Research Article Open Access
Promotion of Influenza Prevention Beliefs and Behaviors through Primary School Science Education
Koep TH1,2, Jenkins S3, M Hammerlund ME4, Clemens C1, Fracica E5, Ekker SC4, Enders FT3, Huskins WC6* and Pierret C4*1Clinical and Translational Sciences, Mayo Graduate School, Mayo Clinic, Rochester, MN, USA
2Department of Biology Teaching and Learning, University of MN, St. Paul, MN, USA
3Department of Health Sciences Research, Mayo Clinic, Rochester, MN, USA
4Department of Biochemistry and Molecular Biology, Mayo Clinic, Rochester, MN, USA
5Mayo Medical School, Mayo Clinic, Rochester, MN, USA
6Division of Pediatric Infectious Diseases, Department of Pediatric and Adolescent Medicine, Mayo Clinic, Rochester, MN, USA
- *Corresponding Author:
- Chris Pierret, PhD
Mayo Clinic, Guggenheim 13, 200 ast St. SW, Rochester
MN-55905, USA
Tel: +1 507 773 0814
E-mail: pierret.christopher@mayo.edu
- W. Charles Huskins M.D.,MSc.
Mayo Clinic, 200 1st Street SW, Rochester, MN-55905, USA
Tel: +1 507 255 8464
E-mail: huskins.charles@mayo.edu
Received date: April 27, 2016; Accepted date: June 20, 2016; Published date: June 27, 2016
Citation: Koep TH, Jenkins S, M Hammerlund ME, Clemens C, Fracica E, et al. (2016) Promotion of Influenza Prevention Beliefs and Behaviors through Primary School Science Education. J Community Med Health Educ 6:444. doi:10.4172/2161-0711.1000444
Copyright: © 2016 Koep TH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: School-based campaigns to improve student health have demonstrated short-term success across various health topics. However, evidence of the effectiveness of programs in promoting healthy beliefs and behaviors is limited. We hypothesized that educational curricula teaching the science behind health promotion would increase student knowledge, beliefs and adherence to healthy behaviors, in this case related to influenza.
Methods: Integrated Science Education Outreach is a successful education intervention in Rochester, Minnesota public schools that has demonstrated improvements in student learning. Within this program, we designed novel curricula and assessments to determine if gains in knowledge extended to influenza prevention. Further, we coupled InSciEd Out programming with a clinical intervention, Influenza Prevention Prescription Education (IPPE), to compare students' attitudes, intentions and healthy behaviors utilizing surveys and hand hygiene monitoring equipment.
Results: 95 students participated in (IPPE) in the intervention school. Talking drawings captured improvement in influenza prevention understanding related to hand washing [pre n=17(43%); post n=30(77%)] and vaccination [pre n=2(5%); post n=15(38%)]. Findings from 1024 surveys from 566 students revealed strong baseline understanding and attitudes related to hand washing and cough etiquette (74% or greater positive responses). Automated handhygiene monitoring in school bathrooms and classrooms estimated compliance for both soap (overall median 63%, IQR 38% to 100%) and hand sanitizer use (0.04 to 0.24 uses per student per day) but did not show significant pre/ post IPPE differences.
Conclusions: Student understanding of principles of influenza prevention was reasonably high. Even with this baseline, InSciEd Out and IPPE improved students' unprompted knowledge of behaviors to prevent influenza, as reflected by talking drawings. This novel metric may be more sensitive in capturing knowledge among students than traditional assessment methods. However, IPPE did not produce further significant differences in student attitudes and behaviors regarding the flu.
Keywords
Influenza; Science education; Health behavior; Community health; Child health
Introduction
Background
The 2013 Institute of Medicine (IOM) report evaluating the National Institutes of Health Clinical and Translational Science Awards (CTSAs) called for expanded emphasis on “child health research, community engagement, and training and education” to promote health [1]. Yet, despite the importance of lifelong health habits (e.g., vaccination, proper nutrition and exercise, tobacco avoidance), interventions to promote these habits in young populations are limited. Few studies have fully tested the effect of a health education model integrating science, health, and education [2], and a full evaluation of such a model on disease-incidence outcomes is complicated by the extended natural history of most preventable diseases. Consequently, we need to study the effect of education on surrogate measures of students’ health beliefs and behaviors. The development of robust tools to evaluate changes in students’ health beliefs and behaviors and longterm health outcomes is critical.
