Promoting Vaccination at Birth Using Motivational Interviewing Techniques Improves Vaccine Intention: The PromoVac Strategy
Received: 12-Sep-2018 / Accepted Date: 18-Sep-2018 / Published Date: 21-Sep-2018 DOI: 10.4172/2332-0877.1000379
Keywords: Motivational interviewing; Vaccination intention; Vaccination determinants; Infants; Health promotion interventio
Introduction
Sustained high vaccine coverage (VC) programs have reduced mortality and morbidity by controlling several vaccine-preventable diseases (VPDs) [1]. However, in some areas, VC is suboptimal among infants [2] and clusters of under-immunized individuals have led to community outbreaks of VPDs [1], as has been observed with measles outbreaks in several countries [1,3-5]. Vaccines are delivered through publicly-funded programs in Canada; therefore, restricted access to vaccination services alone cannot explain suboptimal VC. Instead, there are increasing numbers of parents who feel ambivalent toward vaccine effectiveness and safety. Because of the low incidence of VPDs and their complications, for some parents, the fear of vaccine risks now outweighs the fear of VPD complications [6-8]. “Vaccine hesitancy” is described by the World Health Organization as the “delay in acceptance or refusal of vaccines despite availability of vaccine services.” In several studies, up to one-third of parents were vaccinehesitant [9–14]. In a 2011 Canadian survey of 1,745 parents, four in 10 parents reported being more concerned about the safety of vaccines now than they were 5 years ago [15]. Three effective interventions are known to increase vaccination uptake: Parent reminder and recall; multicomponent interventions including education; and vaccination requirements for child care, school, and college attendance [16]. However, no study has reported an effect of education-only interventions on VC improvement. Among the few studies that addressed parental vaccine hesitancy and refusal, no effective strategy was identified [17-19]. Motivational interviewing (MI), a promising tool for health promotion [20], is a patient-centered communication style used to enhance patients’ internal motivation to change by exploring and solving their own ambivalences [21]. Originally developed for substance abuse, MI was also used for behavioral change in several health-related fields [22–24]. This approach is particularly indicated for ambivalent and hesitant clients [25]. MI is based on four principles: 1) expressing empathy toward clients, 2) developing discrepancy between their current and desired behaviors, 3) dealing with resistance without antagonising, preserving effective communication, and allowing clients to explore their views, and 4) supporting self-efficacy (confidence in their ability to change) [25]. MI techniques have been used previously in the area of adult vaccination [26–29]. This study is the first, to our knowledge, to use the MI approach to promote infant and childhood immunization. This study assessed the feasibility and impact of an educational strategy of vaccination promotion at birth, based on MI techniques, on mothers’ intention to vaccinate their infant. We also identified determinants of vaccination intentions among a large population of mothers.
Methods
The methods section adheres to the Transparent Reporting of Evaluations with Non-randomized designs (TREND) statement checklist guidelines [30]. This study was a part of a regional cohort study conducted in the Eastern Townships of Quebec (Canada) to assess the effectiveness of an educational strategy at birth using MI tools. A follow-up of the impact of the intervention on infants’ vaccine coverage will be presented in a forthcoming publication.
Participants
This pre-experimental study with a one-group pretest-post-test design was conducted at the maternity ward of the Centre hospitalier universtaire de Sherbrooke (CHUS), located in the Eastern Townships region (Quebec, Canada). Births at CHUS represent 95% of the total births in the region. During a 1-year period, eligible mothers aged ≥ 18 years, French- or English-speaking, and living in the aforementioned region who gave birth at CHUS were invited to participate in the study. Mothers requiring acute care were excluded, as were mothers of newborns requiring acute care.
Mothers were screened during their postpartum stay at the maternity ward, between 8 AM to 5 PM, in chronological order of delivery. Mothers who delivered first but and had not yet been approached by the research team were screened first. This approach was adopted in order to optimize recruitment given the short mean duration (48 hr) of postpartum maternity ward stays. Mothers who agreed to participate provided written informed consent prior to their participation, as per applicable law.
