow and fingers flexor spontaneously recovered as M2 muscle strength improved. During this phase, pain was reported as a score of 1/10. The maximum active elbow extension exhibited -30° (extension lag).
Strengthening phase: With recovery of elbow and finger extension, the treatment program moved into strengthening phase. The transferred LD muscle had to operate both elbow and fingers extension. Initially, it was hard for the patient to recruit fingers extension simultaneously with elbow extension. For the purpose of strengthening and improving motor control, the technique of combing isotonics for elbow muscles was integrated into D1 extension pattern. The therapist’s one hand gripped the patient’s upper arm to guide the desired motion. The other hand grasped on dorsal forearm to provide resistance for provoking elbow extension, and the patient instructed to maintain the movement at the end of extension. Then the therapist reversed the grip on volar side contact of forearm and resisted him to flex elbow. The movement was maintained at the end of flexion for few seconds. Because the strength of the transferred muscles and the elbow flexors were not strong enough, resistance was provided and repetitions gradually increased according to patient's maximal muscle strength.
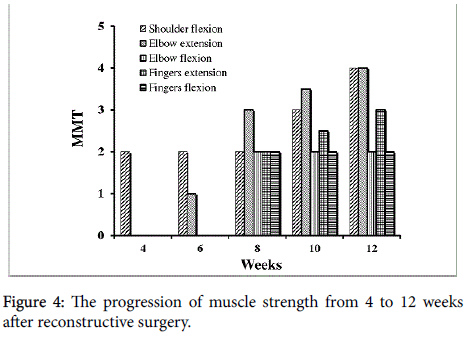
The LD muscle recruited elbow extension easier than finger extension, irradiation techniques using resisted elbow extension was given to facilitate fingers extension. Four months after reconstructive surgery, this patient could elevate shoulder above his head with M4 muscle strength. His elbow and fingers extension reached M4 and M3 muscle strength, respectively. Elbow and fingers flexion were measured as M2 muscle strength (Figures 3B and 3C). Strengthening programs for elbow and fingers muscles continued using thera-band and weights. In addition, daily activities training and participation in activities of daily living with the right upper limb were integrated into all of the treatment programs. Figure 4 illustrates the progressive muscle strength development. During this phase, pain was reported as a score of 0/10. The maximum elbow extension exhibited -20°.
Results
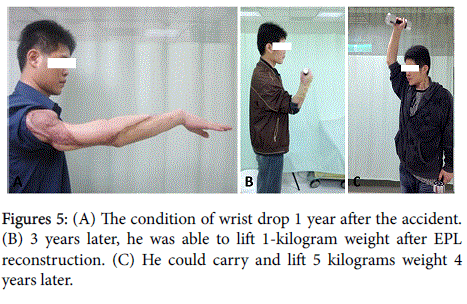
Post injury the patient could not manipulate his right hand due to inadequate finger flexor and wrist drop (Figure 5A). Between the second and third year after the accident, consequential scar release, palmaris longus tendon transfer for the extensor pollicis longus (EPL), muscle lysis, and flexor carpi radialis transfer to extensor carpi radialis longus were performed respectively. In 2 months post follow up surgery, and additional training after the EPL reconstruction, the patient was able to lift 1-kilogram weight (Figure 5B). He returned to his original work as a manufactory worker 2 years after injury. Four years post injury; the patient had acquired satisfactory hand function and could carry up to a 5 kilogram weight (Figure 5C). The Disabilities of the Arm, Shoulder and Hand (DASH) was scored as 29. Total SF-36 score was 57 with physical health scoring 56 and mental health scoring 58.
Discussion
We presented a patient who suffered a high-energy injury at his workplace. For the purpose of reconstructing elbow and hand function, pedicled LD musculocutaneous flap simultaneous reconstruction for elbow and fingers extension was performed. Reconstructions for major upper arm traction avulsion amputation are challenging [4,6,27] and the long-term rehabilitation can pose a frustrating course for patients. Nerve regeneration is slow and physiologically unpredictable at the level proximal to wrist. In this case study, PNF techniques were implemented step by step to facilitate the initiation of motion and the control of the transferred muscle contraction successfully in the early phase after muscle transfer.