Integrated Science Education Outreach (InSciEd Out) is a program shown to improve science proficiency among grade children in Rochester, Minnesota through novel science education strategies and community partnership [3,4]. Recently, InSciEd Out has expanded its mission to test the hypothesis that focusing InSciEd Out’s innovative education methods on unique disease challenges may improve student learning related to health [5]. Complementary to InSciEd Out, Prescription Education refers to the design of clinical interventions to more rigorously test growth in student attitudes, intents, and behaviors related to health promotion resulting from curricula.
As grade schools and children are central to the spread of influenza within communities, K-12 science education focusing on influenza prevention, specifically hygienic behaviors and vaccination, has potential for substantial impact [2,6-8]. Previous interventions that have utilized campaign-style communication to students regarding influenza prevention have demonstrated an effect in reducing influenza infection and absenteeism [9]. However, no study has directly integrated education regarding influenza prevention directly within school curriculum nor described how influenza prevention attitudes, intents, and behaviors change over the course of normal childhood development. Additionally, vaccination is often excluded from instruction, despite being the most effective means for prevention [10,11].
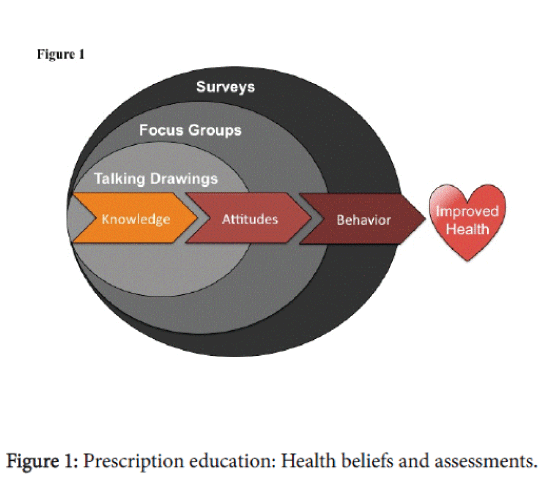
In this study, we tested the effectiveness of InSciEd Out and Influenza Prevention Prescription Education (IPPE), compared to the standard Rochester Public School (RPS) science curriculum, in advancing baseline student influenza prevention understandings, attitudes, and intents supporting healthy behavior choices. A representation of the Prescription Education framework and assessments for each domain are listed in Figure 1.
Methods
InSciEd Out intervention
InSciEd Out is predicated on providing students with active science inquiry opportunities, utilizing zebrafish as a method of engagement and for disease modeling [3]. Zebrafish offer a biological model for learners, encouraging them to ask and answer human biology questions. Initially, teachers participate in a 12-day internship within a research laboratory at Mayo Clinic focused on genetics and development, the nature of science (the ‘‘who’’ and ‘‘how’’ of science), pedagogy, and dialogue, linked by a common disease thread relevant to the school partner (i.e. influenza in this study). Detailed influenza prevention instruction for teachers within this internship included vaccine design and effect, hand hygiene and cough etiquette, germ growth, and immune system functioning. Over the course of the internship and beyond, teachers, education specialists, school administration, and scientists iteratively construct student IPPE curriculum appropriate for respective grade levels. Sustained curricular and technological support is then provided to teachers throughout the school year.
This study describes the design and implementation of IPPE, development and evaluation of novel assessment tools, and early results through 2013-2014 (2 successive school years). Central to our hypothesis is the Health Belief and Integrated Behavioral Model [12-17], where behavioral change is dependent on a foundation of proper disease and prevention understanding and willingness to adopt healthy behaviors.
Study design
The Prescription Education component of the study was a nonrandomized interventional cohort study in an intervention school (∼45 students per grade/year) and a control school (∼80 students per grade/year) in the Rochester Public School (RPS) district (Table 1). The intervention and control school had no previous InSciEd Out affiliation and were selected based upon administrator and teacher willingness to participate. Control school selection was also driven by school diversity, class size, and economic status of students to limit potential convenience sample bias (Table 1). Alternative study designs were also considered, however, randomization of schools was not possible due to requirements for instructional equity and transparent partnerships. Teachers and students in the 3rd and 4th grades (8-10 years old) were chosen due to the alignment of state science standards at these ages with infectious disease topics. Following curricular design through the fall of 2012, 3rd and 4th grade students (Cohort 1 and 2 respectively) participated in 4-6 weeks of IPPE curriculum in the spring of 2013, with Cohort 1 participating a second time as 4th graders in the fall of 2013 (Table 1). The control school received standard RPS curriculum and served as an inter-school control over the course of the study. The study was approved by the Mayo Clinic’s Pediatric and Adolescent Research Committee, Office of Community Engaged Research, and Institutional Review Board with a waiver of informed parental consent in accordance with 45CFR46.116.