Intervention
To promote early childhood immunization, we developed a short educational intervention, based on MI techniques, to be delivered to mothers during their postpartum stay. The MI intervention, based on the Quebec Immunization Protocol [31], consisted of five components: 1) Summary of the six VPDs at 2, 4, and 6 months of life; 2) Vaccines administered at 2, 4, and 6 months and their effectiveness; 3) Importance of the routine immunization schedule at 2, 4, and 6 months; 4) Fears and side effects related to vaccination; and 5) Organization of local vaccination services in the Eastern Townships. During the study period, the Quebec routine immunization schedule recommended vaccines at 2, 4, and 6 months to protect against diphtheria, tetanus, poliomyelitis, whooping cough, infections from Haemophilus influenza B and pneumococcus [31].
The intervention content was adapted from two existing theoretical frameworks: 1) The Health Belief Model (HBM) [32] and 2) Transtheoretical model of behavior change [33]. Based on this composite model, each mother’s intention about vaccination was determined and categorized into one of four states of change adapted to vaccination. Overall, this procedure aimed to administer a standardized intervention, adapted to each mother according to her current stage of change regarding vaccination intention. This approach aimed to help each woman progress through the later stages of change at her own pace, ultimately enabling her to self-mobilize toward vaccination on her own.
Pre-intervention measures were collected using a self-administered questionnaire based on the HBM and theory of planned behavior [32,34]. The study intervention was administered to mothers 24–48 hours after delivery, by one of the three clinical research assistants who had received standardized training on the intervention content and MI approach. The intended duration of the intervention was approximately 20 minutes. At the end of the MI session, a second selfadministered questionnaire was administered to mothers. This last questionnaire was collected on discharge from the maternity ward.
Objectives
We hypothesized that an individualized educational information session on immunization using MI tools and delivered during postpartum hospitalization would improve mothers’ vaccination intention and determinants.
Outcomes and data collection
In order to identify a statistically significant increase of 5% in a mother’s intention to vaccinate her infant, taking into account a basic rate of 78% (preliminary data), a risk of alpha error of 0.05 and a power of 80%, we needed to recruit a total of 1046 mothers among the 3000 annual births at the CHUS maternity ward. Descriptive analyses using the χ2 test were computed for all variables included in the preintervention and post-intervention questionnaires for all participants. The main outcome measure i.e. mother’s intention to vaccinate her infant, was dichotomized using an asymmetric split as follows: “Certainly” vs. “Probably,” “Probably not,” and “Certainly not.” Other variables were dichotomized using a symmetric split. For example, “Knowledge of the diseases prevented by vaccine administered at 2, 4, and 6 months of life” was dichotomized as “Not at all” and “Somewhat” vs. “Quite well” and “Very well.” Univariate logistic regression was used to determine which variables as measured pre-intervention were associated with a mother’s intention to vaccinate prior to the intervention. Variables with p<0.1 were included in the multivariate analysis. The final multivariate regression model was used to identify the determinants of vaccination intention. Odds ratios and their respective 95% confidence intervals (CI) were calculated. Finally, nondichotomized answers of the pre-intervention and post-intervention questionnaires were compared, using McNemar’s test to assess the intervention’s effects on these variables. The feasibility of the intervention was measured by the number of mothers who agreed to receive the intervention and that of mothers who received the intervention during their postpartum stay. Statistical analyses were performed using SPSS Version 20.0 (IBM, Armonk, NY, USA) and SAS version 9.3 (SAS Institute Inc., Cary, NC, USA), with statistical significance set at 0.05.
Ethical considerations
This study was duly reviewed and approved by the CHUS Research Ethics Review Board.
Results
Study participants
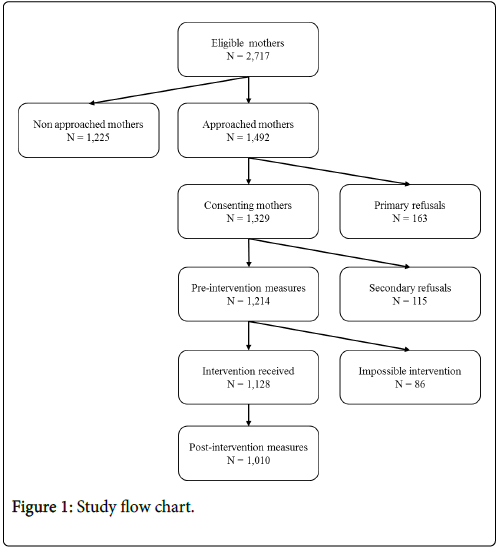
Among the 1492 mothers of newborns approached during the study period (Figure 1), 1329 agreed to participate (89%) and 1214 completed the pre-intervention questionnaire. Some 115 subsequently refused to participate, decreasing the percentage of acceptance to 81.4%. A total of 1201 questionnaires out of 1214 were available to evaluate mothers’ knowledge, beliefs, attitudes and the determinants of vaccination intention.