Although PNF is a widely used technique in clinical practice, its neurophysiological mechanisms are still unknown. Hindle et al. [28] tried to investigate the possible theoretical mechanisms and concluded that autogenic inhibition, reciprocal inhibition, stress relaxation, and the gate control theory could explain the increase in range of motion, as well as in strength and athletic performance under consistent PNF protocol. According to Shimura and Kasai’s research [29], PNF position improves movement efficiency of the joint by changing the muscle discharge order. These researchers mentioned that peripheral organs such as muscle spindles stimulated by the change of muscle length, and limb position may influence the initiation of voluntary movement. In this case, the stretch reflex of PNF technique was integrated to change elbow or finger extensor muscle length to facilitate motion initiation as the patient perceived transferred muscle contraction and tried to control it. Under this mechanism, it was easy to initiate the motion with the newly transplanted muscle.
Once the transferred muscle could be stretched, and the patient intended to contract the transfer, the D1 extension pattern was used to facilitate the muscle contractions needed to extend the elbow and fingers. The D1 extension pattern is a full upper extremity extension patterns with abduction, medial rotation along with elbow extension and wrist extension, happens to resemble the combinational role of its former and new function of the transferred latissimus dorsi muscle. Henseler et al. [13] explored EMG for LD muscle activation 1 year after transfer for rotator cuff tears. Their study showed transferred LD predominately active in new functional movement as a synergy, but still active in its original antagonistic function with lesser extension. We employed a PNF technique with a partial pattern or full D1 extension pattern to facilitate the new function of the transferred LD through its original function, and successfully developed muscle control 6 weeks postoperatively Irlenbusch et al. [30]. Studied EMG activation after LD transfer and could not detect any finding after 6 weeks. The activation took place 6 months postoperatively and reached higher activity after 12 months. In this current case, the patient and the therapist were aware of LD muscle contractions through PNF interventions 6 weeks postoperatively, with evidence of muscle control documented 8 weeks post muscle transfer (Figure 3A).
The timing of PNF interventions was essential. Once compensatory strategies and motor learning are established, prolonged and overload training might be required for motor improvement. While some motor recovery is a spontaneous process post stroke, PNF is a neurophysiological intervention strategy that stimulates proprioceptors to influence motor outputs of the central nervous system. Reconstructions for major upper arm traction avulsion amputation are difficult and functionally demanding. In this case study, therapists innovatively applied the concepts of PNF early post reconstruction surgery in a patient with a major upper arm traction avulsion amputation with peripheral nerve injury. Application of PNF on this specific surgical condition was unprecedented.
PNF techniques have been recommended for facilitation of neuromuscular control, stability, strength improvement, endurance, coordination, motor control, flexibility (ROM) enhancement, relaxation, and pain release. Application of this technique in this case of a brachial plexus avulsion with surgical reconstruction showed the unprecedented methodology of employing PNF to initiate and provoke learning of a new motion. Based on Adler et al., “rhythmic initiation” and “repeated stretch from the beginning of range” are suggested to achieve the goal of initiate motion. “Rhythmic initiation”, “combination of isotonics”, “repeated stretch from the beginning of range”, “repeated stretch through range” and “replication” are the suggested approaching techniques to learn new motions [31]. Gontijo et al. reported movement pattern of lower limbs could be triggered by irradiation resulting from PNF motions of trunk flexion or extension [32]. In our case, we used the concept of irradiation (also known as overflow) to promote transferred muscle strength and motor function. At the initial stage, we resisted upper limb against medial rotation and extension as the prime movement originally triggered by LD muscle contraction. At the late stage, we resisted elbow extension to facilitate weak finger extension. We found the patient could easily exhibit the desired movement through PNF techniques.
Lin et al. [33] and Schoeller et al. [7] respectively described the primary muscle flap for wound coverage and functional restoration. In the primary stage, they reported satisfactory results. Kawamura et al. described no relationship between free or pedicled LD musculocutaneous flap reconstruction and the functional outcomes [1]. Adkinson et al. also stated distant pedicle flaps are more suitable when recipient vessels are injured or patient-related factors preclude prolonged mircrosurgery [34]. To maximize the rehabilitation outcomes, various reanimation surgeries [4,27] can further challenge therapists to define successful rehabilitation programs. Our patient received a distant pedicled LD musculocutaneous flap in the primary stage. In these flaps, motor nerve reinnervation can be avoided and bypassed compared with secondary free functioning muscle transfers. The results of this case showed that PNF was an intervention effective and also specific to assist and promote the transferred LD in cerebral cortical plasticity after LD musculocutaneous flap transfer.