| School 1 Intervention | School 2 Control | |||
|---|---|---|---|---|
| Characteristics | Cohort 1 (Grade 3) | Cohort 2 (Grade 4) | (Grade 3) | (Grade 4) |
| Ages | 8-9 | 9-10 | 8-9 | 9-10 |
| Total number of students | n=51 | n=44 | n=78 | n=87 |
| Sex | ||||
| Male | 27 (53%) | 21 (47%) | 44 (56%) | 52 (60%) |
| Female | 24 (47%) | 23 (53%) | 34 (44%) | 35 (40%) |
| Students of Color | 23 (45%) | 26 (59%) | 31 (40%) | 43 (49%) |
| FRPL (Free and Reduced Lunch | 20 (39%) | 23 (53%) | 21 (27%) | 20 (23%) |
| Years Receiving Curriculum | ||||
| Year 1 01/28/2013-3/15/2013) |
Spring 2013 (As 3rd graders) |
Spring 2013 (As 4th graders) |
Did not receive | Did not receive |
| Year 2 08/19/2014-09/26/2014) |
Fall 2014 (As 4th graders) |
Did not receive | Did not receive | Did not receive |
Characteristics of participating schools and student cohorts from the 2013-14 and 2014-15 school years. Individual cohorts were followed for two seasons, with Cohort 1 receiving curriculum in both 3rd and 4th grade.
Table 1: School characteristics and description of intervention timeline.
Description of curricula
The InSciEd Out 3rd grade curriculum was drawn from Minnesota 3rd grade science standards and focused mainly on concepts relating to the process of science, such as how to “generate questions that can be answered when scientific knowledge is combined with knowledge gained from one's own observations or investigations” (Minnesota Academic K-12 Science Standards).
Curricular inquiry activities included hand washing with Glo Germ™ (Glo Germ Company: Moab, Utah), to visualize germ spread and subsequent student-led experiments to assess best hand washing practices. Students also learned about microorganisms and tested ways in which germs collected from the school environment could be killed.
Building upon this 3rd grade foundation, the 4th grade curriculum had 2 clear infectious disease benchmarks: 1.) “To recognize that the body has defense systems against germs, including tears, saliva, skin and blood” and 2.) “To give examples of diseases that can be prevented by vaccination” (Minnesota Academic K-12 Science Standards). One student activity centered on neutrophil chemotactic experiments using zMPO:GFP zebrafish, as described by Dodd et al. [18]. Students visualized immune cells responding to a wound site and investigated the role of unique variables in immune modulation. General InSciEd Out curricula philosophies and development are described by Pierret et al. [3].
Program assessment
Within the greater InSciEd Out program, assessments are used in partner schools to follow gains in student learning related to curricular themes. Talking drawings (TD’s) are one strategy utilized to assess pre/ post intervention changes in student understanding and emerging student language [3,19]. Infectious disease specific TD’s were used in this study in the intervention school with all 4th grade students asked to answer with words and pictures the following question, “What does it mean to be healthy?” Third grade students received a different question related to the nature of science, not relevant to the aims of this study. Word counts and thematic groupings of student answers were compared pre and post curricula, in both year 1 and year 2. Physical copies of TD’s are matched pre/post intervention with unique student identifiers. Unmatched TD’s are discarded from analysis. Analysis of TD’s begins with a text list built by student responses. Common words (the, a, etc.) are removed. Misspelled but phonetically clear words are re-spelled, and phrases are connected as a single text unit, as in “Cover your cough,” to capture the intent of the text. All words used in the TD prompt are removed unless linked in a unique phrase. For example, “healthy” is removed in this analysis but “Eat healthy” is not. Health concepts were chosen prior to TD concept analysis and included: 1.) Even though we can’t see them, germs are everywhere, and they can make us sick. 2.) Our body has natural defenses to fight germs and keep us healthy 3.) We can do certain things to help our body fight illness or keep germs away. After first review it was clear Exercise and Eating healthy were concepts built into the module and were added to concept analysis. Each concept is only counted once per TD and reviewed independently by two team members for concepts and text. A third reviewer compares phrase grouping and concepts and addresses any differences between the initial analyses. Text (including phrases in consensus) is applied to the Worldle® generator at wordle.net and Java applet in Firefox on a Mac to visualize (shifts/change) of pre/post text from all students in a word cloud. The size of the word within the word cloud corresponds directly to the number of times used by students. Concepts are simply tallied and presented in a pre/post format by double column graph in Microsoft Excel.