Overall, 1128 mothers received the study intervention and of these, 1010 (89.5%) completed the post-intervention questionnaire (population study). Among the mothers who completed the preintervention questionnaire, most were married or lived with their partner (88.4%), born in Canada (93.1%), spoke French at home (93.5%), and delivered at 37 weeks gestation or later (95.5%; Table 1).
| Characteristics | n = 1,214 | |
| Age | ||
| <30 years | 732 (60.7) | |
| Highest education level | ||
| Collegial or university | 712 (59.2) | |
| Parity | ||
| At least one another child | 625 (52.1) | |
| Pregnancy length | ||
| ≥ 37 weeks | 1,029 (95.5) | |
| Marital status | ||
| Single | 134 (11.2) | |
| Married/common-partner | 1,057 (88.4) | |
| Divorced/separated | 5 (0.4) | |
| Perception of household income | ||
| As comfortable as other people | 862 (72.4) | |
| More comfortable | 224 (18.8) | |
| Less comfortable | 104 (8.7) | |
| Country of birth | ||
| Canada | 1,091 (93.1) | |
| Home language | ||
| French | 1,128 (93.5) | |
| English | 45 (3.7) | |
| Other | 34 (2.8) | |
Table 1: Demographic characteristics of mothers who completed preintervention measures (*Numbers in parenthesis shows percentages in each group, **Valid percentage was used due to some missing values).
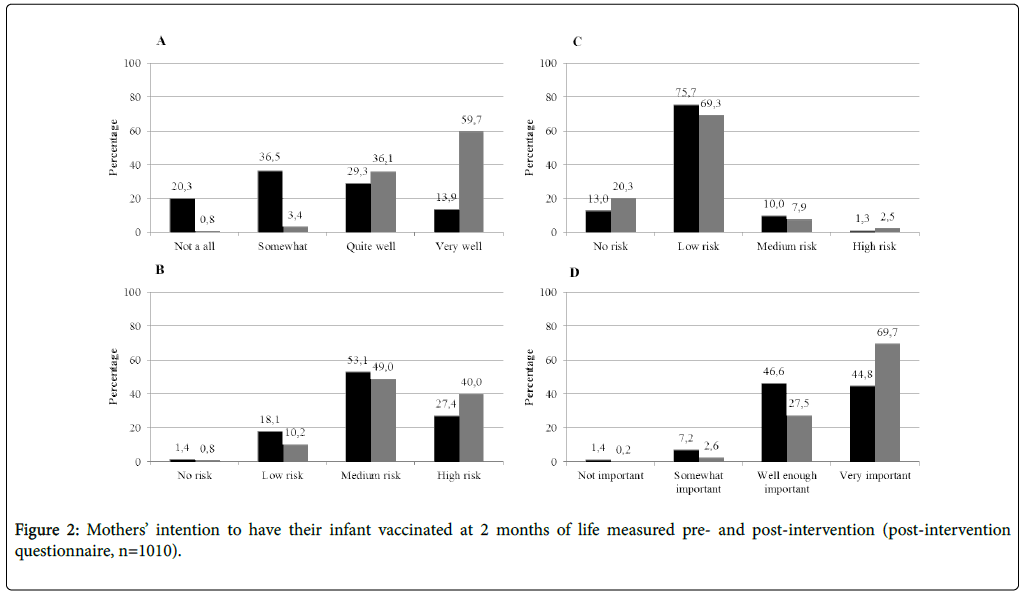
Over 50% of mothers perceived their household income as comfortable (72.4%), were aged under than 30 years (60.7%), had a high education level (59.2%), and already had at least one child (52.1%). Knowledge, beliefs, attitudes, and vaccination intention prior to study intervention (pre-intervention questionnaire, n=1201). Prior to the study intervention, most respondents (874/1201; 72.8%) answered “Certainly” when asked if they intended to vaccinate their infant at 2 months of age (Figure 2). Nearly one-fourth (24.2%) answered “Probably.” The remainder declared that they would “Probably not” (2.4%) or “Certainly not” (0.5%) vaccinate their infant. Those three latter groups could be considered vaccine-hesitant. The self-perceived level of knowledge of the vaccine preventable diseases and vaccines was very low. Only 14.2% of mothers declared having overall knowledge of the diseases preventable by vaccines administered at 2, 4, and 6 months and, except for tetanus, less than 25% had ever heard of these diseases. Another 12.5% of respondents self-rated their knowledge of the vaccines against these diseases as “Quite well” or “Very well”. However, only 44% of mothers declared knowing “Quite well” or “Very well” the importance of vaccinating their infant at 2, 4, and 6 months of age. A proportion of 20% of mothers perceived the risk related to non-vaccination as inexistent or low. Notably, only 37% of respondents perceived vaccines as “very effective”. Accordingly, only half of the mothers considered vaccination of their infant as “very important”. Interestingly, although most respondents declared that health care professionals’ recommendations are important, only 25% had received information about vaccination during pregnancy.