The Latissimus dorsi is the largest, versatile and reliable flap, which can be used simultaneously as soft tissue coverage and muscle transplantation [34,35]. Even though the length of the LD muscle can be harvest sufficiently, when compared with gracilis or rectus femoris, its excursion is less [5]. To be transferred as elbow and finger extensor simultaneously, its limited excursion makes the muscle strength not powerful enough for wrist extension. In this case, wrist brace and other surgeries were required for correcting wrist drop.
In conclusion, to salvage function following a major arm traction avulsion amputation, a team professionally and specifically skilled in reconstruction and rehabilitation is required. This case report of a traction avulsion amputation of the upper limb, reports the benefit of an early PNF program for rehabilitating function post reconstruction using a pedicled LD musculocutaneous flap. PNF may assist in establishing early awareness of muscle contractions and motor control for new function of a transplanted muscle.
References
- Kawamura K, Yajima H, Tomita Y, Kobata Y, Shigematsu K, et al. (2007) Restoration of elbow function with pedicled latissimus dorsi myocutaneous flap transfer. J Shoulder Elbow Surg 16: 84-90.
- Gulgonen A, Ozer K (2012) Long-term results of major upper extremity replantations. J Hand Surg Eur Vol 37: 225-232.
- Haas F, Hubmer M, Koch H, Scharnagl E (2004) Immediate functional transfer of the latissimus dorsi myocutaneous island flap for reestablishment of elbow flexion in upper arm replantation: two clinical cases. J Trauma 57:1347-1350.
- Lin SH, Chuang DC, Hattori Y, Chen HC (2004) Traumatic major muscle loss in the upper extremity: reconstruction using functioning free muscle transplantation. J Reconstr Microsurg 20: 227-235.
- Chuang DC, Lai JB, Cheng SL, Jain V, Lin CH, et al. (2001) Traction avulsion amputation of the major upper limb: a proposed new classification, guidelines for acute management, and strategies for secondary reconstruction. Plast Reconstr Surg 108: 1624-1638.
- Fufa D, Lin CH, Lin YT, Hsu CC, Chuang CC, et al. (2014) Secondary Reconstructive Surgery Following Major Upper Extremity Replantation. Plast Reconstr Surg 134: 716-720.
- Schoeller T, Wechselberger G, Hussl H, Huemer GM (2007) Functional transposition of the latissimus dorsi muscle for biceps reconstruction after upper arm replantation. J Plast Reconstr Aesthet Surg 60: 755-759.
- Sultana SS, MacDermid JC, Grewal R, Rath S (2013) The effectiveness of early mobilization after tendon transfers in the hand: a systematic review. J Hand Ther 26: 1-20.
- Stevanovic M, Sharpe F (2014) Functional free muscle transfer for upper extremity reconstruction. Plast Reconstr Surg 134: 257e-274e.
- Chen R, Anastakis DJ, Haywood CT, Mikulis DJ, Manktelow RT (2003) Plasticity of the human motor system following muscle reconstruction: a magnetic stimulation and functional magnetic resonance imaging study. Clin Neurophysiol 114: 2434-2446.
- Manktelow RT, Tomat LR, Zuker RM, Chang M (2006) Smile reconstruction in adults with free muscle transfer innervated by the masseter motor nerve: effectiveness and cerebral adaptation. Plast Reconstr Surg 118: 885-899.
- Watanabe Y, Akizuki T, Ozawa T, Yoshimura K, Agawa K, et al. (2009) Dual innervation method using one-stage reconstruction with free latissimus dorsi muscle transfer for re-animation of established facial paralysis: simultaneous reinnervation of the ipsilateral masseter motor nerve and the contralateral facial nerve to improve the quality of smile and emotional facial expressions. J Plast Reconstr Aesthet Surg 62: 1589-1597.
- Henseler JF, Nagels J, Nelissen RG, de Groot JH (2014) Does the latissimus dorsi tendon transfer for massive rotator cuff tears remain active postoperatively and restore active external rotation? J Shoulder Elbow Surg 23: 553-560.
- Plath JE, Seiberl W, Beitzel K, Minzlaff P, Schwirtz A, et al. (2014) Electromyographic activity after latissimus dorsi transfer: testing of coactivation as a simple tool to assess latissimus dorsi motor learning. J Shoulder Elbow Surg 23:1162-1170.
- Dickstein R, Hocherman S, Pillar T, Shaham R (1986) Stroke rehabilitation. Three exercise therapy approaches. Phys Ther 66: 1233-1238.