Study assessment
We applied both traditional and novel assessment tools to assess the effect of the curricular intervention. Traditional methods involved surveys of student self-reported knowledge, attitudes and behavior. As previously described [20], surveys were used to collect student selfreports of knowledge, attitudes, and behavior to identify targets for curriculum revision, and to evaluate the effects of IPPE. No previous child influenza surveys were available to guide survey design, so questions were adapted from previously published adolescent and adult surveys and evaluated for reliability and validity [12,14,17,20]. Surveys spanned multiple domains, including hand hygiene, cough etiquette, and vaccination behavior, and were well understood by all students [20]. Questions were completed on school iPads or desktop computers using REDCap, an online survey tool [21].
In addition to student self-reports, we utilized automated soap and sanitizer dispensers equipped with sensors logging every individual HH event to measure changes pre/post curricula [22]. Dispensers were obtained and installed in all bathrooms and commonly used schoolrooms through an agreement between GOJO® Industries, Inc, Mayo Clinic, and Rochester Public Schools. Sensor data was stored in an online database over 2 consecutive school years between January 2013 and March 2014. Comparisons of HH in intervention and control schools were done pre, during, and post the Year 2 intervention period. Classroom soap and hand sanitizer counts included total dispenses assessed at half hour intervals on school days. To assess impact of the intervention, bathroom soap usage was adjusted for student traffic in and out of the bathroom spaces within Year 1 of the intervention. Infrared sensors monitored total numbers of students entering and leaving and were tied to usage by date/time. Hand sanitizer analysis included all of Year 2 data.
Statistical analysis
Survey questions were categorized a priori into 6 domains guided by the Health Belief Model (HBM) and Integrated Behavioral Models (IBM) [13,16]. Domains were as follows: 1) Knowledge/attitudes about influenza; 2) Knowledge/attitudes about immunization 3) Effectiveness of immunization against influenza; 4) Hand hygiene and cough etiquette; 5) Breaking person-to-person contact (e.g., staying home when sick, avoiding others); and 6) Perceived risk/susceptibility to illness caused by influenza. Responses were dichotomized a priori as a favorable (“correct”) or unfavorable (“incorrect”) response within 5- point Likert scales and Yes/No/Don’t know response types. Don’t know or missing responses were scored as unfavorable responses across all questions. The score is the percentage of items with a favorable response within each domain. Scores from the first and last surveys administered to Cohorts 1 and 2 in the intervention and control school were compared with a paired t-test, and selected individual survey questions (scored as correct vs. incorrect) were compared with McNemar’s test.
The percentage of soap uses per doorway entrance was calculated in half-hour intervals, and “compliance” was calculated in reference to an 80% threshold. This scaled threshold was chosen to account for students crossing the doorway entrance not needing to wash their hands and drawing from student surveys in which 80% was considered a reasonable expected maximum for compliance. This is a conservative scale due to potential student response bias overestimating use. For example, for half-hour intervals during which 80% or more soap uses per doorway entrance was observed, the scaled compliance was set to 100%. Observations that were below 80% were scaled accordingly [example, 60% usage was set to 75%=100*(60/80)]. A classroom hand sanitizer usage rate was calculated from total number of dispenses within each grade and divided by students within each grade. Hand hygiene outcomes (bathroom soap usage scaled compliance, daily classroom sanitizer rate) was then assessed using linear regression with generalized estimating equations to adjust the standard errors for repeated data within each bathroom (or grade) using an exchangeable correlation structure. The independent variables considered were intervention time (pre versus during versus post), grade, sex, and school (intervention versus control). Dates for which there was no school were excluded. All analyses were performed using SAS version 9, and p-values less than 0.05 were considered statistically significant.
Results
Talking drawings
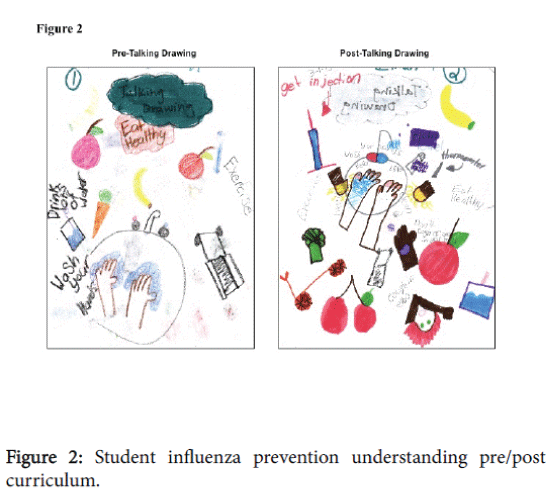
In our partner intervention school, 39 students completed both preand post-TD’s, with 3 TD’s being removed due to either a missing pre- TD or post-TD. A representative pre- and post-intervention TD is depicted in Figure 2.