Determinants of intention to vaccinate
In univariate regression analyses, several variables were associated with mothers’ intention to vaccinate their infant at 2 months of age (Table 2).
| Vaccination intention at 2 months | Crude Odds Ratio [95% CI] | p-value | Adjusted Odds Ratio [95% CI] | p-value | ||
|---|---|---|---|---|---|---|
| Factors associated with vaccination intention | “Not certain” | “Certain” | ||||
| n=327 | n=874 | |||||
| Knowledge of the 6 vaccine-preventable diseases | 23/324 (7.1) | 145/861 (16.8) | 2.6 [1.7-4.2] | <.001 | ||
| Knowledge of the vaccines administered at 2, 4 and 6 months | 18/321 (5.6) | 128/845 (15.1) | 3.0 [1.8-5.0] | <.001 | ||
| Knowledge of the importance of vaccinating the infant at 2, 4 and 6 months | 65/323 (20.1) | 454/866 (52.4) | 4.4 [3.2-5.9] | <.001 | 2.8 [1.8-4.2] | <.001 |
| Perception of the susceptibility of contracting a vaccine-preventable diseases (pneumococcus) | 101/309 (32.7) | 407/835 (48.7) | 1.9 [1.5-2.6] | <.001 | ||
| Risk perception of vaccination | 84/323 (26.0) | 62/866 (7.2) | 4.6 [3.2-6.5] | <.001 | 4.5 [2.6-7.8] | <.001 |
| Risk perception of non-vaccination | 206/323 (63.8) | 751/867 (86.6) | 3.7 [2.7-5.0] | <.001 | 2.7 [1.7-4.1] | <.001 |
| Belief in vaccine effectiveness | 295/324 (91.0) | 857/872 (98.3) | 5.6 [3.0-10.6] | <.001 | ||
| Belief of the importance of starting the infant’s vaccination at 2 months | 234/315 (74.3) | 834/852 (97.9) | 16.0 [9.4-27.3] | <.001 | 7.8 [3.7-16.0] | <.001 |
| Information about vaccination received during pregnancy | 57/327 (17.4) | 246/871 (28.2) | 1.9 [1.3-2.6] | <.001 | ||
| Beliefs that health care professionals’ recommendations are important | 214/309 (69.3) | 711/847 (83.9) | 2.3 [1.7-3.1] | <.001 | ||
| Favorable opinion of the spouse in relation to vaccination | 273/318 (85.8) | 845/859 (98.4) | 10.0 [5.4-18.4] | <.001 | 4.7 [1.8-12.1] | .001 |
| Knowledge of where to go to have child immunized | 252/322 (78.3) | 788/868 (90.8) | 2.7 [1.9-3.9] | <.001 | ||
| Knowledge of which health care professionals will take care of child? | 188/318 (59.1) | 604/858 (70.4) | 1.6 [1.3-2.1] | <.001 | ||
| Mother’s age ≥ 30 years | 99/325 (30.5) | 370/870 (42.5) | 1.7 [1.3-2.2] | <.001 | 1.5 [1.0-2.3] | .044 |
| At least one another child in the family | 99/325 (30.5) | 527/865 (60.9) | 3.8 [2.9-5.0] | <.001 | 3.7 [2.5-5.6] | <.001 |
| Family physicians involved in pregnancy follow up care | 117/324 (36.1) | 383/870 (44.0) | 1.4 [1.1-1.8] | .014 | ||
| Midwife involved in pregnancy follow up care | 12/324 (3.7) | 13/870 (1.5) | 0.4 [0.2-0.9] | .018 | ||
Table 2: Determinants of “certain” vaccination intention in univariate and multivariate analyses (pre- intervention questionnaire).