- Wang RY (1994) Effect of proprioceptive neuromuscular facilitation on the gait of patients with hemiplegia of long and short duration. Phys Ther 74: 1108-1115.
- Ribeiro T, Britto H, Oliveira D, Silva E, Galvao E, et al. (2013) Effects of treadmill training with partial body weight support and the proprioceptive neuromuscular facilitation method on hemiparetic gait: a randomized controlled study. Eur J Phys Rehabil Med 49: 451-461.
- Miyahara Y, Naito H, Ogura Y, Katamoto S, Aoki J (2013) Effects of proprioceptive neuromuscular facilitation stretching and static stretching on maximal voluntary contraction. J Strength Cond Res 27: 195-201.
- Chen CH, Nosaka K, Chen HL, Lin MJ, Tseng KW, et al. (2011) Effects of flexibility training on eccentric exercise-induced muscle damage. Med Sci Sports Exerc 43: 491-500.
- Moyano FR, Valenza MC, Martin LM, Caballero YC, Gonzalez-Jimenez E, et al. (2013) Effectiveness of different exercises and stretching physiotherapy on pain and movement in patellofemoral pain syndrome: a randomized controlled trial. Clin Rehabil 27: 409-417.
- Lee JH, Park SJ, Na SS (2013) The effect of proprioceptive neuromuscular facilitation therapy on pain and function. J Phys Ther Sci 25: 713-716.
- Lee CW, Hwangbo K, Lee IS (2014) The effects of combination patterns of proprioceptive neuromuscular facilitation and ball exercise on pain and muscle activity of chronic low back pain patients. J Phys Ther Sci 26: 93-96.
- Caplan N, Rogers R, Parr MK, Hayes PR (2009) The effect of proprioceptive neuromuscular facilitation and static stretch training on running mechanics. J Strength Cond Res 23: 1175-1180.
- Rubini EC, Souza AC, Mello ML, Bacurau RF, Cabral LF, et al. (2011) Immediate effect of static and proprioceptive neuromuscular facilitation stretching on hip adductor flexibility in female ballet dancers. J Dance Med Sci 15: 177-181.
- Novak CB, von der Heyde RL (2013) Evidence and techniques in rehabilitation following nerve injuries. Hand Clin 29: 383-392.
- Willand MP, Holmes M, Bain JR, de Bruin H, Fahnestock M (2014) Sensory nerve cross-anastomosis and electrical muscle stimulation synergistically enhance functional recovery of chronically denervated muscle. Plast Reconstr Surg. 134: 736e-745e.
- Dafydd H, Lin CH (2014) Hand reanimation. Curr Rev Musculoskelet Med 7: 76-82.
- Hindle KB, Whitcomb TJ, Briggs WO, Hong J (2012) Proprioceptive Neuromuscular Facilitation (PNF): Its Mechanisms and Effects on Range of Motion and Muscular Function. J Hum Kinet 31: 105-113.
- Shimura K, Kasai T (2002) Effects of proprioceptive neuromuscular facilitation on the initiation of voluntary movement and motor evoked potentials in upper limb muscles. Hum Mov Sci 21: 101-113.
- Irlenbusch U, Bernsdorf M, Born S, Gansen HK, Lorenz U (2008) Electromyographic analysis of muscle function after latissimus dorsi tendon transfer. J Shoulder Elbow Surg 17: 492-499.
- Adler SS, Beckers D, Buck M (2008) PNF in Practice: An Illustrated Guide. (3rd edtn), Springer, USA.
- Gontijo LB, Pereira PD, Neves CD, Santos AP, Machado Dde C, et al. (2012) Evaluation of strength and irradiated movement pattern resulting from trunk motions of the proprioceptive neuromuscular facilitation. Rehabil Res Pract 2012: 281937.
- Lin CH, Zhu ZS, Lin CH, Hsu CC, Yeh JT, et al. (2012) Primary free functioning muscle transfer for fingers with accompanying tendon transfer for thumb provide one-stage upper extremity composite reconstruction in acute open wound. J Trauma Acute Care Surg 72: 737-743.
- Adkinson JM, Chung KC2 (2014) Flap reconstruction of the elbow and forearm: a case-based approach. Hand Clin 30: 153-163.
- Wei FC, Mardini S (2009) Flaps and reconstructive surgery. Elsevier Health Sciences, Amsterdam, Netherlands.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 16793
- [From(publication date):
June-2016 - Jul 03, 2025] - Breakdown by view type
- HTML page views : 15520
- PDF downloads : 1273