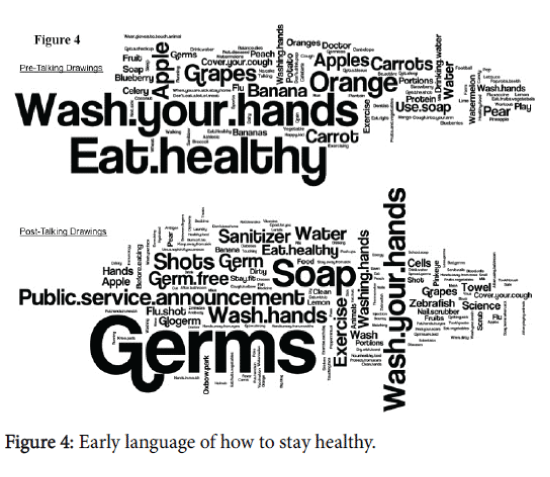
In the pre-intervention TDs, prominent domains included eating healthy (n=29, 74%) and washing hands (n=17, 44%). While these domains were also represented in post-intervention TDs, additional concepts for promoting health emerged. Students more readily identified the immune system (pre n=0, (0%); post n=10 (26%)) and vaccination (pre n=2 (5%); post n=15 (38%)) as a means of staying healthy (Figure 3). Increased word use included “germs”, “soap”, “shots” and “wash your hands”, “washing hands”, and “wash hands”, each related to a concept identified in the intervention curriculum. Post- TD’s also demonstrated emergent language in the use of words such as “antigen,” “antibody,” “vaccine,” “infection,” and “flu shot”. Pictorial representations of these findings are shown in Figure 4.
Representative drawings from a single 4th grade student in Intervention School, Year 1 pre and post-curriculum intervention, in response to the question, “What does is mean to be healthy?”.
Comparison of year 1 pre-curricula and year 1 post-curricula concepts on student talking drawings, where each count represents use on an individual drawing. Concepts were selected prior to the study period from candidate influenza prevention strategies and gradespecific science standards.
Classroom analysis of words and phrases appearing on pre- and post- curriculum talking drawings in 4th grade, Year 1, as depicted in a word cloud. Word size is proportional to frequency of usage, with larger word size correlating to higher frequency of use.
Surveys
A total of 1204 surveys [Intervention School Year 1 (n=254), Year 2 (n=313); Control School Year 1 (n=429), Year 2 (n=208)] were administered to 565 unique students in both the intervention and control school, with an overall response rate of 88% (Intervention School, 87%; Control School, 90%). Among responders in this analysis, 62 (65.2%) students in the intervention school and 108 (64.6%) students in the control school were either in 3rd or 4th grade in year 1 and completed a survey at all offerings. Student self-reports relating to use of HH and cough etiquette in Cohort 1 and 2 in the intervention and control schools were relatively high at baseline across all comparisons.
On average, students scored at least 74% (responded favorably) on knowledge, attitudes, and performance questions relating to hand washing, hand sanitizer use, and covering of cough and sneezes (Table 2). For the question: “After you go to the bathroom, how often do you wash your hands?” 87% of students in School 1 and 91% of students in School 2 reported washing their hands “most times” or “every time.” This did not change between baseline and follow up observations (p=1.0). Trends throughout the study period for all survey domains, unadjusted by grade, are shown in Table 2.
| School 1 (Intervention), n=62 | School 2 (Control), n=108 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Survey Domain | Year 1 Pre | Year 1 Post | Year 2 Pre | Year 2 Post | p value | Year 1 Pre | Year 1 Post | Year 2 Pre | Year 2 Post | p value |
| Knowledge about flu | 41% | 48% | 59% | 56% | 0.0006 | 54% | 51% | -- | 64% | 0.002 |
| Knowledge about flu shot | 68% | 71% | 78% | 75% | 0.23 | 68% | 67% | -- | 76% | 0.01 |
| Hand hygiene, Cough etiquette | 75% | 76% | 77% | 74% | 0.78 | 78% | 74% | -- | 76% | 0.52 |
| Getting flu Shot/Mist | 57% | 63% | 66% | 68% | 0.02 | 65% | 69% | -- | 75% | 0.002 |
| Avoiding sick people | 58% | 55% | 66% | 64% | 0.17 | 73% | 66% | -- | 72% | 0.75 |
| Risk/Susceptibility | 61% | 53% | 60% | 57% | 0.52 | 56% | 55% | -- | 54% | 0.56 |
Of students in each school who completed the survey in all offerings (4 times in school 1, 3 times in School 2), table shows average student score within each survey domain. P-values reflect differences between first and last observation within each school. P-values less than 0.05 considered statistically significant.