Multivariate analyses were used to identify seven determinants of mothers’ intention to vaccinate. Among them, the most significant correlates of vaccination intention were the belief of the importance of starting infant vaccination at 2 months (OR=7.8; 95% CI: 3.7-16), favorable spousal opinion of vaccination (OR=4.7; 95% CI: 1.8-12.1), risk perception of vaccination (OR=4.5; 95% CI: 2.6-7.8) and already having at least one child in the family (OR=3.7; 95% CI: 2.5-5.6)
Feasibility of intervention
Among the 1214 mothers who had initially agreed to receive the intervention, 1128 did receive it during their postpartum hospitalization, 57 subsequently changed their mind and refused, and another 29 mothers were impossible to reach during their postpartum stay. The feasibility rate of the intervention was 93%.
Intervention’s impact on intention to vaccinate (post intervention questionnaire, n=1010)
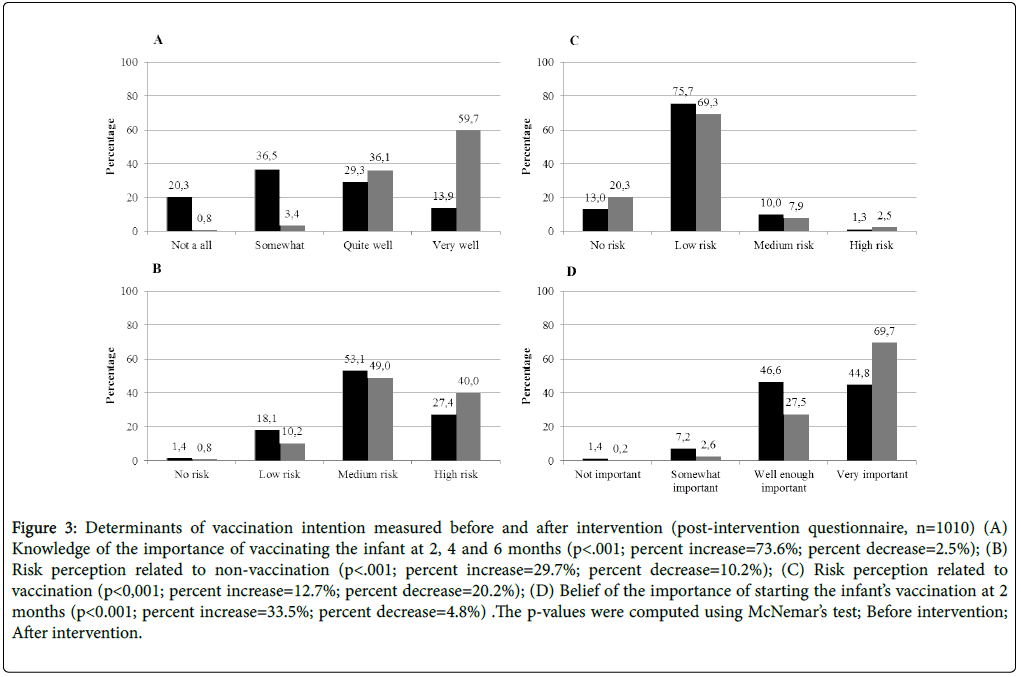
Following the intervention, mothers’ intention to vaccinate their infant at 2 months of age significantly increased from 72.8% to 87.3% (p<0.001; Figure 2). Significant increases were also observed in the main determinants of vaccination intention: Knowledge of the importance of vaccinating infants at 2, 4, and 6 months of age; belief of the importance of starting the infant’s vaccination at 2 months; and perception of the risks related to vaccination, with an overall improvement of 73.6%, 33.5%, and 29.7%, respectively (Figure 3).
Figure 3: Determinants of vaccination intention measured before and after intervention (post-intervention questionnaire, n=1010) (A) Knowledge of the importance of vaccinating the infant at 2, 4 and 6 months (p<.001; percent increase=73.6%; percent decrease=2.5%); (B) Risk perception related to non-vaccination (p<.001; percent increase=29.7%; percent decrease=10.2%); (C) Risk perception related to vaccination (p<0,001; percent increase=12.7%; percent decrease=20.2%); (D) Belief of the importance of starting the infant’s vaccination at 2 months (p<0.001; percent increase=33.5%; percent decrease=4.8%) .The p-values were computed using McNemar’s test; Before intervention; After intervention.
Finally, a significant overall drop (20.2%) was observed in the perception of risks related to vaccination (Figure 3). Additionally, we wondered whether already one child having at least was a significant independent vaccination intention determinant. Therefore, we analyzed the impact of the intervention on study participants who were primiparous mothers i.e. giving birth to their first offspring. In this sub-population of mothers, the study intervention actually drove up mothers’ intention to vaccinate their infant from 60% to 83.3% (p<0.01).
Satisfaction regarding intervention
Among the 1010 mothers who completed the post-intervention questionnaire, most declared having appreciated (“Somewhat agree” and “Agree”) participating in the intervention and declared that they would recommend it to other parents at the maternity ward (>97% for both answers). Additionally, 87.1% of respondents declared that the intervention timing was suitable and 87.5% declared that the intervention’s duration was adequate. Finally, 98.7% declared that they felt that the intervention respected their opinion about vaccination.
Discussion
To our knowledge, this study is the first to demonstrate the efficacy of educational intervention using MI techniques to increase vaccination intention in a population of mothers. Our results revealed that the intervention modifies the determinants of vaccination intention. Pre-intervention measures allowed us to document the knowledge, beliefs, attitudes, and vaccination intentions among a large sample of mothers who participated in this regional study. These measures also enable us to identify which factors influence a mother’s intention to vaccinate her infant. Typically, mothers intended on having their infant vaccinated at 2 months of age and were favorable to vaccines. However, most mothers reported a limited knowledge about VPDs and vaccines at 2, 4, and 6 months; and over 50% of mothers declared not knowing the importance of vaccinating their child at 2 months of age. A Canadian survey of parents also showed various levels of familiarity with infants’ vaccines: 50% reported to be moderately, or not familiar with childhood vaccines [15]. Only one of four mothers declared that they had received information about vaccination during their pregnancy.
As demonstrated in the final multivariate model, the most significant determinants of the intention to vaccinate were not related to knowledge, but to favorable beliefs and attitudes toward vaccination. The belief of the importance of starting infant immunization at 2 months, favorable spousal opinion of vaccination, and risk perception about non-vaccination influenced the intention to vaccinate the most. These results support the fact that new immunization promotion strategies need to move beyond the “knowledge-deficit model” to improve infant VC [35]. Experts agree that a tailored client-centered approach, based on the respect of client-held values, would be more beneficial to resolving parent ambivalence regarding vaccination than providing information to increase parents’ knowledge of vaccination [35,36].
Using an MI approach to promote vaccination intention among the mothers of newborns, the study intervention significantly increased mothers’ intention to vaccinate their infant at 2 months of age. To our knowledge, this shift of nearly 15% is one of the largest reported in the literature [16-19]. The intervention mostly targeted vaccine-hesitant mothers, as Miller and Rollnick showed that MI is effective among ambivalent persons [25]. The major impact was observed in those mothers who previously declared that they “Probably” intended to vaccinate their child. Prior to the study intervention, this group of mothers represented 24.2% of the total study sample, which is relatively similar to that in other studies which quantified the proportion of vaccine-hesitant parents at approximately 33% [9–14]. Following the study intervention, only 11% of mothers declared they “Probably” intended to have their infant vaccinated.