Table 2: Influenza prevention understanding and behavior across survey domains.
Table 2 reveals that both student knowledge about the flu and adherence to the flu shot/mist improved significantly over time in both schools (all p values < 0.02). However, these scores continued to lag behind those observed in the HH and cough etiquette domain at baseline. Furthermore, despite greater than 85% of students responding positively to the prompt, “Getting the flu shot/mist is a good idea,” only 74% of 3rd and 4th grade students at both schools said that they received the flu shot “most years” or “every year.” All remaining survey domains did not show any further differences by intervention assignment or over time. Higher HH self-reported compliance by sex was also observed within student surveys at both schools, as 68% of females and 56% of males claimed they washed their hands “every time” after going to the bathroom (data from year 2, post).
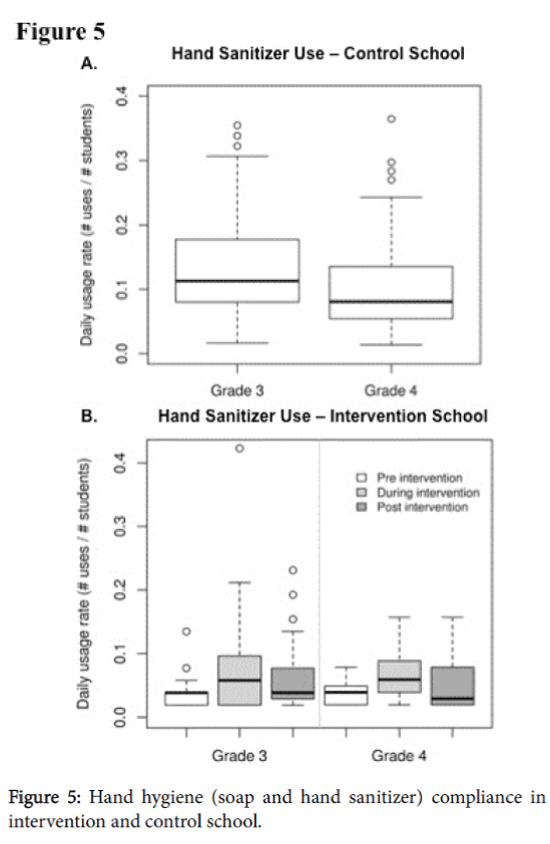
Hand hygiene
Median hand washing compliance across male and female bathrooms in intervention and control schools during a nonintervention month ranged from 45% to 73% (overall median=63%, IQR=38% to 100%). However, the control school had a higher compliance than the intervention schools (median=71% vs. 50%). Furthermore, females at each school had a median compliance nearly 20% higher than males within the same school (Intervention school: 60% vs. 42%; Control school: 79% vs. 63%). Considering the entire time frame, no statistically significant differences in hand soap compliance were seen when comparing the control school to the intervention pre, during, and post intervention in year 2 following adjustments for repeated data. Within classrooms, median classroom hand sanitizer use was low and ranged from 0.04 to 0.24 uses per student per day, with the highest rates observed in grade 3 of the control school (Figure 5A). Although usage appeared to increase slightly in the intervention school pre-intervention to duringintervention (increase from 0.04 to 0.06 in grade 3, 0.04 to 0.06 in grade 4), there was no statistically significant difference in the rate around the time of the intervention, nor was there a significant difference with respect to grade (Figure 5B). Adjustments by school, grade, and sex were also not significant.
Hand sanitizer dispenser data from main hallway entry into all 3rd and 4th grade classrooms at both Intervention and Control Schools. A). August 18, 2013-April 11, 2014 hand sanitizer use in 3rd and 4th grade classrooms; Control school, Year 2 B). August 18, 2013-March 20, 2014 hand sanitizer usage in 3rd and 4th grade classrooms; Intervention school, Year 2. Intervention dates in each grade were non-overlapping and comprised 4-6 weeks within total study interval.
Discussion
We explored the impact of incorporating influenza-centered curricula within an established education reform effort to improve child health knowledge, attitudes, and behavior relating to influenza (Figure 1). To our knowledge, Influenza Prevention Prescription Education (IPPE) represents the first attempt to incorporate themes related to influenza prevention directly within student curriculum. Our study presents a new educational approach to improving student health beliefs and behavior and offers novel influenza prevention outcome measures.
Prescription education measures student changes in knowledge, attitudes, and behavior regarding relevant health topics pre and post curriculum. Various assessments, such as talking drawings, surveys, and focus groups, are utilized to assess different health determinant domains.