In addition to increasing the intention to vaccinate, the MI session also significantly modified four of its determinants relative to knowledge, as well as beliefs and attitudes about vaccination. This communication style focused on the mother’s concerns regarding the necessity and safety of vaccines rather than on providing information in a directive way. Our results show that the MI approach led mothers to resolve their own ambivalence about vaccination, and to change their perception about vaccination. Trying to convince parents through a lot of information and statistics about vaccination alone can actually compound and increase negative attitudes toward vaccination [37]. Thus, the use of the MI approach may be an effective tool for increasing parents’ intention to vaccinate, and to ultimately help curb vaccine hesitancy. In the field of vaccination, only one other group studied the effects of MI sessions on knowledge of vaccines (against hepatitis A and B viruses) [27]. Those authors observed a significant increase in the knowledge of vaccines [27] but did not report any conclusive results as to vaccination completion [28], probably due to the relatively small sample size and target population composed of adults receiving methadone maintenance treatment. Vaccine hesitancy can also be defined by the acceptance of vaccination, but with reluctance. Our early MI session, delivered at the maternity ward, could also benefit less ambivalent parents to increase their knowledge about vaccines and vaccine-preventable diseases through a clientcentered approach. This study’s short intervention was appreciated by participants. They felt that their opinions about vaccination were respected. The acceptability rate regarding the study intervention was high, as 82% of the mothers initially agreed to receive it. The intervention was performed in 93% of the mothers who agreed to participate, suggesting great feasibility and that the postpartum period and maternity ward, therefore, both seemed highly conducive for the implementation of an effective MI strategy for promoting immunization. A major strength of this study was that the intervention was performed by three different research assistants over the entire recruitment period. This contributed to substantially reducing the potential selection bias inherent to the assistant. Moreover, as 95% of deliveries in the Eastern Townships occur at the CHUS maternity ward, our sample is highly representative of the regional population of mothers of newborns as a whole. However, mothers who gave birth at home or in birthing houses could not be included in the study. These mothers, as well as those who refused to participate in the study, may hold somewhat different opinions about vaccination. Although study questionnaires were anonymous and self-administered, a potential social desirability bias could have affected the internal validity of the study. Mothers could have indicated a more favorable opinion about vaccination because of the hospital setting. However, to control for this bias, research assistants were instructed to leave the room when mothers answered the pre-intervention and post-intervention questionnaires. Our population may also have been affected by a selection bias because parents who refused to participate were perhaps highly vaccine-hesitant. However, the rate of vaccine-hesitant individuals in our study is similar to that reported in the literature [9– 14]. Also, pre-intervention, a mother’s intention to vaccinate was similar whether she belonged to the group who accepted to receive the study intervention, who subsequently refused to receive it, for whom the intervention was not possible. Finally, our findings suggest that a mother’s intention to vaccinate her newborn is a relatively good proxy of the infant’s VC at 2 months. However, our findings must be confirmed in a further study assessing the study intervention’s impact on infant VC at 2, 4, and 6 months of age.
Conclusions
This study revealed that a promotional educational strategy based on the MI approach delivered at a maternity ward significantly increased mothers’ intention to vaccinate their infant and that many of its determinants, including knowledge, beliefs, and attitudes about vaccination, influence vaccination intention. A forthcoming study will assess the intervention’s impact on infant VC to accurately demonstrate the effectiveness of such a promotional strategy.
Acknowledgements
We wish to thank all the mothers who participated in the study. We acknowledge the support of all the nurses and physicians of the CHUS maternity ward.
References
- Andre FE, Booy R, Bock HL, Clemens J, Datta SK, et al. (2008) Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ 86: 140-146.
- Boulianne N, Audet D, Ouakki M, Dubé È, Serres G De, et al. (2015) Enquête sur la couverture vaccinale des enfants de 1 an et 2 ans au Québec en 2014. Quebec.
- An Advisory Committee Statement: Measles and Rubella Elimination Working Group. Guidelines for the prevention and control of measles outbreaks in Canada (2013) CCDR 39(3): 1-52.
- Gagneur A, Pinquier D (2010) Early waning of maternal measles antibodies: Why immunization programs should be adapted over time. Expert Rev Anti Infect Ther 8: 1339-1343.
- Gagneur A, Pinquier D (2010) Spotlight on measles 2010: Timely administration of the first dose of measles vaccine in the context of an ongoing measles outbreak in France. Euro Surveill 15: 19689.
- Hilton S, Petticrew M, Hunt K (2006) “Combined vaccines are like a sudden onslaught to the bodyâ€s immune system’: Parental concerns about vaccine “overload†and “immune-vulnerabilityâ€. Vaccine 24: 4321-4327.
- Janko M (2012) Vaccination: A victim of its own success. Virtual Mentor 14: 3-4.
- MacDonald NE (2015) Vaccine hesitancy: Definition, scope and determinants. Vaccine 33: 4161-4164.
- Ritvo P, Wilson K, Willms D, Upshur R, Goldman A, et al. (2005) Vaccines in the public eye. Nat Med 11:S20-S24.
- Lagarde F (2005)Â Summary of public opinion on immunization in Canada.
- Sauvageau C, Duval B, Gilca V, Lavoie F, Ouakki M (2007) Human papilloma virus vaccine and cervical cancer screening acceptability among adults in Quebec, Canada. BMC Public Health 7: 304.
- Smith A, Yarwood J, Salisbury DM (2007) Tracking mothers’ attitudes to MMR immunisation 1996-2006. Vaccine 25: 3996-4002.
- Zimet GD, Liddon N, Rosenthal SL, Lazcano-Ponce E, Allen B (2006) Chapter 24: Psychosocial aspects of vaccine acceptability. Vaccine 24: 201-209.
- Fabry P, Gagneur A, Pasquier J-C (2011) Determinants of A (H1N1) vaccination: Cross-sectional study in a population of pregnant women in Quebec. Vaccine 29: 1824-1829.
- Ekos Research Associates Inc (2011) survey of parents on key issues related to immunization.
- Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, et al. (2000) Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med 18: 97-140.
- Sadaf A, Richards JL, Glanz J, Salmon DA, Omer SB (2013) A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine 31: 4293-304.
- Dubé E, Gagnon D, MacDonald NE (2015) Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 33: 4191-203
- Kaufman J, Ryan R, Walsh L, Horey D, Leask J, et al. (2018) Face-to-face interventions for informing or educating parents about early childhood vaccination. Cochrane Database Syst Rev 5: CD010038.
- Appiah-Brempong E, Okyere P, Owusu-Addo E, Cross R (2014) Motivational interviewing interventions and alcohol abuse among college students: a systematic review. Am J Health Promot 29: e32-42.
- Rollnick S, Miller WR, Butler CC (2008) Motivation interviewing in health care: Helping patients change behavior.
- Hettema J, Steele J, Miller WR (2005) Motivational interviewing. Annu Rev Clin Psychol 1: 91-111.
- Rubak S, Sandbaek A, Lauritzen T, Christensen B (2005) Motivational interviewing: A systematic review and meta-analysis. Br J Gen Pract 55: 305–12.
- Britt E, Hudson SM, Blampied NM (2004) Motivational interviewing in health settings: A review. Patient Educ Couns 53: 147-55.
- Miller WR, Rollnick S (2002) Motivational interviewing: Preparing people for change. 2nd ed. New York.
- Venne S, Trudeau GL (2009) entretien motivationnel, un vaccin contre la résistance du patient Le Médecin Du Québec 44: 33-7.
- Nyamathi A, Tyler D, Sinha K, Marfisee M, Cohen A, et al. (2010) Predictors of hepatitis knowledge improvement among methadone-maintained clients enrolled in a hepatitis intervention program. J Community Health 35: 423-432.
- Nyamathi A, Sinha K, Greengold B, Cohen A, Marfisee M (2010) Predictors of HAV/HBV vaccination completion among methadone maintenance clients. Res Nurs Health 33: 120-132.
- Brackett A, Butler M, Chapman L (2015) Using motivational interviewing in the community pharmacy to increase adult immunization readiness: A pilot evaluation. J Am Pharm Assoc (2003) 55: 182–186.
- Des Jarlais DC, Lyles C, Crepaz N, TREND Group (2004) Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health 94: 361-366.
- Ministère de la Santé et des Services sociaux. Protocole d’immunisation du Québec. Mise à jour 2014.
- Rosentock I (1974) Historical origins of the health belief model. Heal Educ Behav 2: 328-335.
- Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: Toward an integrative model of change. J Consult Clin Psychol 51: 390-395.
- Ajzen I (1991) The theory of planned behavior. Org Behavior Human Dec Proc 50: 179- 211.
- Dubé E, MacDonald NE (2016) Addressing vaccine hesitancy and refusal in Canada. CMAJ 188: E17-E18.
- Witteman HO (2015) Addressing Vaccine Hesitancy with Values. Pediatrics 136: 215-217.
- Nyhan B, Reifler J, Richey S, Freed GL (2014) Effective messages in vaccine promotion: A randomized trial. Pediatrics 133: e835-e842.
Citation: Gagneur A, Lemaître T, Gosselin V, Farrands A, Carrier N, et al. (2018) Promoting Vaccination at Birth Using Motivational Interviewing Techniques Improves Vaccine Intention: The PromoVac Strategy . J Infect Dis Ther 6: 379. DOI: 10.4172/2332-0877.1000379
Copyright: © 2018 Gagneur A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6787
- [From(publication date): 0-2018 - Nov 13, 2025]
- Breakdown by view type
- HTML page views: 5724
- PDF downloads: 1063