Talking drawings (TDs), which have traditionally been restricted to education research settings, were adapted to follow student learning relating to health [19]. At baseline, student reasoning around “how to stay healthy” was generally limited to nutrition and exercise-related disease prevention concepts and language in early years (Figure 3). Unprompted student understanding largely neglected influenzaprevention related activities, as shown on pre-talking drawings (Figures 2-4). Following our IPPE intervention, language and pictorial representations of hand washing, covering of coughs, and vaccination showed improvement (Figures 3 and 4). While promising, it is uncertain whether the knowledge gains demonstrated on TDs represent deep understanding of the preventative strategy listed and how these findings correlate with student attitudes and behaviors.
Overall, the high student survey response rate (Intervention School, 87%; Control School, 90%) was achieved through a waiver of informed consent. The waiver was supported by literature that demonstrated that race was associated with a disparity in the parental response rate when written informed consent was required [23-26]. Importantly, the waiver of consent has been shown to accurately reflect parental wishes [27]. Baseline hand hygiene understanding and performance rated strongest among all domains, while health beliefs relating to the flu shot/mist and breaking person-to-person contact lagged behind (Table 2). Only 74% of 3rd and 4th grade students at both schools said that they received the flu shot “most years” or “every year.” In this version of the intervention, the majority of the 3rd grade curricular content was focused on hand hygiene and covering of cough. These results suggest our curriculum should be revised to more fully capture vaccination as a means of influenza prevention.
Objective measures of hand hygiene (HH), soap and hand sanitizer dispensing, were also piloted in this study for the first time. Historically, school-based studies are not rigorous in following health beliefs underlying behaviors or innovative in the collection of objective outcome measures [10]. Previous studies have attempted to capture HH solely through indirect teacher observations, the validity of which is uncertain [10,28]. As there was no available standardized definition for HH compliance, we developed a methodology for capturing and analyzing student use. Overall, bathroom HH was highly variable across schools, yet, tracking student movement in and out of school restrooms along with dispenser data offers the ability to determine mean values of compliance and observe trends over time. Classroom hand sanitizer use was also quantified as use per student per school day. Overall, classroom use was quite low, with highest median daily use equaling 0.24 uses per student per day (Control School, grade 3, pre-intervention). While increases in sanitizer use were seen during the intervention period, changes were neither significant nor maintained post-intervention (Figure 5B). Low classroom utilization of both soap and hand sanitizer among students may explain the minimal change observed pre/post intervention. Future instruction should prioritize identification of practical opportunities for HH practice and extend beyond the methods and merits of general use. Although objective measures are ideal, installing and supporting automated soap dispensers within public schools may not be feasible in all settings. However, refinement of HH monitoring technology may offer the most reliable way to measure compliance in non-pharmaceutical interventions. Moving forward, future studies should examine student behaviors in relation to overall influenza infection rates in these schools and the greater community.
Authors’ Contributions
THK, SCE, FTE, WCH and CP, and were involved in conception of the study. TK, WCH and FTE contributed to study design. Curriculum constructed by TK, CP, and RPS teachers. TK and CC collected the data. TK, SJ, CC, MEMH, EF, FTE, WCH and CP analyzed and interpreted the data. All authors drafted or critically reviewed the manuscript and approved the final version.
Acknowledgements
The authors would to thank staff and students and Rochester Public Schools for help in data collection. Funding for this study was provided by the Mayo Clinic Department of Adolescent and Pediatric Medicine (DPAM) Individualized Medicine/Community Based Medicine Award and the Center for Clinical and Translation Science (CCaTS): Mayo CTSA Grant Number UL1TR000135 from the National Center for Advancing Translational Sciences. We would also like to acknowledge the help of the Mayo Clinic Survey Research Center and the Research Electronic Data capture (REDCap) team. Additional gratitude is given to GOJO Industries, Inc. for providing automated soap and hand sanitizer dispensers and making detailed data collection possible.
References
- Leshner AI, Terry SF, Schultz AM, Liverman CT (2013) The CTSA Program at NIH: Opportunities for Advancing Clinical and Translational Research. National Academies Press.
- St Leger LH (1999) The opportunities and effectiveness of the health promoting primary school in improving child health—a review of the claims and evidence. Health Educ Res 14: 51-69.
- Pierret C, Sonju JD, Leicester JE, Hoody M, LaBounty TJ, et al. (2012) Improvement in Student Science Proficiency Through InSciEd Out. Zebrafish 9: 155-168.
- Yang J,LaBounty TJ, Ekker SC, Pierret C (2016) Students being and becoming scientists: measured success in a novel science education partnership. Palgrave Communications 2.
- Ekker MP, Nathan GJ, Cao X, Enriquez-Sarano C (2012) Presentations from the 10th International Conference on Zebrafish Development and Genetics, Madison, Wisconsin, June 20–24, 2012. Zebrafish9: 250-255.
- Cauchemez S, Ferguson NM, Wachtel C, Tegnell A, Saour G, et al. (2009) Closure of schools during an influenza pandemic. Lancet Infect Dis 9: 473-481.
- Chao DL, Halloran ME, Longini IM Jr (2010) School opening dates predict pandemic influenza A(H1N1) outbreaks in the United States. J Infect Dis 202: 877-880.
- Viboud C, Boëlle PY, Cauchemez S, Lavenu A, Valleron AJ, et al. (2004) Risk factors of influenza transmission in households. Br J Gen Pract 54: 684-689.
- Stebbins S, Cummings DA, Stark JH, Vukotich C, Mitruka K, et al. (2011) Reduction in the incidence of influenza A but not influenza B associated with use of hand sanitizer and cough hygiene in schools: a randomized controlled trial. Pediatr Infect Dis J 30: 921-926.
- Stebbins S, Stark JH, Vukotich CJ Jr (2010) Compliance with a multilayered nonpharmaceutical intervention in an urban elementary school setting. J Public Health Manag Pract16: 316-324.
- Aledort JE, Lurie N, Wasserman J, Bozzette S (2007) Non-pharmaceutical public health interventions for pandemic influenza: an evaluation of the evidence base. BMC Public Health 7: 208.
- Lindley MC, Wortley PM, Winston CA, Bardenheier BH (2006) The role of attitudes in understanding disparities in adult influenza vaccination. Am J Prev Med 31: 281-285.
- Lau RR, Quadrel MJ, Hartman KA (1990) Development and change of young adults' preventive health beliefs and behavior: influence from parents and peers. J Health Soc Behav 31: 240-259.
- Gellin BG, Maibach EW, Marcuse EK (2000) Do parents understand immunizations? A national telephone survey. Pediatrics 106: 1097-1102.
- Wodi AP, Samy S, Ezeanolue E, Lamour R, Patel R, et al. (2005) Influenza vaccine: immunization rates, knowledge, and attitudes of resident physicians in an urban teaching hospital. Infect Control Hosp Epidemiol 26: 867-873.
- Fishbein M,Ajzen I (1975) Belief, attitude, intention and behavior: An introduction to theory and research.
- Fowler FJ (2009) Survey Research Methods. SAGE Publications.
- Mathias JR, Dodd ME, Walters KB, Rhodes J, Kanki JP, et al. (2007) Live imaging of chronic inflammation caused by mutation of zebrafish Hai1. J Cell Sci 120: 3372-3383.
- Van Meter P, Garner J (2005) The promise and practice of learner-generated drawing: Literature review and synthesis. Educ Psychol Review 17: 285-325.
- Koep TH, Huskins WC, Clemens C, Jenkins S, Pierret C, et al., (2014) Influenza Knowledge, Attitude, and Behavior Survey for Grade School Students: Design and Novel Assessment Methodology. J Community Health 2014: 1231-1240.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, et al. (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42: 377-381.
- Boyce JM (2011) Measuring healthcare worker hand hygiene activity: current practices and emerging technologies. Infect Control Hosp Epidemiol 32: 1016-1028.
- Tigges BB (2003) Parental consent and adolescent risk behavior research. J Nursi Scholarsh 35: 283-289.
- Dent CW, Galaif J, Sussman S, Stacy A, Burton D, et al. (1993) Demographic, psychosocial and behavioral differences in samples of actively and passively consented adolescents. Addict Behav 18: 51-56.
- Fletcher AC, Hunter AG (2003) Strategies for Obtaining Parental Consent to Participate in Research. Family Relations 52: 216-221.
- Kearney KA, Hopkins RH, Mauss AL, Weisheit RA (1983) Sample bias resulting from a requirement for written parental consent. Public Opinion Quarterly 47: 96-102.
- Ellickson PL, Hawes-Dawson J (1989) An assessment of active versus passive methods for obtaining parental consent. Evaluation Review 13: 45-55.
- Stebbins S, Downs JS, Vukotich CJ (2011) The effect of grade on compliance using nonpharmaceutical interventions to reduce influenza in an urban elementary school setting. J Public Health Manag Pract 17: 65-71.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 12542
- [From(publication date):
June-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11591
- PDF downloads : 951